 Click to Print Adobe PDF
Click to Print Adobe PDF
Fall 2012 - Vol.7, No.3
|
Preventing Prematurity: One Woman at a Time
Stephen Ratcliffe, M.D., M.S.P.H., Angela Gambler, M.B.A., Megan Gross, M.P.H., R.N., Michael Horst, Ph.D., M.P.H.S., M.S., Thomas Raff, M.D.
|
  |
INTRODUCTION
Pregnancies that last less than 37 weeks result in premature births. The incidence of premature babies has risen steadily in the United States during the past 20 years, fueled in part by an increase in multiple births as a direct result of fertility treatments. In addition, the United States has experienced an epidemic of premature births related to biopsychosocial factors that have placed the U.S. in the third quartile of the world ranking in the percentage of births before 37 weeks gestation. In a recent World Health Organization study, the U.S. ranked 130 out of 183 countries in the world with an estimated 12% of its babies born prematurely.1
Severely premature babies, those born before 32 weeks gestation, have a marked increase in neonatal and post-neonatal mortality as well as chronic morbidity in the form of cerebral palsy, chronic respiratory conditions, and chronic developmental delays. Babies born between 32 and 37 weeks gestation often have prolonged stays in newborn ICUs and experience increased morbidity and mortality compared to full term babies. The cost of health care to treat the complications of prematurity in the U.S. was estimated to be approximately $25 billion in 2005.2
Premature births commonly occur as a result of premature labor or premature rupture of the membranes. Infections of the genital or urinary tracts are often associated with premature labor,3 as are psychological stress, maternal depression, domestic violence, illicit drug use, smoking and maternal trauma.4-6 Maternal conditions that result in impaired fetal growth such as gestational hypertension or pre-eclampsia may lead to decisions to induce a premature birth in order to prevent further fetal injury.1 One of the greatest risk factors associated with increased risk of prematurity is a previous history of preterm labor and/or delivery. Women who experience a “rapid repeat pregnancy” or a short inter-pregnancy interval of less than 9 months between births are also at increased risk of a subsequent premature birth.7
A REGIONAL RESPONSE TO THE PREMATURITY EPIDEMIC:
The Development of the FMEC-IMPLICIT Network The Family Medicine Education Consortium (FMEC) is a not-for-profit organization designed to foster interest in family medicine among medical students in the northeast United States and to support the overall growth of the discipline of family medicine. The FMEC sponsors an annual fall conference in the Northeastern U.S. that brings together 400 family medicine faculty and residents together with approximately 300 medical students, to explore cutting edge medical topics in a collegial setting. As Program Director of the Lancaster General Family Medicine Residency, Dr. Nikitas Zervanos was the visionary founder of this organization in 1993.
At the 2003 Northeast Regional FMEC Meeting in Pittsburgh, the concept was introduced of creating a network of residencies in Family Medicine that would use Continuous Quality Improvement (CQI) methods to collectively reduce the incidence of premature babies in their practices. With seed funding provided by the National March of Dimes, the network was formally created at the 2004 FMEC meeting in Rye, New York. Evidence-based reviews of 13 conditions associated with an increased risk of prematurity were presented. The working group identified five areas of focused intervention to use as the basis of the prematurity prevention program (Table 1), and added a subsequent intervention in 2006 (use of weekly progesterone injections in women with a prior history of spontaneous preterm delivery). Since 2004, the network has conducted ongoing evidence-based reviews of the literature and has adjusted its protocols based upon the best evidence. In 2005, this practice-based CQI network formally became the FMEC IMPLICIT Network (Interventions to Minimize Preterm and Low Birth Weight Infants Using Continuous Quality Improvement Techniques).
The FMEC IMPLICIT Network Infrastructure
The durability and success of the FMEC IMPLICIT Network has developed out of an effective collaboration among Lancaster General Hospital, the FMEC, the National March of Dimes, and the strong commitment of the members of the network. Lancaster General Health
The LGH Research Institute, under the direction of Dr. Michael Horst, has coordinated all aspects of data management including creating data abstraction tools and data dictionaries, establishing a web-based portal for data input and extraction, and conducting periodic analyses of the data. Angela Gambler, Supervisor of the Research Institute, has served in an essential role as the Network Coordinator since 2006. Dr. Stephen Ratcliffe, Program Director of the LGH Family Medicine Residency, has served as the IMPLICIT Network Director since its inception. Megan Gross was hired in 2010 as Project Coordinator for various sub-studies that are part of the IMPLICIT project.
FMEC
The FMEC serves as the sponsor of IMPLICIT and has a web site dedicated to the storage of materials essential to the daily function of a participating program. Laurence Bauer, Executive Director of the FMEC, has been a key supporter and contributing member of the network, particularly in the area of fundraising, networking, and media relations. The IMPLICIT Network meets twice a year, once at the annual fall FMEC Conference, and again in the spring meeting in Lancaster, PA.
National March of Dimes
The March of Dimes (MOD) has provided ongoing financial and technical support of the network, including funding to support program infrastructure, network meetings, and national speakers. The IMPLICIT network uses a MOD telephone conference line for its monthly audio conference meetings. Network Members
During the past 8 years, membership in the IMPLICIT Network has varied between 12 and 16 active programs, defined as those that have created the necessary infrastructure to conduct CQI and data extraction utilizing the existing clinical protocols. Programs that have stayed active in the network maintain teams that consist of faculty, residents, nurses, and designated data managers. Inactive members of the network have been unable to maintain the infrastructure to support data extraction and perform the ongoing CQI in their setting. Table 2 lists the names and locations of both active and inactive members of the network.
Functional Structure of the FMEC-IMPLICIT Network
The functional structure of the FMEC IMPLCIT Network is one of the keys to its longevity and success. All those involved in the project contribute time and effort on a volunteer basis. Each site has one or two champions who have a deep interest in obstetrical care and in decreasing prematurity rates of the patients they serve. The site leaders serve as the primary conduit to bring information and ideas back to the participating sites from the network as well as contributing ideas to the network as a whole.
The flexibility of the network has helped sites to continue to be involved despite conflicting responsibilities and expectations at the sites. Data collection has utilized several mechanisms including summer interns, AmeriCorps workers, clinicians, and program coordinators funded by local grants.
Member sites have contributed patient education materials, and developed guidelines, care protocols and IRB templates. In addition, each site has shared its successes and disappointments in “getting the word out” to their own communities in an effort to develop both professional relationships and ongoing financial support. This sharing of intellectual resources has reduced the work load of individual projects, and has improved efficiency and accelerated implementation of the model.
Another key feature of the FMEC IMPLICIT Network is that it is largely comprised of family medicine residencies. These sites have a highly vested interest in educating the next generation of family physicians in all aspects of medicine. All family medicine residencies are required to create an “environment of inquiry and scholarship which encourages support of faculty and residents to engage in scholarly activity.”8 The FMEC IMPLICIT project is congruent with this educational mission and environment of inquiry and scholarship. Residents and staff can work in a collaborative team-based approach using CQI techniques to implement the IMPLICIT interventions of patient education, prevention and clinical care.
Outcomes
Data are tracked at the level of individual members and across the collective IMPLICIT network. Individual network members have demonstrated improved birth outcomes such as decreased incidence of prematurity and low birth weight babies. The network as a whole has demonstrated improvements in the rates of screening for depression and administration of weekly progesterone to women at increased risk of preterm delivery.
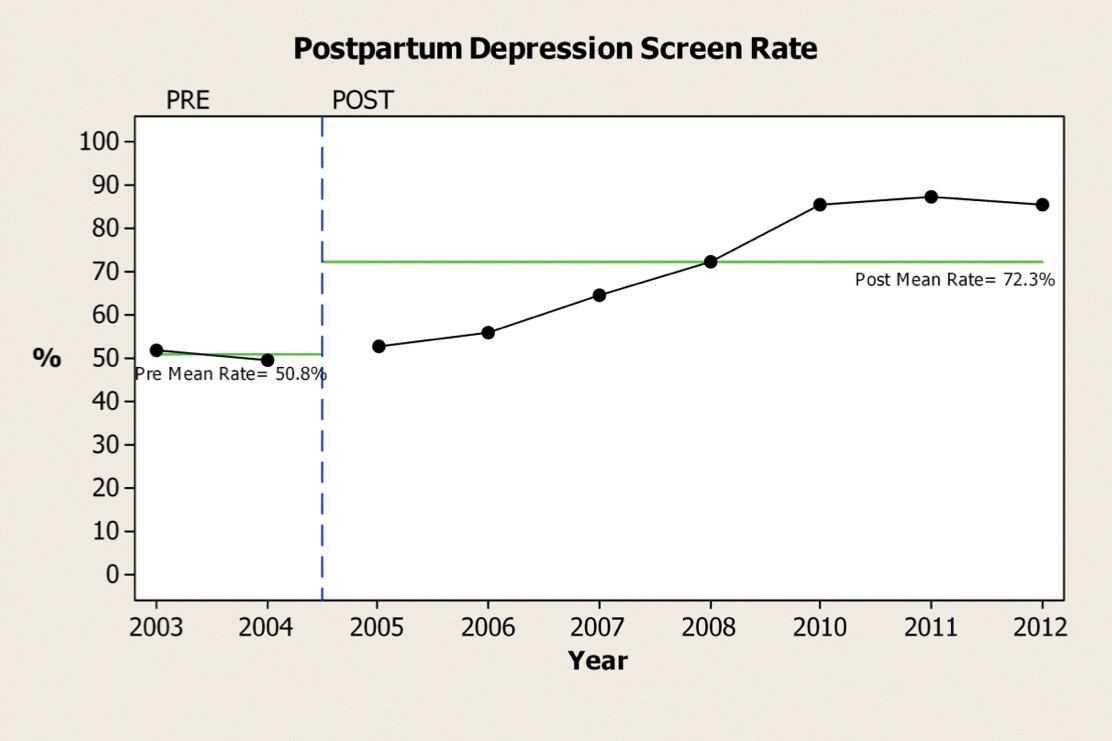
Screening for Depression
Analysis of network data has led to the validation of an instrument to screen for depression that aids in the reduction of screening time. Screening for depression is performed at a number of contact points during the prenatal and postpartum period, and a significant improvement in prenatal and postpartum depression care processes has been observed after initiating the IMPLICIT CQI program.9 The Network has demonstrated that implementing systematic screening for depression during prenatal and postnatal care can be done in a consistent, sustainable manner (Figures 1 & 2). During the first four years of the IMPLICIT program, screening for depression was done with both the 2-item PHQ screen and the 10-item Edinburgh Post Partum Inventory, but the network data demonstrated that a negative 2-item screen effectively ruled out depression more than 95% of the time.13 Consequently, the network now administers the longer screening test only if the 2-item screen is positive.
Figure 1.
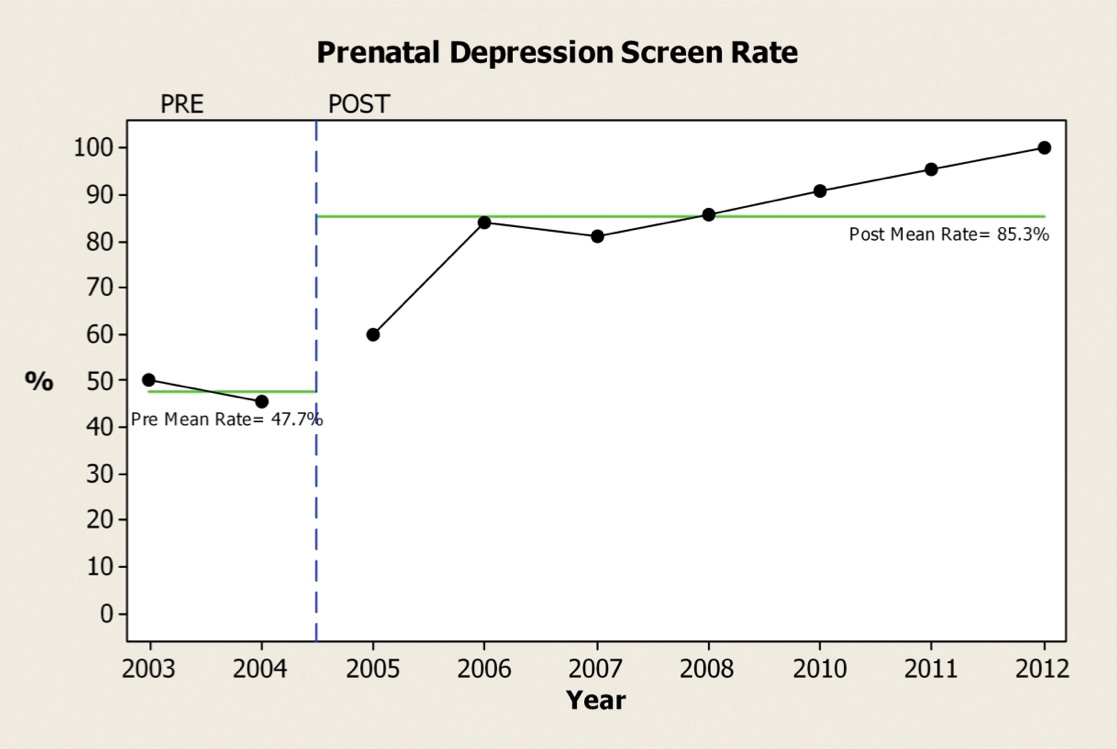
Figure 2.
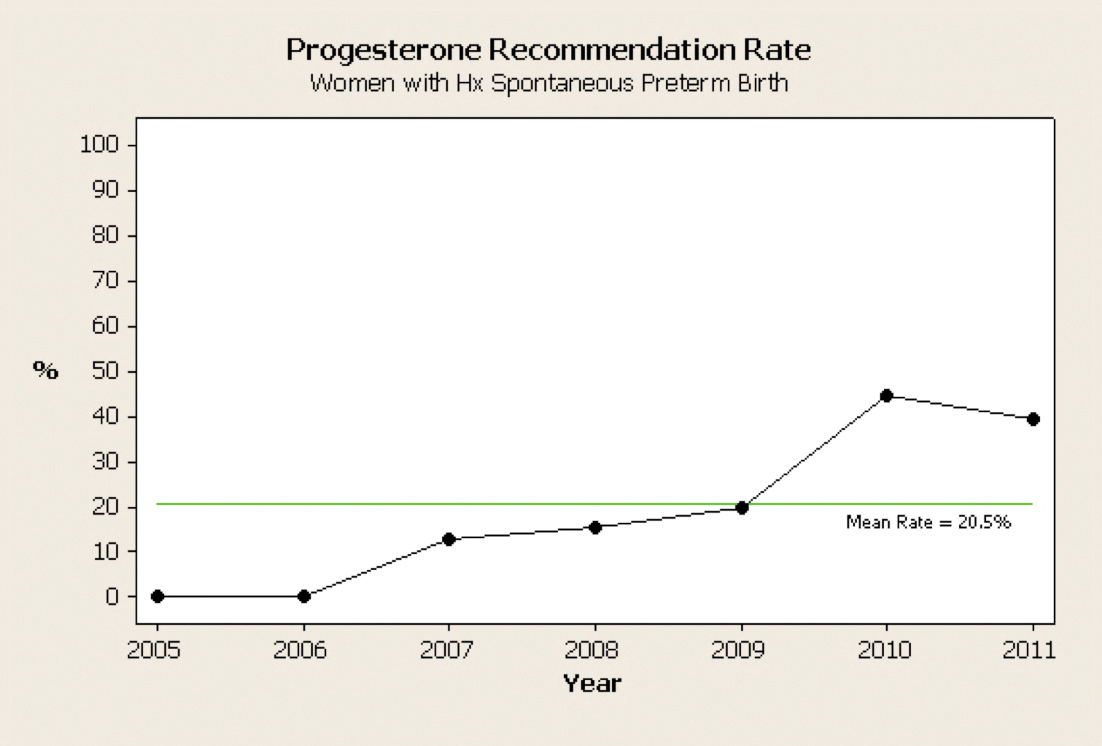
Administration of Progesterone
Although the network has made improvements in the administration of progesterone to patients at increased risk, process improvement is still urgently needed to lower prematurity rates (Figure 3). Women who have had a previous preterm delivery as a result of preterm labor or preterm spontaneous rupture of the membranes are candidates for the administration of 17 alpha-hydroxy progesterone via intramuscular injections given weekly between 18 and 36 weeks’ gestation. Many women find it difficult to adhere to this recommendation because of poor economic conditions and social support systems. They also find these painful injections difficult to tolerate for such a long period of time. This area of process improvement remains one of focused and coordinated work across the IMPLICIT Network.
Figure 3.
Prematurity Rates
Analysis of cumulative date in the IMPLICIT Network has not demonstrated a decrease in prematurity rates for the network as a whole, since some sites serve high risk populations where up to 50% of the preterm deliveries occur. In those populations induction of labor is frequently indicated medically to benefit the mother or fetus.10
However, three network members affiliated with the University of Pittsburgh (St. Margaret, Shadyside, and McKeesport Family Medicine Residencies) demonstrated a sustained decrease in prematurity rates during the past 8 years (Table 3).11 In addition, Barr and associates demonstrated that the combination of IMPLICIT protocols coupled with group prenatal care was associated with a decrease in prematurity rates in an urban family medicine training site in New York City (Table 4).12
Projects that have Grown out of the IMPLICIT Network
The FMEC IMPLICIT network has demonstrated that it is feasible to create a practice-based CQI Network linking more than a dozen family medicine residencies in the Northeastern U.S. This success has led directly to the funding of two ongoing projects in the maternal child arena:
a. Care Managers for Perinatal Depression
A goal of the FMEC IMPLICIT Network is to reduce disparities in health through a process in which key areas of perinatal care, including perinatal depression, are targeted for evidence-based improvement in evidence-based processes of care. These processes should be pragmatic and sustainable, as well as being developed and tested in the context of real clinical practices, and they have led to creation of a project titled Care Managers for Perinatal Depression (CMPD). This project is taking place at FMEC IMPLICIT Network sites in Lancaster and Philadelphia, in concert with federally qualified health centers at those locations.
Taking advantage of the unique setting of a perinatal quality improvement network with established enhanced care processes, the CMPD project aims to determine the added benefits of culturally tailored care management over the significant efforts already in place to treat perinatal depression. This project integrates a unique clinical care network focused on improving perinatal care delivery to low income and race/ethnic minority women with a research team experienced in working in the areas of depression in primary care, perinatal depression, and perinatal intervention evaluation among low income minority patients.
Lancaster General Health was awarded a grant from the Robert Wood Johnson Foundation Finding Answers: Disparities Research for Change Program to conduct a 3-year multi-site study aimed at evaluating the use of collaborative care in treatment of perinatal depression. One of the two main goals of the project is evaluating the benefits of care managers through three primary outcomes: (1) diagnosis within 2 weeks of screening, (2) treatment within 1 month of diagnosis, and (3) continuity of depression care from pregnancy to postpartum. The other goal is to conduct supplementary econometric and qualitative analyses to aid in understanding the provider and system context in which this intervention is implemented across the four study sites.
Interconception Care
Until recently, strategies for improving pregnancy outcomes have focused solely on improving prenatal care with little impact on poor birth outcomes. Improved access to prenatal care has also shown disappointing results, with nearly zero impact on the existing racial disparities in infant mortality, low birth weight, and prematurity rates.14 It is noteworthy that approximately half of all pregnancies in the U.S. are unintended, and by the time women enter prenatal care, it is often too late to affect birth outcomes.15, 16 The FMEC IMPLICIT Network followed the 2006 CDC Work Group recommendation to conduct a risk assessment and interventions for mothers in the interconception period.
Interconception care (ICC) is defined as care provided to women during the period following childbirth until the birth of a subsequent child. It includes medical and psychosocial interventions that improve a woman’s health and modify risk factors in order to promote a healthy outcome with subsequent pregnancies. Although there has been growing enthusiasm for the potential benefit of ICC, it has not yet been widely implemented. Barriers include lack of access to care for women between pregnancies, loss of insurance coverage after birth, maternal focus on infant health to the exclusion of their own health care needs, lack of awareness among providers, increasingly limited clinician time, and the lack of an established model for delivery of ICC.
The Pennsylvania March of Dimes supported the IMPLICIT Network’s proposal to start a pilot program for Interconception Care and granted it a community award in 2011 and 2012. These funds are being used to support eight Pennsylvania Programs that are in the process of implementing ICC. We plan to expand to other family medicine residency programs in the upcoming year.
The objectives of ICC are to: (1) better understand current ICC practices provided by family physicians within the context of well child visits; (2) assess the extent of specific maternal risk factors for recurrent preterm birth; and (3) explore maternal attitudes and receptivity to receiving information about their own health in the context of their child’s well child visit. These objectives are supported by the delivery during well-child visits of four maternal interventions that were chosen on the basis of strong evidential support, and their suitability for inclusion in a brief intervention model. They include smoking cessation, maternal depression, family planning, and folic acid supplementation.
Summary
We have summarized the steps taken to create a practice-based Continuous Quality Improvement Network involving family medicine training programs primarily based in the Northeastern U.S.. This collaboration has occurred because of the contributions and dedication of Lancaster General Health, the FMEC, the March of Dimes, and front-line family physicians and nurses. We have summarized some of the contributions that the FMEC IMPLICIT Network has made during the past 8 years. More information is available on the FMEC website.
References
1 March of Dimes, PMNCH, Save the Children, WHO. Born Too Soon: The Global Action Report on Preterm Birth. Eds CP Howson, MV Kinney, JE Lawn. World Health Organization. Geneva, 2012.
2 Institute of Medicine. Clinical Preventive Services for Women: Closing the Gaps, 2011.
3 Smaill F. Antibiotics for asymptomatic bacteriuria during pregnancy. Cochrane Database Syst Rev 2007:2: CD 000490. p 1-22.
4 Lumley, J., Chamberlain, C., Dowswell, T., Oliver, S., Oakley, L., & Watson, L. (2009). Interventions for promoting smoking cessation during pregnancy. Cochrane Database of Systematic Reviews , 3. doi: 10.1002/14651858.CD001055.pub3
5 Davalos DB, Yadon CA, Tregellas HC. Untreated prenatal maternal depression and the potential risks to offspring: a review. Arch Womens Ment Health. 2012 Feb; 15(1):1-14.
6 Grote NK, Bridge JA, Gavin AR, et al. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry. 2010 Oct; 67(10):1012-24.
7 Zhu BP. Effect of interpregnancy interval on birth outcomes: findings from three recentU.S.studies.Int J Gynaecol Obstet. 2005 Apr; 89 Suppl 1:S25-33.
8 ACGME Program Requirement for Graduate Medical Education in Family Medicine 2007 pg 7/8 11.B.5 and pg 38 IV.B.
9 Bennett, I. M., Coco, A., Anderson, J., Horst, M., Gambler, A., Barr, W., et al. (2009). Improving Maternal Care with a Continuous Quality Improvement Strategy: A Report from the Interventions to Minimize Preterm and Low Birth Weight Infants through Continuous Improvement Techniques. Journal of the American Board of Family Medicine. 22(4), 380-386.
10 Rohrer, JL. Improving Access to Progesterone Treatment in the Prevention of Preterm Birth, Lancaster General Research Day Poster, Third Year Resident Performance Improvement Project, May, 2012.
11 Srinivasan, S., Schlar, L., & Conti, T. IMPLICIT Network: Preventing Prematurity One Woman At A Time. Presentation given at the Total Quality Council at the University of Pittsburgh Medical Center, Pittsburgh, PA, September, 2011
12 Barr, W. B., Aslam, S., & Levin, M. Evaluation of a Group Prenatal Care-based Curriculum in a Family Medicine Residency. Family Medicine.43 (10), 712-717.
13 Bennett, I. M., Coco, A., Coyne, J. C., Mitchell, A. J., Nicholson, J., Johnson, E., et al. (2008). Efficiency of a Two-Item Pre-Screen to Reduce the Burden of Depression Screening in Pregnancy and Postpartum: An IMPLICIT Network Study. Journal of the American Board of Family Medicine. 21 (4), 317-325.
14 Healy, A.J., Malone,F.D., Sullivan, L.M., Porter, T.F.,Luthy, D.A.,Comstock, C.H., et al. (2006). Early Access to Prenatal Care: Implications for Racial Disparity in Perinatal Mortality. Obstetrics & Gynecology. 107(3), 625-631.
15 Finer, L.B. & Zolna, M.R. (2011). Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception. 84 (5), 478-485.
16 Santelli, J., Rochat, R.,Hatfield-Timajchy, K., Gilbert, C.,Curtis, K., Cabral,R, et al. (2003). The Measurement and Meaning of Unintended Pregnancy. Perspectives on Sexual and Reproductive Health. 35(2), 94-101.