 Click to Print Adobe PDF
Click to Print Adobe PDF
Winter 2013 - Vol.8, No.4
|
Transjugular Intrahepatic Portosystemic Shunt (TIPS): A Clinical and Procedural Review
Mark R. Werley, M.D.
Lancaster Radiology Associates
John Briguglio, M.D.
Division Chief, Vascular and Interventional Radiology, Lancaster Radiology Associates
|
  |
INTRODUCTION
This article reviews clinical and procedural information relating to placement of a transjugular intrahepatic portosystemic shunt (TIPS) in patients with symptomatic portal hypertension.i
Portal hypertension is a frequently encountered cause of morbidity and mortality in the general population. The most common cause is cirrhosis resulting from ethanol abuse or viral hepatitis, although there is a rising incidence of patients with non-alcoholic steatohepatitis (NASH) associated with type II diabetes mellitus and obesity. Cirrhotic changes within the liver parenchyma increase microvascular resistance within the hepatic portal triads and elevate portal pressure. Portal hypertension can also result from severe right atrial hypertension or hepatic veno-occlusive disease (Budd-Chiari syndrome).
Elevated portal pressures cause multiple clinical manifestations, some of which can be life-threatening. In an attempt to reduce portal pressure, the body will attempt to shunt the portal blood to the systemic system via portosystemic collaterals. These occur most often at anastomoses within the gastrointestinal system, such as between the esophageal and intrathoracic veins, between the gastric/splenic veins and the left renal vein, or between the rectal and hemorrhoidal veins. The umbilical vein can also become recanalized. Portal hypertension can also result in increased vessel permeability and ascites. Accompanying shifts in volume can also lead to diminished cardiac and renal function, also known as the hepato-renal syndrome.
Varices within the esophagus and stomach are at increased risk for hemorrhage due to their thin walls combined with increased intraluminal pressure. When these varices rupture they can rapidly lead to exsanguination, and are a major cause of mortality in cirrhotic patients. Ascites and the hepato-renal syndrome are also leading causes of morbidity in patients with portal hypertension. They often lead to complications and additional costs related to procedures such as dialysis and repeated paracentesis.
Early attempts to control portal hypertension involved surgical creation of shunts between the portal and systemic system, but these procedures had high mortality rates and the shunts had limited long-term patency. The first successful placement of portosystemic shunts via the percutaneous approach was performed in 1982 by Colapinto et al., and the first stented TIPS was created in 1988 by Richter et al.1 This procedure is now considered a standard treatment for portal hypertension in the appropriate setting.
PREPROCEDURE EVALUATION AND PREPARATION:
In any patient with portal hypertension, TIPS can be used in control of a life-threatening complication, as a bridge to eventual hepatic transplant, or as a palliative measure. TIPS is not currently indicated as the primary treatment for acute variceal bleeding. Though there is debate about absolute and relative indications for TIPS, acute variceal bleeding refractory to medical/endoscopic management and refractory ascites are the most commonly accepted and treated indications. Other indications include non-esophageal gastrointestinal varices, Budd-Chiari syndrome, and hepatic hydrothorax. TIPS has also shown potential for treatment of hepatorenal syndrome.
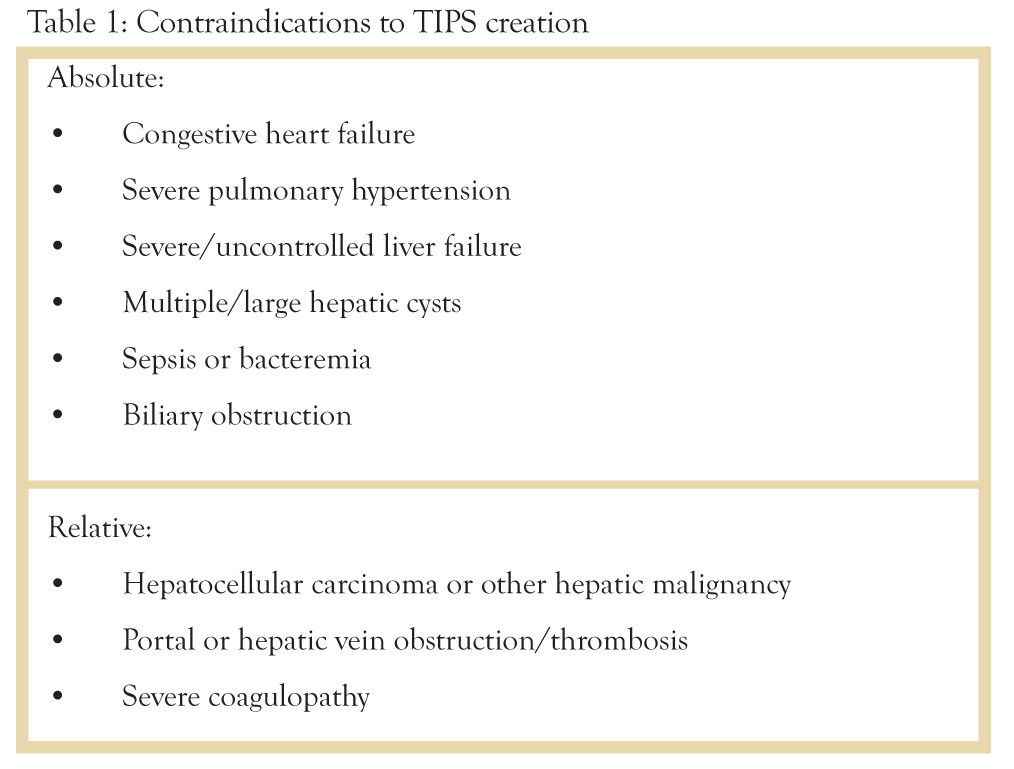
Multiple absolute and relative contraindications to TIPS creation exist (Table 1).2 The degree of impairment of liver function may serve as an absolute or relative contraindication. Many of the relative contraindications reflect increased intraprocedural risk for complication or technical challenges. Attempts have been made to correlate clinical scoring and staging systems with preprocedure risk and mortality. The authors currently use the MELD (Model for End-stage Liver Disease) scoring system to assess preoperative risk, which uses a logarithmic model that accounts for serum bilirubin, serum creatinine, and INR (international normalized ratio) and has been shown to be comparable to other scoring systems such as the Child-Pugh score for stratifying risk prior to TIPS3. A MELD score of greater than 18 is indicative of a 40% survival rate post-TIPS, compared with 90% for a MELD score of 18 or less. In another study, MELD scores of 25 or greater were associated with 3, 6, and 12 month mortalities of 42%, 65.5%, and 74.2% respectively. The same study showed no deaths at 3 months in patients with a MELD score of 10 or less.
Preprocedure planning should involve discussion with the patient’s hepatologist as well as discussion of risks and benefits with patients and their families. In addition to procedural risks such as severe bleeding or death, long-term risks such as encephalopathy should also be discussed. A pre-procedure hepatic ultrasound is typically ordered to assess patency and flow of the portal and hepatic veins; occlusion of these veins will not prevent TIPS placement, but will make placement substantially more challenging. Cardiac consultation and echocardiography is also typically performed to evaluate for right heart failure. Cross-sectional imaging is useful for planning of shunt orientation and location. Placement is typically performed with general anesthesia to reduce patient discomfort and movement during an extended procedure. Coagulation parameters should be optimized to a platelet count greater than 50,000 and an INR less than or equal to 1.7. Consideration of renal function should also be made, as the placement procedure typically utilizes at least 60 cc of iodinated contrast.
PROCEDURE
Initial access is established using the right internal jugular vein, and a wire is passed into the inferior vena cava. A sheath is passed into the heart and a right atrial pressure is measured. Elevated right atrial pressure (greater than 10 mmHg) is an absolute contraindication to TIPS placement and will result in termination of the procedure. A catheter and wire are then placed through the sheath into the right hepatic vein. An occlusive balloon catheter is then used to measure both a free hepatic vein pressure and a “wedged” pressure with the balloon inflated, which approximates portal pressure.
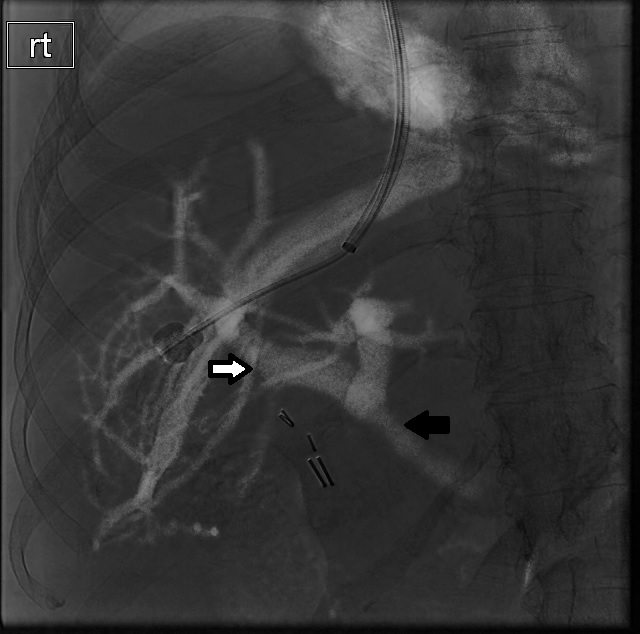
Prior to placement of the shunt, fluoroscopic guidance is most commonly used to target the portal system, though multiple other methods have been described. Fluoroscopic guidance can be performed by directly accessing the portal system percutaneously, with injection of contrast material or placement of markers, or it can be performed via the hepatic vein, typically with carbon dioxide, which rapidly diffuses into the portal system and acts as a negative contrast agent. Injection is performed via the inflated balloon catheter within the right hepatic vein, yielding a limited venogram of the portal system (Figure 1).
Figure 1: Wedged portal venogram performed using carbon dioxide as a negative contrast agent. A balloon catheter has been inflated in the right hepatic vein. Forceful injection of carbon dioxide opacifies the right portal vein (white arrow) and main portal vein (black arrow).
Several needle kits are currently available for portal vein access, the most commonly used being the Colapinto or Rosch-Uchida kits (Cook Incorporated, Bloomington, IN, USA).4 The authors typically use the Rosch-Uchida kit, which is has a smaller gauge access needle. A stiff curved metal cannula is passed into the hepatic vein via the sheath, which is used to direct the needle. The expected location of the right portal vein is anterior and slightly inferior to the right hepatic vein. Access is ideally achieved between the central portion of the right hepatic vein and the peripheral right portal vein, although access can be successfully be achieved between the middle hepatic and right portal vein as well as the left hepatic and left portal veins. Achieving portal vein access is by far the most technically challenging portion of the procedure, and can take several hours. Non-target structures are commonly traversed as there is limited control of the needle after it leaves the metal cannula.
Once access to the portal vein is secured, a catheter is passed into the portal vein and portal venous pressure is measured. If the portosystemic gradient (the difference between portal and systemic pressures) is less than 12 mmHg, then TIPS placement is not indicated. If the gradient is high enough, contrast is then injected through the catheter to evaluate portal vein anatomy and to determine the final length of the shunt (Figure 2). All TIPS procedures are performed with stents, to reduce contraction and thrombosis of the shunt path. The tract across the liver is first dilated with an angioplasty balloon, followed by deployment of the stent across the tract. Following stent placement a repeat contrast injection is performed to confirm direction of flow; there is often a dramatic reduction in flow into collateral vessels (Figure 3). Repeat portal and systemic pressures are then measured; the goal is a portosystemic gradient of less than 8 mmHg. If the desired gradient is not reached the stent may be dilated again with a balloon, or in severe cases a second TIPS can be placed.
Figure 2: Portal venogram performed following transhepatic access to the portal vein and prior to TIPS creation. A catheter has been passed through the liver and portal vein (white arrow) and into the splenic vein. Large esophageal varices are seen filling via the cardiac vein (black arrow)
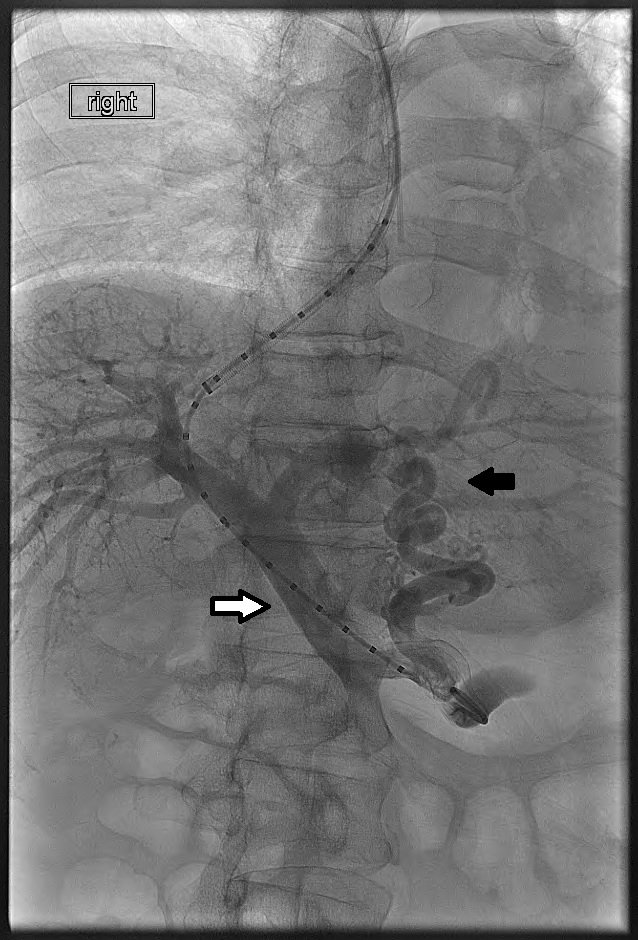
Figure 3: Digital subtraction venogram performed following TIPS creation in the patient shown in figure 2. There has been placement of a 10 mm diameter Viatorr stent (white arrow), extending from the portal vein to the right atrium (black arrow). Note that the previously visualized esophageal varices are no longer opacified.

For many years TIPS procedures were performed with bare metal Wallstent endoprostheses (Boston Scientific, Natick, MA, USA), but recent studies have demonstrated superiority of the Viatorr partially covered stent (WS Gore, Flagstaff, AZ, USA). Primary patency rates with the Viatorr stent at 3, 6, and 12 months were 94%, 67%, and 38% respectively, compared with 63%, 48%, and 24% for bare metal stents.5 Secondary patency rates were also higher for the covered stent group. The Viatorr stent consists of a 2 cm bare metal stent which protrudes into the portal vein, and a variable length ePTFE covered stent portion which extends from the portal vein to the hepatic vein-IVC junction.
POST-PROCEDURE MANAGEMENT
All patients undergoing TIPS placement should be admitted to a telemetry unit for at least one night. Hemodynamic shifts with increased right heart pressures and decompensated hepatic function may require intensive care monitoring. Most elective patients are able to leave the hospital within 1-2 days. Prior to leaving the hospital or within 7-10 days of TIPS placement, it is recommended that the patient undergo a routine Doppler ultrasound examination of the liver as a baseline for future monitoring. TIPS performed with placement of a Viatorr stent cannot be evaluated with ultrasound immediately after placement, as a small amount of air remains trapped in the ePTFE stent lining. This interferes with ultrasound transmission and will give the appearance of stent thrombosis.
Surveillance ultrasound of the TIPS should be performed at 3-6 months and every 6 months afterward, as well as anytime that symptoms of portal hypertension recur. Angiographic study is indicated if flow velocities are less than 80 cm/s or greater than 180 cm/s, or if in-stent velocity changes more than 50 cm/s compared with the previous study. The large majority of TIPS failures result from intimal hyperplasia at the venous end of the stent resulting in flow restriction and eventual thrombosis. This can be reduced by covering the entirety of the shunt from the portal vein to the IVC with the covered portion of the Viatorr stent. Revision of a TIPS may require thrombolysis, angioplasty, and possibly placement of a new stent.
COMPLICATIONS
Complications can be intra-procedural or post-procedural (Table 2).2,4Procedural complications are almost entirely related to passage of the entry needle through the liver at an unintended location,4 and can be minimized with careful technique. Extra-hepatic punctures and punctures of the bile ducts and hepatic arteries occur frequently but rarely result in severe complications. Severe injuries of the biliary system or hepatic arteries can be managed with biliary diversion or embolization. Puncture of the gallbladder is infrequent but can result in cholecystitis or biliary peritonitis. The most severe complications arise from poor stent placement. If the portal vein is punctured near the bifurcation of the main portal vein, the entry site will be extrahepatic, and balloon dilation of the high-pressure extrahepatic portal vein could result in rapid exanguination.

Post-procedure complications are more common but often less severe. Patients with underlying cardiac disease may experience transient heart failure from rapid shunting of mesenteric blood to the right atrium. This is almost always successfully managed medically with diuretics and optimization of cardiac output. The most common complication, a direct consequence of bypassing the liver, is worsening hepatic encephalopathy, occurring in anywhere from 10-40% of TIPS patients. Naturally, the greatest risk is in patients with baseline encephalopathy prior to shunt placement. In most patients this problem can be controlled with medical management such as lactulose or oral antibiotics. Worsening hepatic function can also occur. Refractory hepatic failure and encephalopathy that fail all medical therapy will often require endovascular narrowing of the existing TIPS, or possibly occlusion of the shunt. These methods are a last resort however, as portal hypertension and accompanying clinical findings will rapidly recur. TIPS stenosis and failure are a common delayed complication, however with appropriate technique in placement and monitoring this is becoming less common.
FUTURE DEVELOPMENTS:
Covered stents have revolutionized the procedure of TIPS placement and significantly improved long term patency. Studies have shown that patients with hepatocellular carcinoma can successfully receive TIPS as a palliative measure or as a bridge to transplant, and interventional oncology procedures such as chemoembolization have been shown to be safe in TIPS patients. New guidance techniques for portal vein localization such as percutaneous ultrasound or intravascular ultrasound (IVUS) have been successful in TIPS placement. Improvements in angiography suites now allow for cone-beam CT to be performed on the angiography table to aid in three-dimensional guidance. A similar procedure also exists to place an endovascular shunt between the portal vein and IVC via the caudate lobe, called a direct intrahepatic portosystemic shunt (DIPS), but this approach is limited to highly experienced operators. Overall, TIPS remains an essential procedure for management of portal hypertension, with new techniques and equipment resulting in decreased procedure time and improved long-term outcomes.
TIPS at LGH
We have recently begun to offer TIPS at Lancaster General Hospital, and we have had technically successful TIPS placement in 2 of 3 patients in whom the procedure was attempted. Both successful placements resulted in improvement of clinical symptoms, and none of the three patients experienced any major complications.
REFERENCES
1. Haskal, ZJ. Percutaneous Mangement of Portal Hypertension. In: Baum S, Pentecost M, eds. Abrams’ Angiography: Interventional Radiology. 2nd ed. Philadelphia, PA: Lippincott, Williams, and Wilkins; 2006: 581-600.
2. Boyer TD and Haskal ZJ. American Association for the Study of Liver Disease Practice Guideline: The Role of Transjugular Intrahepatic Portosystemic Shunt Creation in the Management of Portal Hypertension. JVIR 2005; 16(5): 615-628.
3. Ferral H and Patel NH. Selection Critera for Patients Undergoing Transjugular Intrahepatic Portosytemic Shunt Procedures: Current Status. JVIR 2005; 16(4): 449-455.
4. Haskal, ZJ. Transjugular Intrahepatic Portosystemic Shunts. In: Kandarpa K, Machan L, eds. Handbook of Interventional Radiologic Procedures. 4th ed. Philadelphia, PA: Lippincott, Williams, and Wilkins; 2010: 390-397.
5. Jung HS et al. TIPS: Comparison of Shunt Patency and Clinical Outcomes between Bare Stents and Expanded Polytetrafluoroethylene Stent-Grafts. JVIR 2009; 20(2): 180-185.