
Summer 2013 - Vol. 8, No. 2
Insomnia: The Mind-Body Connection
Edward J. Purzycki, Ph.D.
Lancaster General NeuroCenter
BACKGROUND
Having been involved in sleep research and the treatment of sleep disorders since the mid 1980’s, I have found the treatment of chronic insomnia to be particularly challenging. In the good old days (before EPIC and RVU’s) members of the Lancaster General Health sleep disorders program met regularly to discuss the latest sleep research and to review challenging clinical cases. Back then we spoke frequently of the need for some type of structured program for patients with recalcitrant insomnia. The program never came to fruition, at least at that juncture, and so my colleagues and I continued to treat our insomnia patients on an individual basis using stimulus control, sleep consolidation and other behavioral strategies in an attempt to promote better sleep. Of course treatment of insomnia can be even more complicated when patients present with other conditions such as pain, anxiety, and depression, and such patients are often on multiple medications including psychotropic drugs, analgesics, and/or other medicines for various medical problems that can interfere with sound sleep. Although we did not measure outcomes back then, I suspect that our success was modest at best.
MINDFULNESS-BASED COGNITIVE-BEHAVIORAL THERAPY AT LGH
In 2010, a colleague (Jennifer Collins, Psy.D.) and I developed a mindfulness-based cognitive-behavioral therapy program designed specifically for our patients with persistent insomnia. It seemed to make intuitive sense that mindfulness meditation, a practice that was being used successfully to manage pain and anxiety, would also be valuable in treating insomnia - particularly when combined with cognitive-behavioral therapy. (Cognitive-behavioral therapy or CBT is a psychotherapeutic approach based on the premise that thoughts, not external events themselves, cause emotional distress.) There were also a few research articles suggesting that we might be on the right track with this approach.1,2
Although we modeled our program after Jon Kabat-Zinn’s MBSR program at the University of Massachusetts Medical Center, we modified the program to emphasize our primary goal of improving sleep. Since September 2010 we have completed 7 groups with 50 patients having completed the program thus far. As this article is being written, we are in week 3 of our 8th offering of the program. The aggregate outcome data from our first 4 groups are presented below. Although we have collected data on each patient in each subsequent group (pre and post data are provided to the referring physician upon completion of the program) we have thus far analyzed only the data from the first four groups. However, an overview of subsequent group data appears consistent with that of the first four groups: some patients in each cohort demonstrated dramatic improvement, some had modest improvement, and some had minimal improvement.
LGH Program Details
Our program requires that each patient be evaluated by one of our psychologists before being considered for the group program. For the purpose of maintaining a reasonably well-functioning group, we exclude from the group patients with severe psychopathology or patients whose needs exceed that which can be managed in a group setting. As this is a highly structured, agenda-driven program, participants need to be able to attend most if not all 8 sessions, profit from didactic type educational experiences, be reasonably well-socialized, and be willing to practice what they learn regularly. Most of the patients who enter our program present with multiple medical comorbidities, the most common being chronic pain. Many have mild-moderately high levels of anxiety and/or depression as well. Ages have ranged from 16 to 80 years, and about 80 percent are women. Although our first 4 groups were relatively small (4-6 patients per group) our more recent groups have each averaged 8-11 patients.
The first 2 sessions are dedicated primarily to the topic of sleep, with discussions of general sleep architecture, sleep hygiene, stimulus control, and sleep consolidation strategies. Although the primary goal of the program is to improve the quality of patients’ sleep, little time beyond the first 2 sessions is actually dedicated to sleep. Our philosophy is that when people learn to calm their mind’s activity, modify stress-producing thoughts, and begin to adopt a lifestyle that promotes compassion towards self and others, sleep will occur naturally.
From session one, patients are taught to meditate and are encouraged to develop and maintain a daily meditation practice. Very early in the process they begin to appreciate, perhaps for the first time, how quick they are to judge themselves, their circumstances, and other people, and how these judgments generate stress, tension, and—in general terms—suffering. These stress-producing thoughts are particularly evident during meditation when one is trying to simply attend to the breath. Although intended to be a time for quiet reflection, we learn that the “quiet” is frequently disturbed by intrusive thoughts like, “I don’t think I am doing this correctly” and, “Why didn’t they arrange to have a quieter room. There are too many distractions; I can’t relax;” or “Why am I sitting here doing nothing when I could be doing something productive!” Patients then begin to notice similar ruminations at nighttime, when distractions are at a minimum and they are desirous of sleep. Now the distraction becomes, “I’ll never get to sleep” or “I have an important day at work tomorrow and it’s imperative that I get a good night’s sleep.” It is common for our patients to attribute their insomnia to their inability to stop their minds from racing. Many are surprised to learn that this is what minds do and that there is nothing pathologically wrong with their minds. Through the practice of meditation they learn that while they cannot turn off their mental activity as if it had a switch, they can learn to manage their thinking more effectively leaving them more relaxed and setting the stage for a more restful pattern of sleep.
Through meditation our patients are able to monitor their mental activity and to identify stress-producing thoughts, many of which are simply replays of thoughts created years ago and are now applied rather automatically to a variety of situations and people. Our patients are then taught how to modify those thoughts. A thought like, “I can’t believe I did that, I’m such an idiot,” might become, “I’m disappointed that I did not handle that situation as well as I could have, but I will learn from that experience and manage similar situations differently in the future.” Many of our patients provide examples of how this process afforded them the opportunity to identify and modify mental activity that would have previously led to significant emotional distress. Nighttime musings of “I HAVE to sleep!” are transformed to “While I’d like to sleep, I have had sleepless nights before and have managed to get through the day. It’s not the end of the world if I don’t sleep well.” The paradox of course is that by reducing the pressure patients place on themselves to sleep, the better the chance that they will sleep.
Finally, our patients are instructed in meditation techniques like the body scan which allows them to attend to and relax their muscles, muscle by muscle, moment by moment. Does this approach seem like it might be beneficial to improved sleep and overall well-being? We thought so and our data suggests so.
Although these data are not the product of formal scientific methods, they do provide some evidence that our approach to insomnia is effective for some people. The following graphs represent the pre- and post-tests for 11 people in our first 4 groups. Only patients who completed at least 7 of the 8 sessions were included. Three patients were excluded from the data due to non-compliance or having a medical condition at the time of testing that dramatically skewed their results.
Pre- and post-test measures included the Beck Depression Inventory-II (BDI-II), the Beck Anxiety Inventory (BAI) and the Insomnia Severity Index (ISI). As shown in the three figures, for BDI (Fig. 1) the group improved from an average index of 19 (mild-moderate) to 9 (minimal); for BAI (Fig. 2), the group improved from 13 (mild) to7 (minimal-mild); and for ISI (Fig. 3) the group improved from 17 (moderate) to 9 (subthreshold).
Fig. 1. Beck Depression Inventory BDI): Average indexes for the group before and after participation in the program (see text).0-13 minimal; 14-19 mild; 20-28 moderate; 29+ severe
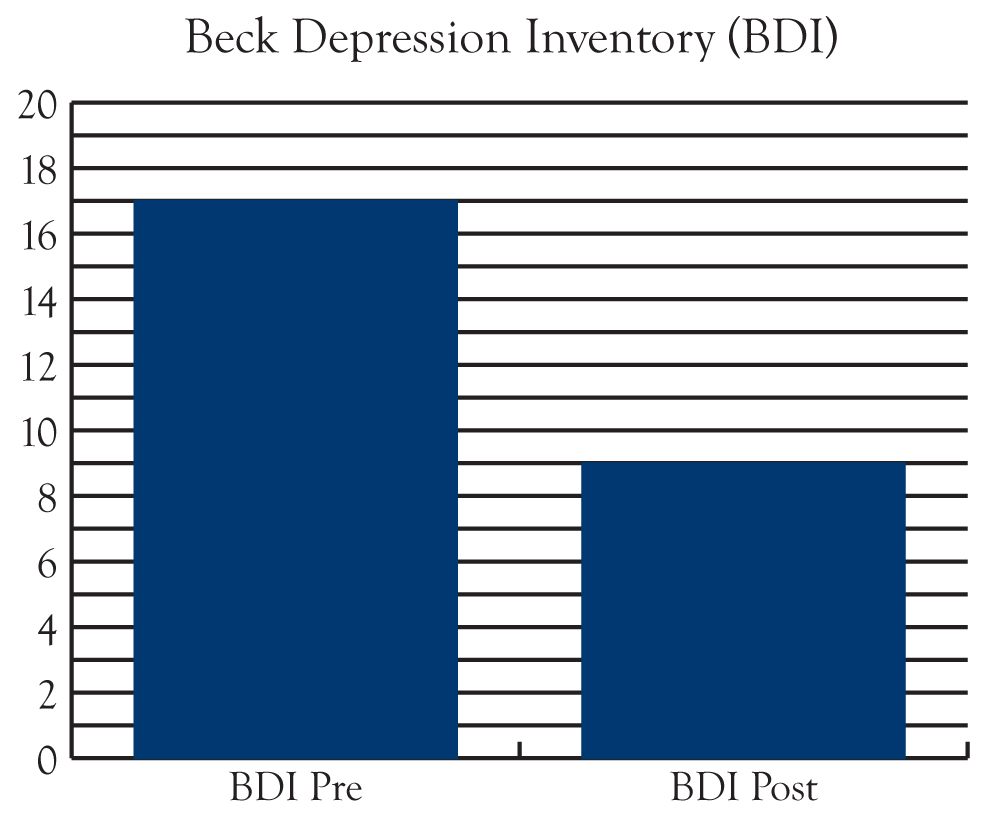
Fig. 2 Beck Anxiety Inventory (BAI): Average indexes for the group before and after participation in the program (see text). 0-7 minimal; 8-15 mild; 16-25 moderate; 26+ severe

Fig. 3: Insomnia Severity Index (ISI): Average indexes for the group before and after participation in the program (see text). 0-7= no clinically significant insomnia; 8-14= subthreshold insomnia; 15-21= moderately severe insomnia; 22-28= severe insomnia

Our plan is to continue collecting data not only to monitor for group trends but to monitor the success or failure of our individual patients. In reviewing the data collected thus far, it seems clear that level of improvement corresponds with the number of sessions completed and the individual’s overall commitment to the program as evidenced by homework assignments completed and weekly reports of progress and obstacles faced and overcome. We also plan to begin monitoring pain levels, as many of our patients have co-morbid pain disorders. Anecdotally, several of our patients reported better management of their pain along with an improved functional status as a result of their participation in the program. Data will be forthcoming.
References
1.Carlson, L.E. and Garland, S.N. Impact of Mindfulness-Based Stress Reduction (MBSR) on Sleep, Mood, Stress and Fatigue Symptoms in Cancer Outpatients. International Journal of Behavioral Medicine 2005, Vol. 12, No. 4, 278-285
2.Shapiro, S.L., Bootzin, R.R., Figueredo, A.J., Lopex, A.M. and Schwartz, G.E. The Efficacy of Mindfulness-Based Stress Reduction in the Treatment of Sleep Disturbance in Women with Breast Cancer An exploratory Study. Journal of Psychosomatic Research 2003, 54, 85-91