
Fall 2013 - Vol. 8, No. 3
Concussion in American Football and Sports
Jon E. Bentz, Ph.D.
Neuropsychology Specialists
INTRODUCTION
A little more than a century ago, football was on the verge of being banished. Deaths on the gridiron occurred almost weekly during the football season; there were 18 in 1904 and 19 in 1905. Numerous colleges, including Northwestern, Columbia, and Duke dropped football in 1906 due to its violence and dangers. If it were not for President Teddy Roosevelt’s efforts to broker a plan that revamped the game’s rules and lessened the sport’s inherent violence, football might have disappeared (see fig.1).
Fig. 1. President Teddy Roosevelt brokered a change in football rules to lessen it’s inherent violence.
Today, concern is again arising about the violence and dangers that are part of the game. The primary impetus behind this concern comes from the growing body of evidence that concussions cause a risk in later life of persistent cognitive impairment, dementia, and depression. Retired professional football players have initiated a number of pending lawsuits. Even ESPN, whose success is at least partially dependent upon football, has raised concern regarding the incidence and management of concussions, and has suggested that rule changes may be needed to reduce the frequency of brain injury. Responding to these concerns, even President Obama entered the discussion. During a January 2013 interview published in The New Republic magazine, he encouraged the NCAA to explore options that would reduce the incidence of concussion among football players.
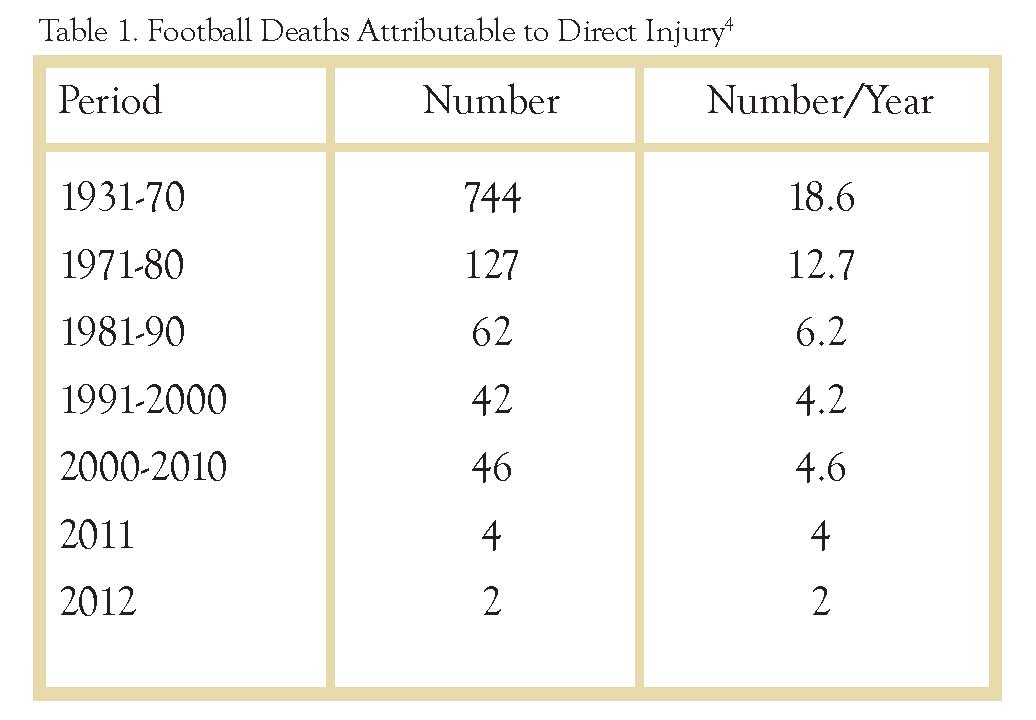
THE SAD STATISTICS
Up until the past decade, the primary focus on scientific studies on football related brain injuries and prevention have focused on more serious traumatic brain injuries such as intracranial and intracerebral bleeds. An article in the December 6, 1931 New York Times reported 40 football related deaths during that season and a total of 275 football related deaths between the years 1906-1931.1 Since 1931, The National Center for Catastrophic Sport Injury has tracked sports related injuries. Their data indicate a reduction in the total number of deaths directly attributable to football. But while the number of deaths related to playing football—which are primarily due to brain and spinal cord injuries—has been reduced dramatically, the incidence of concussion has not. The Centers for Disease Control estimates that sports-related concussions in the U.S. occur at a rate of 1.6-3.8 million/year. Of these, concussion in high school athletes is estimated to account for 300,000/year,2 with football accounting for an estimated 67,000/year.3 This statistic converts into an average of one concussion in every American football game.
Over the years the nature of the game has change dramatically. Tackling has progressed from wrapping arms around the ball carrier and dragging him to the turf to impacting and knocking the ball carrier to the ground. Players are bigger, stronger, and faster than 50 years ago. The Laws of Physics being what they are, the impact forces in collisions must be greater today than in the past, which translate into greater acceleration/deceleration of the head and an increased risk of concussion.
We now have the capability to evaluate the linear and rotational forces to the head resulting from impact. Small accelerometers embedded in helmets can measure the g- forces that players’ heads experience upon impact, in addition to the directional force and the location of the impact zone on the head. Studies indicate that a football hit can easily exert (for milliseconds) a force of 50g. Hits greater than 100g are common, and forces as high as 168g have been recorded. For comparison sake, g-forces of fighter jets are generally at a maximum of about 9-12g and in car crash tests at 25mph, crash dummies hit windshields at 100g. The amount of force that can cause a concussion is variable. Studies at the University of North Carolina demonstrated that some players sustain concussions at forces slightly over 60g while other players who sustained hits at greater than 90g showed no signs of concussion.4>
POST CONCUSSION SYNDROME
The possibility of persistent symptoms following concussion has been recognized for many years. The term post concussion syndrome, referring to persistent symptoms including headache, irritability, memory problems, and dizziness was first coined in 1934.5 Individuals experiencing concussion related symptoms 3 weeks beyond the initial injury meet the generally accepted criteria for a diagnosis of post concussion syndrome. Studies have reported that a significant number of patients sustaining concussion (as high as 60%) experience post concussion symptoms after one month and as high as 15% still report symptoms after one year.6 It is well established that children and teens, and especially younger girls are at greater risk of sustaining concussion and post concussion syndrome than adults. The lingering symptoms manifesting in post concussion syndrome are attributed to metabolic changes that occur with concussion. While the National Football League initially downplayed the significance of concussion and the possibility of persistence of symptoms, it has now been established that football players in particular, due to the number of head hits sustained and risk of multiple mild concussive injuries during a season and in a career, are at elevated risk of suffering from post concussion syndrome.7
CHRONIC TRAUMATIC ENCEPHALOPATHY
Roughly beginning in the 1990s, there has been considerable research on the morbidity of concussion in sports. It is now accepted that individuals sustaining multiple concussions are at an increased risk of a subsequent concussion and chronicity and severity of symptoms. Of major concern is the evidence suggesting that football players, with the number of head hits suffered, are at increased risk of developing neurodegenerative disorders manifested in dementia and mood and behavioral disorders.
In 1928, “dementia pugilistica” was described in boxers. This constellation of Parkinsonian and dementia like symptoms included the presence of impaired motor skills, altered mental status, speech impairment and tremors. Now referred to as chronic traumatic encephalopathy (CTE), this neuro-degenerative disorder is attributed to repeated concussive and subconcussive injuries. CTE, with its association with repeated brain trauma is a preventable dementia. Though principally associated with athletes in contact sports (e.g. American football, professional wrestling, professional hockey, boxing, soccer), it has also been identified in a victim of physical abuse, a patient with epilepsy, a self injurer, and a circus clown who was repeatedly shot from a cannon. The symptoms of CTE are not simply attributable to protracted post-concussion syndrome,8 but occur later in life, often years after the suspected trauma.
While the clinical symptoms are often similar to those occurring in individuals with Alzheimer’s disease or frontotemporal lobar degeneration, the neuropathology is distinctly different.9 There are currently 49 neuro-pathologically confirmed cases in the literature. Postmortem neuro-pathological findings include excessive accumulations of hyperphosphorylated tau and TDP-43 proteins in the brain that disrupt normal brain function, but there is a relative absence of the senile amyloid plaques seen in Alzheimer’s disease. Other findings include atrophy of the hippocampus and other medial temporal structures (especially the amygdala), and the orbital frontal regions of the brain.
Early neuropsychological and neuropsychiatric symptoms typically fall into one of 3 domains: cognitive (memory impairment, executive function deficit); mood (depression, apathy, irritability, suicidal tendency); and behavior (impulse control problems, disinhibition, substance abuse and other addictions, aggression, and increased violence). Neurological symptoms often involve difficulty with gait and balance, and slowed or dysarthric speech.10 The Center for the Study of Traumatic Encephalopathy at Boston University reports cognitive symptoms in 69%, mood and behavioral disturbances in 65%, and motor disorders in 41% of those diagnosed with CTE.
HOW MANY AND HOW MUCH IS TOO MUCH?
There are insufficient research and data pertaining to who is at greater risk for developing chronic neurobehavioral impairment or CTE. The number, severity, or cumulative extent of head traumas necessary to cause CTE is not clear. That said, there is a relationship between CTE and increased exposure to head hits in football, soccer, boxing, and horse racing. While a history of repetitive brain trauma has been documented in all cases of CTE, other risk factors may be involved. Age has considered a factor, with the belief that injuries in younger individuals may lead to greater risk of CTE, but this has not been clearly validated. Genetics may contribute to risk with studies reflecting increased incidence of the APOE-e4 allele among those developing CTE. ApoE protein production increases following brain injury and has been theorized to impact neuronal repair.11 However, at this time, there are no definitively identified factors for greater risk of developing CTE.
When is the brain truly concussed? What about subconcussive injury?
The American Academy of Neurology defines concussion as a traumatically induced alteration in mental status caused by a direct or indirect blow to the head. Thus, concussion has traditionally been diagnosed based on symptoms, which assumes a functional and not a structural injury. But with the accumulation of evidence that athletes who sustain multiple concussions are at greater risk for dementia or major depression later in life,12 there is increased concern about the potential cumulative effect of blows to the head that do not result in observable concussive symptoms.
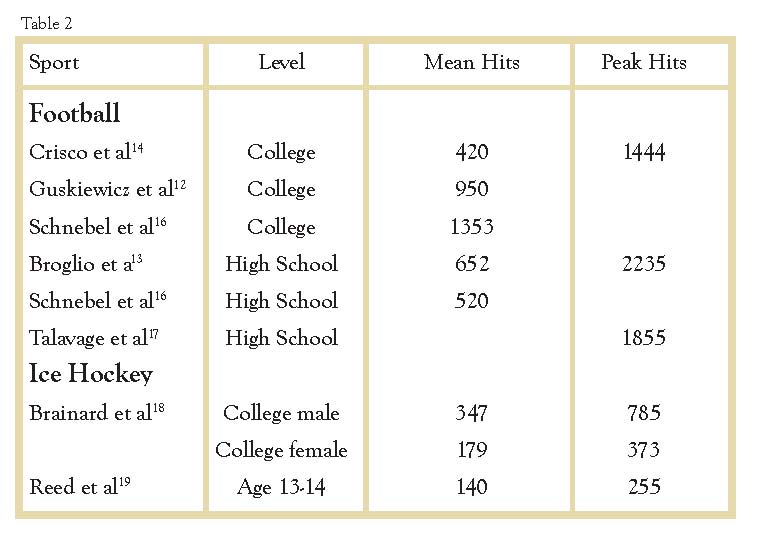
In many sports, particularly football, a player may sustain hundreds of hits in the course of a season. Using helmet accelerometers in a study of high school football, players sustained approximately 652 head impacts during a 14-week season.13 Linemen experienced the greatest number of impacts per season (868), followed by tight ends, running backs, linebackers (619), quarterbacks (467), and receivers and defensive backs (372). The cumulative effect of multiple blows that often do not cause concussive symptoms has become a major area of concern. The Crisco et al14 study involved 3 NCAA football teams and revealed that the median number of head impacts on each team was 4.8, 7.5, and 6.6 impacts per practice and 12.1, 14.6, and 16.3 impacts per game. Linemen and linebackers had the largest number of impacts per practice and per game.
While the vast majority of these hits do not result in clinically identifiable concussions, the cumulative effects of these “nonconcussive” events may potentially alter brain integrity. Diffusion tensor imaging (DTI) studies have detected differences in white matter integrity among high school football players sustaining subconcussive head hits.20 Other studies using functional MRI (fMRI) have identified altered neurophysiologic function, as well as impairment on neuropsychological testing (primarily visual working memory), among high school players who experienced higher numbers of subconcussive hits.12 Long-term longitudinal studies are necessary to clarify the persistence and long-term morbidity of these subconcussive events.
When has the concussed brain fully recovered?
Standard protocol following concussion emphasizes that following concussion it is important for the individual to have considerable rest and not to overexert mentally or physically. Activities that cause exacerbation of symptoms are to be avoided. With resolution of symptoms, a graduated approach toward re-engagement in usual activities is prescribed. Athletes should never return to sports-related activities or play until they are symptom-free and fully recovered. Determination of full recovery is typically based on clinical examination and neuropsychological testing, but research on subconcussive injuries raises doubts that this standard protocol assures “complete recovery.” There may be no observable clinical symptoms, but has the brain thoroughly recovered? Greater access to quantitative functional neuroimaging would appear to be a promising future tool to identify an individual’s readiness to return to play, academics, work, and other everyday activities.
Are helmets the answer or the problem?
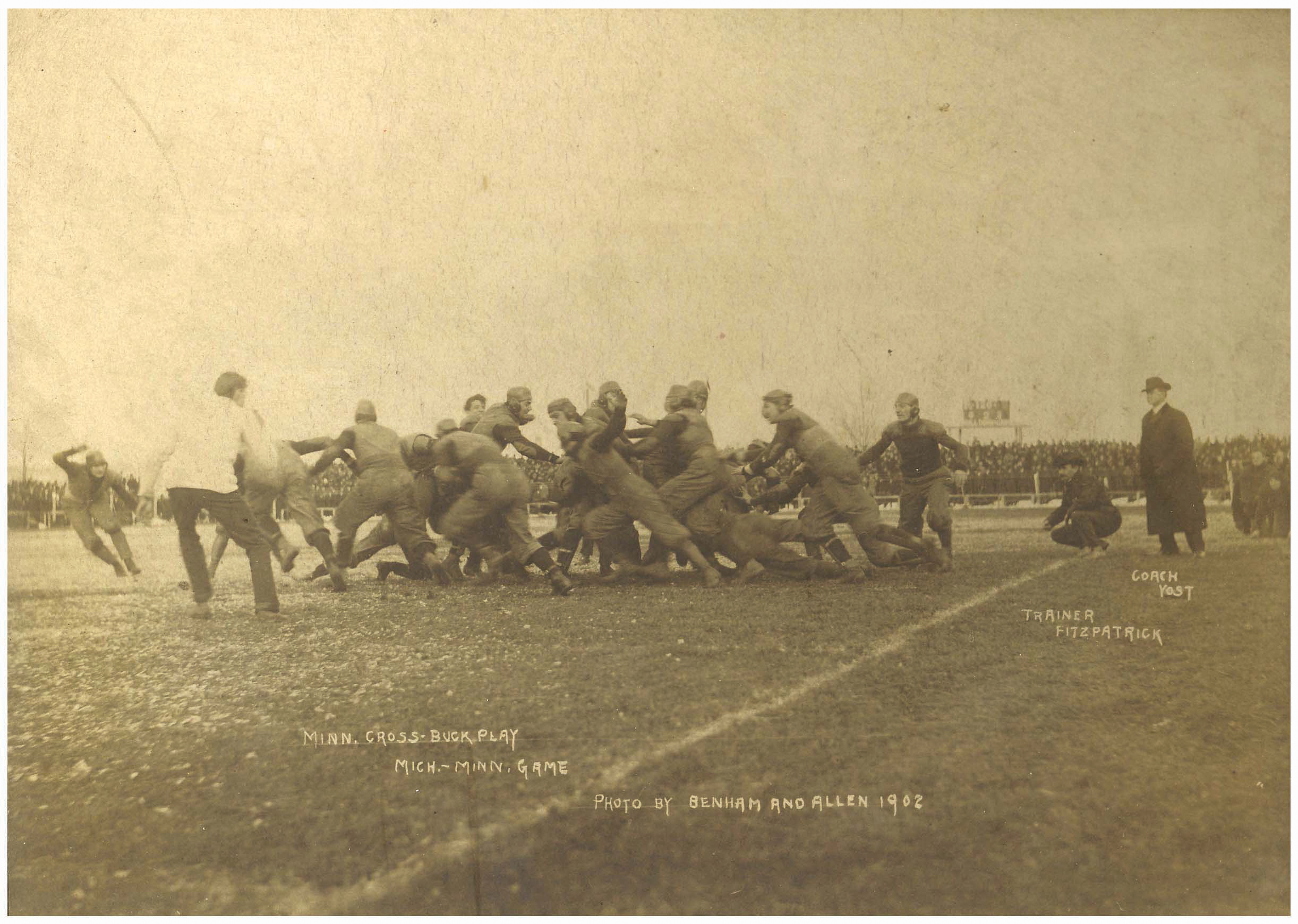
1893 marked the first use of protective leather headgear in a football game (fig.2). Helmets did not become mandatory in the National Football League until 1940.21 There is much debate as to whether head gear is protective or might actually contribute to the problem by facilitating tackles that lead with the head. In a study of collegiate football players, 20% of head hits were associated with impacts to the top of the head. Players with impacts to the top of the head were 3X more likely to experience impact forces of >80g compared with impacts to the front, back, or side of the helmet, and there was a suggestion of a greater likelihood of concussion with blows to the top or front of the helmet.22
Fig. 2. Protective leather headgear in use in 1902.
On contact the head is subjected to linear and rotational forces; the former are more likely to result in skull fractures and intracranial bleeds, while the latter appear to account for the majority of concussions. Helmets do serve a protective function in reducing linear forces, and the advent of padded hard-shell helmets has dramatically reduced and virtually eliminated the incidence of skull fractures and intracranial bleeds. In the middle of the 20th century, as many as 30 football players per year died annually due to head injuries, but there have been no identified skull fractures in the NFL since the 1980s. It has been estimated that newer helmet design has reduced the incidence of concussion by 10-20%.23 But as noted, improvements in protective equipment may have created a false sense of safety.
Fig. 3. Equipment manufacturers turn to new technology to reduce the incidence of concussion by 10-20%.

What does appear to be clear, based on input from helmet manufacturers and biomechanists studying helmets, is that development of a concussion-proof helmet is unlikely. The minimal amount of padding inside a helmet’s outer shell would have to decelerate a player’s head slowly enough to prevent significant injury. One expert on helmet design noted that “In a car crash, you stop in a matter of feet. In an NFL impact, you stop in inches.” The goal in designing helmets is to extend the duration of the impact in the range of hundredths of a second. University of Nebraska physics professor Dr. Timothy Gay believes that football helmets are “85 percent as good as they’re ever going to get,” and a concussion-proof helmet would need 15 inches of foam rubber on the outside of the helmet.
Still, the design of helmets has received considerable attention, and there have been significant improvements that appear to decrease the risk of concussion. Dr. Stefan Duma at the Virginia Tech Center for Injury Biomechanics studies and releases an annual rating system of the protective benefits of various football helmet models. Future research and ratings are also planned for hockey, baseball, softball, and lacrosse helmets.
Should children be playing contact sports?
The greatest number of concussions occurs in children. Research indicates that children are more vulnerable to concussions and have more protracted recovery than adults. Approximately one-half of the emergency room visits for concussions in America are children aged 14 and under. A 2011 study by The Centers for Disease Control and Prevention revealed a 60 percent increase in emergency department visits among children for suspected concussion between the years 2001-09. Concern regarding concussion in younger children is in part associated with the uncertainty of the effects of injury on the developing brain, especially the maturation of white matter. Furthermore, the risk of catastrophic injury in cases of second impact syndrome warrants increased concern in children.
Robert Cantu, M.D., a leading researcher of concussion and author of Concussions and Our Kids, suggests restricting children less than 14 years of age from playing tackle football, body checking in ice hockey, and heading in soccer. His approach is certainly controversial given the number of children playing contact sports without suffering any known significant consequences. While engagement in sports-related activities certainly carries risk, there are numerous positives that come from participation in sports and team play. These include acquiring the benefits of: exercise, a sense of belonging, increased self-confidence, and the principles of team work.
EVALUATION AND TREATMENT OF INDIVIDUALS FOLLOWING CONCUSSION
The Veterans Administration/Department of Defense has issued evidence-based recommendations in the form of clinical practice guidelines regarding management of concussion/mild traumatic brain injury. They emphasize early education of patients regarding concussion and recommend that intervention should include:
- Provision of information and education regarding concussion symptoms and recovery;
- Normalization of symptoms;
- Reassurance of expected positive outcome;
- Awareness of limitations;
- Self-monitoring of symptoms;
- Empowering the patient for self-management;
- Strategies for prevention of further injury;
- Importance of an implementation of sleep hygiene principles;
- Limiting use of caffeine/tobacco/alcohol;
- Program for initiation of graduated exercise in mental activities;
- Monitoring of progressive return to normal activities.
Standard practice continues to prescribe rest and avoidance of physical and mental exertion following injury. Typical guidelines suggest 2-5 days of nearly complete rest following a concussion, as exertion may exacerbate symptoms or delay recovery. Education regarding proper concussion management including rest, adequate nutritional and fluid intake, and stress management is also indicated.
When the patient is free of symptoms, an individualized plan of graduated return to physical and mental activities should be prescribed, with progressive increases in duration and intensity of activity as long as symptoms aren't exacerbated. That determination should be made on the basis of monitoring by health care professionals using tools that include symptom checklists, neurological examinations, and cognitive assessments.
- Any suspicion of concussion should result in immediate discontinuation of play.
- There should be no return to sports-related activities unless the individual is symptom free.
- High school age or younger individuals with concussion should be managed more conservativelythan older athletes regarding return to play.
- Accommodations may be necessary for either academic or work-related activities.
There are no medications specific to the treatment of concussion or post-concussion disorder. Symptom-specific medications have been used with variable effectiveness in the treatment of attention deficit, fatigue, headache, dizziness, vertigo, nausea, mood disorder, and sleep disturbance.
Physical and occupational therapy and vision therapy treatments have become more common for the treatment of post-concussion symptoms. Evaluation and treatment is often beneficial in the attenuation of vestibular symptoms such as dizziness, vertigo, and problems with balance. Post-concussion headaches may be the result of myofascial or cervical injuries, temporo-mandibular joint injury or muscle activity of the superior trapezius and semispinalis capitis muscles in the suboccipital region. Core and neck strengthening programs can reduce vulnerability to these consequences of concussion.
RETIREMENT FROM PLAY
There are no definitive guidelines that mandate retirement from play. Some athletes are at particular risk and it is especially important to counsel patients about the potential consequences of repeated head trauma and the risk factors for neurobehavioral or cognitive impairment to those individuals:
- with multiple concussive events;
- experiencing concussions with increasing frequency across shorter duration of time;
- suffering concussions with lesser intensity of blows;
- experiencing progressively longer recovery following injury;
- reporting or evidencing subjective or objective persistent neurobehavioral impairment;
- CT or MRI evidence of structural injury;
- Non-resolving functional imaging deficit.
WHAT CAN BE DONE TO REDUCE THE RISK OF CONCUSSIONS IN ATHLETICS?
1. First and foremost, education of the medical community is necessary to enhance identification and management of concussion, along with public education for coaches, players and parents. To date, 47 of the 50 states and the District of Columbia have passed student-athlete concussion laws that require education of coaches and players about concussion, and establish guidelines for return to play.
2. While education and awareness of the significance of concussion has improved, survey data from athletes suggest that many continue to underreport their symptoms. A paper presented at the 2012 American Academy of Pediatrics’ annual meeting reported that high schools with athletic trainers identified concussions at a much higher rate than schools without athletic trainers,24 which implied that athletic trainers are more reliable at identifying symptoms of concussion.
3. The greater the time that athletes spend engaged in contact sports, the greater their risk for brain injury. Since the number of head hits received during a season and throughout a lifetime is a major concern, a reasonable first step is decreasing the number of full contact practices. This means restricting full contact football, heading the ball in soccer, or checking in hockey. Noncontact practice during off-season would also significantly decrease the number of head hits. The NFL has restricted the number of full contact practices to only 14 times during its 18 week season. In 2011, Ivy League football limited contact during practices to 2 sessions per week, and in 2012, Pop Warner Football limited contact in practices to 3 hours per week. More schools are using concussion screening programs to compare players’ brain function after a hit to baseline measurements taken pre-season.
4. With the use of accelerometers in helmets to measure linear and rotational acceleration forces of the head, data have been gathered to establish thresholds for impact forces that could potentially serve as guidelines or cut-off scores for removal of players from play. Whether guidelines for removal from play should be based on cumulative g-forces over a specified duration of time, or solely on a single hit, will need further study. Much as Little League Baseball™ has limited the number of pitches a player may throw in a game or over a defined time, it should be possible to monitor the number or intensity of head hits and acceleration forces that a player experiences. These could serve as criteria to immediately remove a player from the game for evaluation and treatment.
5. Core strengthening and neck strengthening programs are beneficial in decreasing head acceleration associated with head impact.
6. Proper selection and wearing of head gear is of paramount importance as there is research that suggests a difference in concussion risk between various models of helmets. The Virginia Tech Star Helmet Ratings provide guidance on football helmets with ratings as: not recommended, marginal, adequate, good, very good, and best.
7. There are numerous claims that the use of mouth guards can reduce the risk of concussion, but the research on this issue has not been particularly extensive or positive. Studies of NCAA basketball players25 and football players26 and South African rugby players27 have failed to demonstrate any reduction in the incidence of concussion injuries. The only possibly encouraging study was a 1967 report of reduced intracranial pressure in cadavers exposed to blunt head trauma.28
8. Proper coaching, skills training, and rule changes can also reduce the risk of head injury. USA Football, the official youth football development partner of the NFL, has emphasized training of coaches and players in proper (“heads up”) tackling and fitting of equipment. After the National Center for Catastrophic Sport Injury reported an average of 19.7 deaths directly related to football in the 10 years from 1967-1976, rule changes were made that penalized leading with the helmet while blocking or tackling, and coaches began teaching tackling with the shoulder while keeping the head up. In the following 10 years football-related deaths from spinal cord or brain injuries dropped to 7.9 per year. In 2011, the NFL moved the kickoff line forward, resulting in fewer kick-off returns. This change resulted in a reduction in concussions/year from an average of 26.3 between 2008-2010 to 15 in 2011.
THE FUTURE
Reduction in the risk of the long-term sequelae of multiple concussive injuries requires expanded understanding of both concussion and sub-concussion injury. Longitudinal studies should increase our understanding of the brain’s capacity to endure injury, and guide earlier counseling of athletes. Developments in clinical and radiological technology offer hope of earlier detection of those injuries that have consequences later in life, thus reducing morbidity and mortality. While repetitive brain trauma is necessary for CTE to develop, it is not a sufficient cause alone. We need further investigation and identification of other factors that escalate the risk of CTE.
Finally, it is assumed that greater diligence in immediately identifying potential concussion and sub-concussion injuries in real time (game time) through the use of helmet accelerometers, would provide improved protection. Other potential benefits may come from the development of early interventions to manage brain inflammation and modulate metabolic disturbances following concussion.
REFERENCES
1. 40 Players killed in football season. New York Times. December 6, 1931.
2. Marar M, McIlvain NM, Fields SK, Comstock RD. Epidemiology of concussions among United States high school athletes in 20 sports. American Journal of Sports Medicine. 2012;40(4):747-755.
3. Broglio SP, Sosnoff JJ, Shin S, He X, Alcaraz C and Zimmerman J. Head Impacts during high school football: a biomechanical assessment. J. Athletic Training. 2009;44:342-349.
4. Mueller FO, Colgate B. Annual survey of football injury research. The National Center for Catastrophic Sport Injury. 2013.
5. Strauss I, Savitsky n. Head injury: neurologic and psychiatric aspects. Archives of Neurology and Psychiatry. 1934;31:893-955.
6. Bazarian JJ, Wong T, Harris M, Leahey N, Mookerjee S, Dombovy M. Epidemiology and predictors of post-concussive syndrome after minor head injury in an emergency population. Brain Injury. 1999;13:173-179.
7. Bailes JE, Cantu RC. Head injury in athletes. Neurosurgery. 2001;48(26):26-46.
8. Gavett BE, Cantu RC, Shenton M, Lin AP Nowinski CJ, McKee, Stern RA. Clinical appraisal of chronic traumatic encephalopathy: current perspectives and future directions. Current Opinion in Neurology. 2011;24(6):525-531.
9. McKee AC, Cantu RC, Nowinski CH, Hedley-Whyte ET, Gavett BE, Budson AE et al. Chronic traumatic encephalopathy in athletes: progressive tauopathy after repetitive head injury. Journal of Neuropathology and Experimental Neurology. 2009;68(7):709-735.
10. Baugh CM, Stamm JM Riley DO, Gavett BE, Shenton ME, Lin A, Nowinski, CJ, Cantu RC, McKee AC, Stern RA, Santini VE, Lee HS, Kubilus CA, Stern RA. Chronic traumatic encephalopathy: neurodegeneration following repetitive concussive and subconcussive brain trauma. Brain Imaging and Behavior. 2012;6(2):244-254.
11. Strittmatter WJ, Saunders AM, Schmechel D, Pericak-Vance M, Enghild J, Salvesen GS, Roses AD. Apolipotrotein E: high-avidity binding to beta-amyloid and increased frequency of type 4 allele in late-onset familial Alzheimer’s disease. Proceeding of the National Academy of Science USA. 1993;90:1977-1981.
12. Guskiewicz KM, Marshall SW, Bailes J, McCrea M, Cantu RC, Randolph C, Jordan BD. Association between recurrent concussion and late-life cognitive impairment in retired professional football players. Neurosurgery. 2005; 57(4):719-726.
13. Broglio SP, Eckner JT, Martini D, Sosnoff JJ, Kutcher JS, Randolph C. Cumulative head impact burden in high school football. J Neurotrauma. 2011; 28(10):2069-2078.
14. Crisco JJ, Fiore R, Beckwith JG, Chu JJ, Brolinson PG, Duma S, McAllister TW, Duhaime AC, Greenwald, RM. Frequency and location of head impact exposures in individual collegiate football players. J Athletic Training, 2010; 45(6):549-559.
15. Guskiewicz KM, Mihalik JP, Shankar V. Measurement of head impacts in collegiate football players: relationship between head impact biomechanics and acute clinical outcome after concussion. Neurosurgery. 2007;61(6):1244-1252.
16. Schnebel B, Gwin JT, Anderson S, Gatlin R. In vivo study of head impacts in football: a comparison of National Collegiate Athletic Association division 1 versus high school impacts. Neurosurgery. 2007; 60:490-496.
17. Talavage, TM, Nauman EA, Breedlove EL, Yoruk U, Dye AE, Morigaki K, Feuer H, Leverenz LJ. Functionally-detected cognitive impairment in high school football players without clinically-diagnosed concussion. J Neurotrauma. 2010; 101001044014052 DOI: 10.1089/neu.2010.1512. Online ahead of print.
18. Brainard LL, Beckwith JG, Chu JJ, Crisco JJ, McAllister TW, Duhaime AC, Maerlender AC, Greenwald RM. Gender differences in head impacts sustained by collegiate ice hockey players. Medicine and Science in Sports and Exercise 2012;44(2):297-304.
19. Reed N, Taha T, Keightley M, Duggan C, McAuliff J, Cubos J, Baker J, Faught B, McPherson M, Montelpare W. Measurement of head impacts in youth ice hockey players. International Journal of Sports Medicine. 2010;31:826-833.
20. Bazarian JJ, Zhu T, Blyth B, Borrino A, Zhong J. Subject-specific changes in brain white matter in diffusion tensor imaging after sports-related concussion. Magnetic Resources Imaging. 2012;30(2):171-180.
21. Levy ML, Ozgur B, Berry C, Aryan HE, Apuzzzo ML. Birth and evolution of the football helmet. Neurosurgery. 2004;55:656-662.
22. Mihalik JP, Bell DR, Marshall SW, Guskiewicz KM. Measurement of head impacts in collegiate football players: an investigation of positional and event-type differences. Neurosurgery. 2007;61(6):1229-1235.
23. Viano DC, Pellman EJ, Withnall C, Shewchenko N. Concussion in professional football: performance of newer helmets in reconstructed game impacts–part 13. Neurosurgery. 2006;59:591-606.
24. LaBella L. A comparative analysis of injury rates and patterns among girls’ soccer and basketball players. Paper presented October 22, 2012 at American Academy of Pediatrics (AAP) National Conference and Exhibition, New Orleans, LA.
25. Labella CR, Smith BW, Sigurdsson A. Effect of mouth guards on dental injuries in college basketball. Medicine and Science in Sports and Exercise. 2002;34(1):41-44.
26. Wisniewski JF, Guskiewicz K, Trope M, Sigurdsson A. Incidence of cerebral concussions associated with type of mouthguard used in college football. Dental Traumatology. 2004;20:143-149.
27. Blignaut JB, Carstens IL, Lombard CJ. Injuries sustained in rugby by wearers and non-wearers of mouthguards. British Journal of Sports Medicine. 1987;21:5-7.
28. Hickey JC, Morris AL, Carlson LD, Seward TE. The relation of mouth protectors to cranial pressure and deformation. Journal of the American Dental Association. 1967;74:735-740.