
Spring 2012 - Vol.7 - No.1
Creation of a Dedicated Psychiatric Hospital Shortens ER Length of Stay for Mental Health Patients Referred from Regional Hospitals
Leopoldo Vocalan, Jr., M.D., MS
Behavioral Health Specialist
Lancaster General Health
ABSTRACT
INTRODUCTION
This study evaluated the effect of a larger inpatient psychiatric facility on Emergency Room (ER) Length of Stay (LOS) of psychiatric patients in surrounding hospitals.
The increasing number of mental health patients seeking care in ERs has increased utilization of medical resources, exacerbated ER overcrowding, and increased the number of psychiatric patients waiting for an available inpatient bed. These problems result in delayed and inadequate care or even death for the mentally ill, and increase the backlog of all patients in the ER. Traditional suggestions to improve this situation have included increased funding for ER expansion, increased staffing, and increased psychiatric bed availability. Recently, Penn State Hershey Medical Center and PinnacleHealth collaborated to create the Pennsylvania Psychiatric Institute (PPI), which effectively increases the number of available psychiatric beds in the area. This study was designed to determine if there was any effect on the LOS of psychiatric patients in surrounding ERs.
Methods
Data were gathered from anonymous retrospective record review of all psychiatric patients seen in three surrounding ERs from a period 1 year before and 1 year after the opening of the Pennsylvania Psychiatric Institute.
Results
The mean ER LOS Post-PPI was significantly shorter than Pre-PPI (p<0.0001), with a mean improvement by 22 minutes among 9,262 mental health patients. There were significant differences among the different hospital’s LOS (p<0.001) and between type of disposition (p<0.0001), with reduction greatest among patients who were eventually transferred to a psychiatric hospital by 2 hrs 18 min.
Conclusions
The creation of a larger psychiatric hospital, the PPI, was associated with a shortened ER LOS for psychiatric patients in three nearby hospital ERs.
Introduction
Mental illness imposes enormous emotional and financial burdens on individuals and their families.1 It is also costly for our nation as reflected in reduced or lost productivity and in medical resources used for care, treatment and rehabilitation. The burden of mental illness on health and productivity in the United States and throughout the world has long been profoundly underestimated because long term disabling effects of mental illness were not taken into account. Using Disability Adjusted Life Years (DALYs), which allows comparison of the burden of disease across many different disease conditions, the estimated direct and indirect cost of mental illness for 2008 was $193.2 billion.2 Data developed by the massive Global Burden of Disease study, conducted by the WHO, revealed that unipolar depressive disorders rank first in the burden of disease in middle and high-income countries.2 The same study also found that mental illnesses comprise three of the top five leading causes of burden of disease in high-income countries, such as the United States. It also projects that in the year 2030, unipolar depression will be the leading cause of burden of disease worldwide.
In the past four decades, the United States has lost effectively 93 percent of its much needed state psychiatric hospital beds.3 Several reasons have been cited including inadequate funding of psychiatric services, deinstitutionalization, and financial strain on hospitals caring for the uninsured and the underinsured. Because there are so few beds available, individuals with severe psychiatric disorders who need hospitalization often fail to receive necessary services.4 The consequences of the radical reduction in psychiatric hospital beds have been hospital emergency room overflow, homelessness, violent crime, and the use of jails and prisons as psychiatric hospitals.5,6,7 ERs are often used as waiting rooms for people in need of a psychiatric bed,5 and the congestion there backs up into the entire hospital system and compromises other medical care.
An American College of Emergency Physicians survey in 2008 indicated that ER psychiatric care is “extremely limited” and “getting worse.”8 Over 60% of mental health patients stay more than 4 hours after the decision to admit, while 33% wait over 8 hours and 6% wait over 24 hours in the ER. 85% of the survey participants also stated that wait times for all patients in the ER would improve if there were better psychiatric services available. These effects are significant because 1 in every 8 ER cases are for psychiatric disorders.9
In Central Pennsylvania, Harrisburg State Hospital (HSH) closed on January 27, 2006 after over 150 years of service to the mentally ill. HSH served its surrounding five counties: Cumberland, Dauphin, Franklin, Fulton and Perry. Since the HSH closure, central Pennsylvania clinicians have reported increasing difficulty accessing inpatient care for patients with mental illness. As in the rest of the country, patients suffering from psychiatric illnesses end up using surrounding ERs for their acute mental health needs.
Recommendations to improve this situation include: funding for increases in ER capacity, staffing, availability of psychiatric beds, and an increased overall system capability.10
Recently, Penn State Hershey Medical Center and Pinnacle Health have joined to create the PPI, a 74-bed psychiatric hospital which doubled Dauphin County’s acute psychiatry beds. The PPI also has a Triage Evaluation Center (TEC) which is designed to enhance and expedite evaluation and treatment of patients coming from surrounding hospitals. Patients with a psychiatric condition below 65 years of age, with normal vital signs, oriented to place and person, without new-onset psychotic symptoms or suspected overdose or active polysubstance abuse, are considered “low medical risk” and are immediately transferred to the PPI from surrounding ERs for expedited psychiatric assessment. If a decision is made to admit, patients can then be directly admitted to the PPI floor from the TEC. This study was conducted to gauge the effect of this larger capacity inpatient psychiatric hospital and the new model of emergency psychiatric care on ER LOS of surrounding hospitals.
Methods
An anonymous retrospective record review of all psychiatric patients seen in the ERs of Hershey Medical Center, Harrisburg Hospital and Community General Hospital, was conducted from a period 1 year before the opening of PPI on April 1, 2008 and 1 year after PPI became fully operational (i.e. April 1, 2007 to March 31, 2008 and July 1, 2008 to June 30, 2009). No ER changes/expansions which could affect patient LOS occurred during the 2 year time period. The sample included all patient types: pediatric, adult and geriatric patients. The database included information regarding the patient’s age, ER registration time, ER disposition time, type of disposition, diagnosis codes and insurance type.
Parameters studied were ER LOS of all psychiatric patients seen at the three ERs one year pre and post PPI. ER LOS, pre and post PPI were also compared among the different patient dispositions: patients subsequently admitted psychiatrically, patients admitted medically, those discharged against medical advice (AMA), and those discharged. ER LOS among the different diagnosis types and insurance types were also compared.
The Cox regression model was used to estimate disposition time of Pre-PPI and Post-PPI subjects. An analysis of variance model was used to assess the relationship between ER LOS, the dependent variable, with the following independent variables: Pre/Post-PPI status, Hospital, Disposition, Diagnosis, and Insurance. Two-way interactions of Pre/Post-PPI status and Hospital, Disposition, Diagnosis, and Insurance were also performed. Because the data were skewed, a logarithmic transformation was used prior to analysis. Tukey-Kramer adjustment was used to account for multiple comparisons. Analysis was conducted by PHS Data Management Department using SAS 9.2.
Results
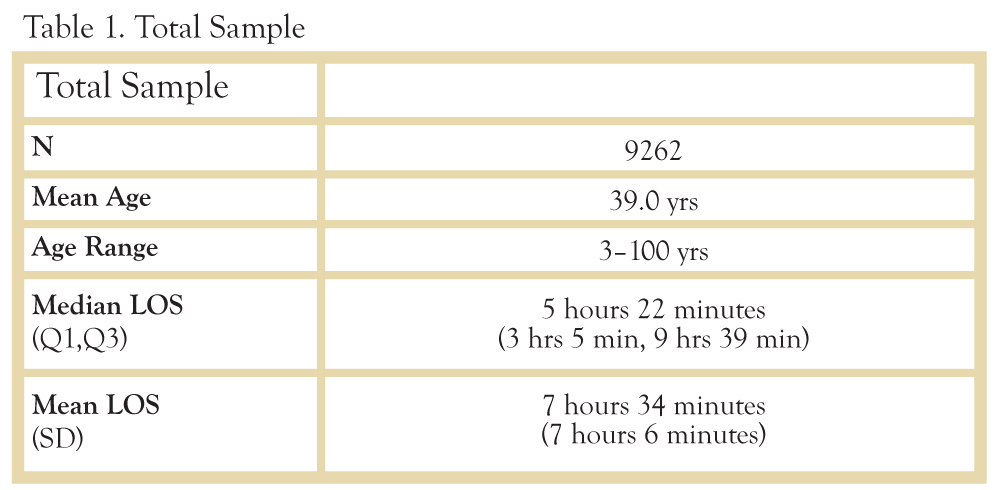
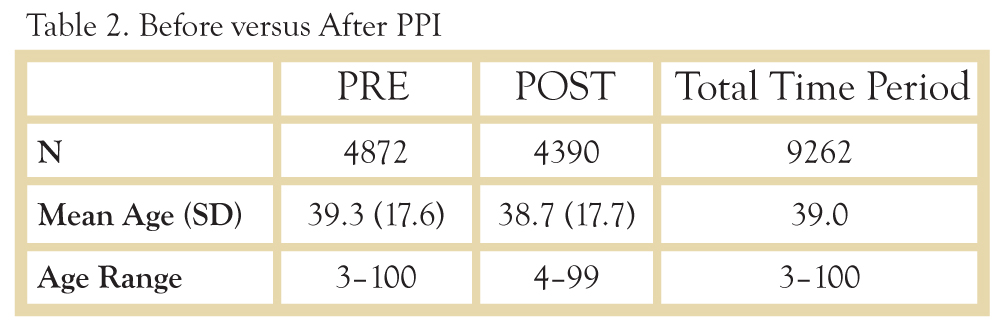
A total of 9,262 observations were collected during the two year period (Table 1): 4,872 observations one year before the creation of the PPI, and 4,390 observations one year after the creation of the PPI (Table 2). Ages ranged from 3 to 100 years old. Median ER LOS was 5 hours and 22 minutes (3 hours and 5 min, 9 hours, 39 min).
Hospital Type
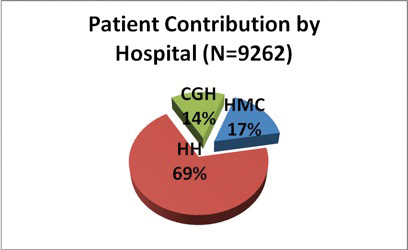
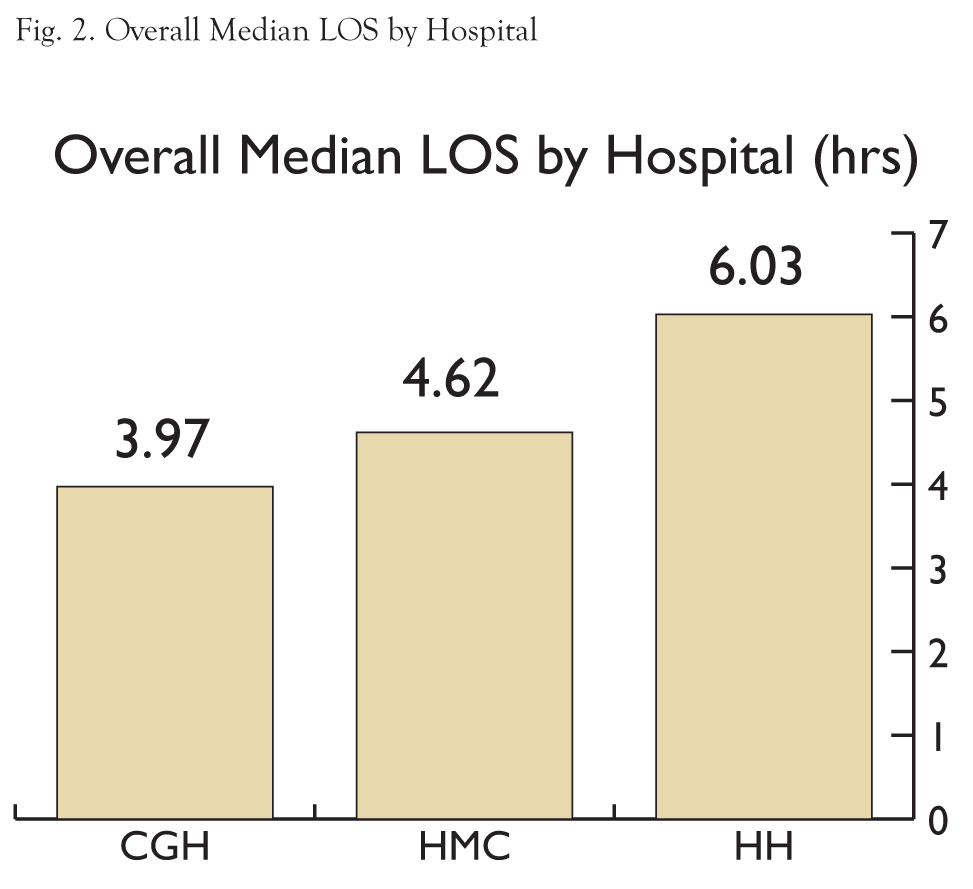
HH contributed the most observations at 6,423 (69.4%) followed by HMC at 1,545 (16.7%) and CGH at 1,294 (14%) (Figure 1). Patients stayed the longest at HH with a median of 6 hrs 2 min (3 hrs 19 min, 10 hrs 43 min), followed by HMC at 4 hrs 37 min (2 hrs 59 min, 7 hrs 8 min) and CHG at 3 hrs 58 min (2 hrs 22 min, 7 hrs 21 min) (Figure 2). The time differences were significant (p<0.0001).
Disposition Type
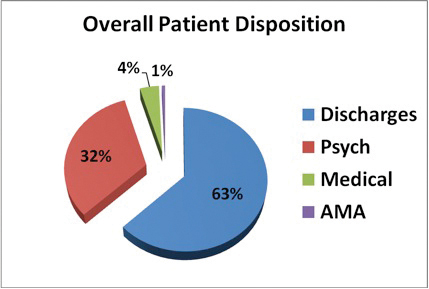
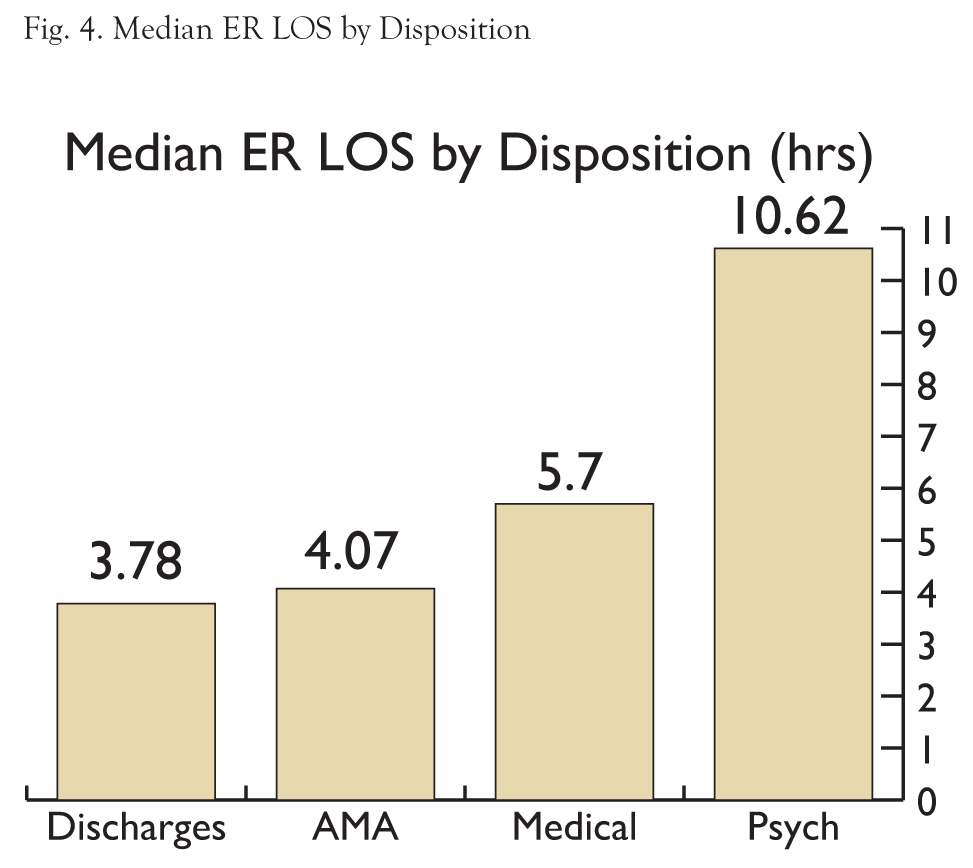
The majority of dispositions were discharges (5,830 cases, 62.9%), followed by transfers to psychiatric hospitals (3,001 cases, 32.4%), Medical/Surgical admissions (368 cases, 4%), and discharged against medical advice (63 cases, 0.7%). (Fig. 3) Patients transferred to a psychiatric hospital stayed the longest with a median of 10 hrs 37 min [7 hrs 22 min, 16 hrs 28 min]; followed by patients medically admitted with a median of 5 hrs 42 min [4 hrs 24 min, 7 hrs 33 min]); and patients who left against medical advice with a median of 4 hrs and 5 min [2 hrs 14 min, 6 hrs 36 min]). Patients who were subsequently discharged stayed the shortest with a median time of 3 hrs 47 min [2 hrs 23 min, 5 hrs 59 min]. (Fig. 4) The time differences were also significant (p<0.0001).
Diagnosis Type
For the purpose of this study, diagnoses were grouped into Mood disorders; Substance-related disorders, which included alcohol disorders; Anxiety disorders, Psychotic disorders, and other diagnoses. Mood disorders comprised the majority (27.1%), followed by Substance-related disorder (23%), anxiety disorders (21.7%), other diagnoses (14.9%), and lastly psychotic disorders (13.3%). Patients with psychotic disorders stayed the longest with a median time of 7 hrs 32 min [4 hrs 29 min, 12 hrs 35 min], followed by mood disorders at 7 hrs 8 min [4 hrs 13 min, 12 hrs 26 min], patients with other diagnoses at 6 hrs 35 min [3 hrs 38 min, 11 hrs 19 min], and substance-related disorders at 5 hrs 13 min [3 hrs 9 min, 8 hrs 59 min]. Patients with anxiety disorders stayed the shortest with a median LOS of 3 hrs 6 min [2 hrs 1 min, 4 hrs 38 min]. The time differences were significant (p <0.0001).
Insurance Type
54% of patients had Commercial insurance (5,018 pts.), followed by 30% who were Self Pay or unknown (2,803 pts.), 15% with Medicare/Medicaid (1,400 pts.) and 0.4% with other government insurance (41 pts.). There was no difference in ER LOS among the different insurance types (p=0.0644).
PRE VERSUS POST PPI
There were significant differences between the Pre and Post PPI ER LOS among the different hospitals; among the disposition types; and among the diagnosis types. There were significant interactions between Hospital and Pre/Post-PPI ER LOS; and between disposition types and Pre/Post-PPI ER LOS. There were no significant differences in ER LOS between insurance types.
Pre-PPI subjects had a median wait time until disposition of 5 hours and 34 minutes, whereas the Post-PPI subjects had a median wait time until disposition of 5 hours and 12 minutes, a difference of 22 minutes. (Table 3) Hazard ratio was 1.09 (95% CI - 1.04, 1.13); p < 0.0001).
Pre/Post PPI by Hospital Type
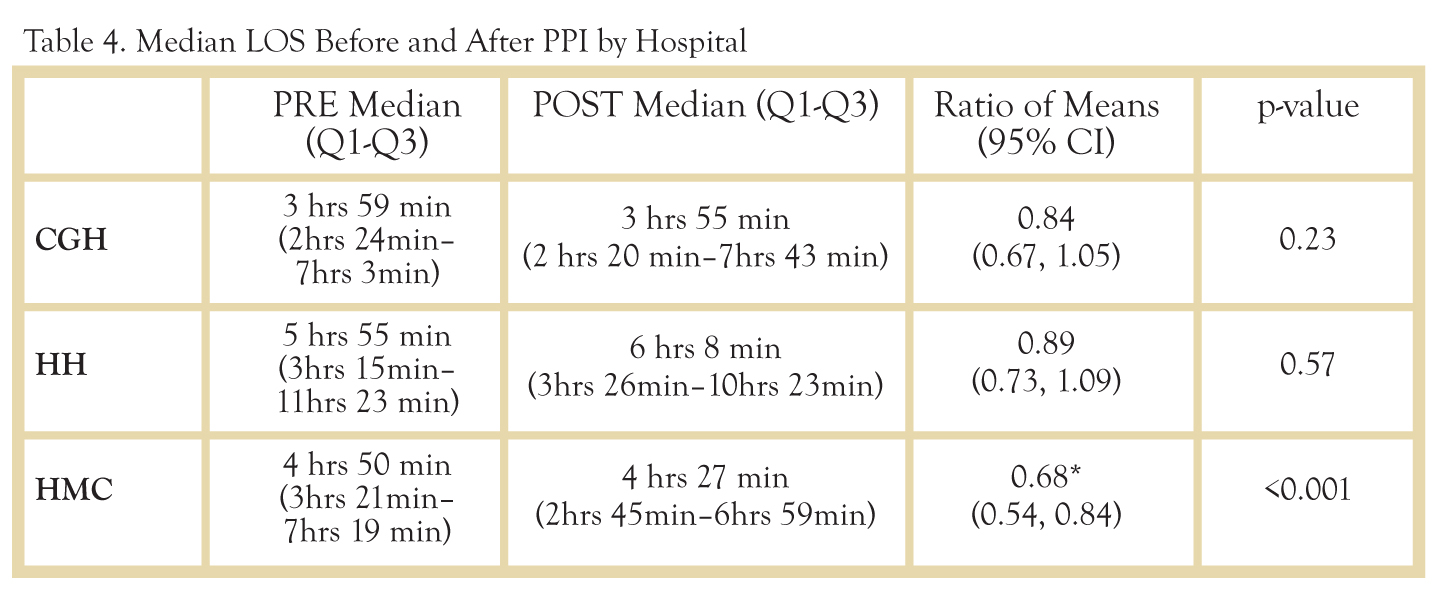
Only HMC showed a significant improvement in ER LOS, with a ratio of means of 0.68 (0.54, 0.84), p<0.001 (Table 4). This translates to 1 hr 33 min or a 32% reduction in LOS.
Pre/Post PPI by Disposition Type
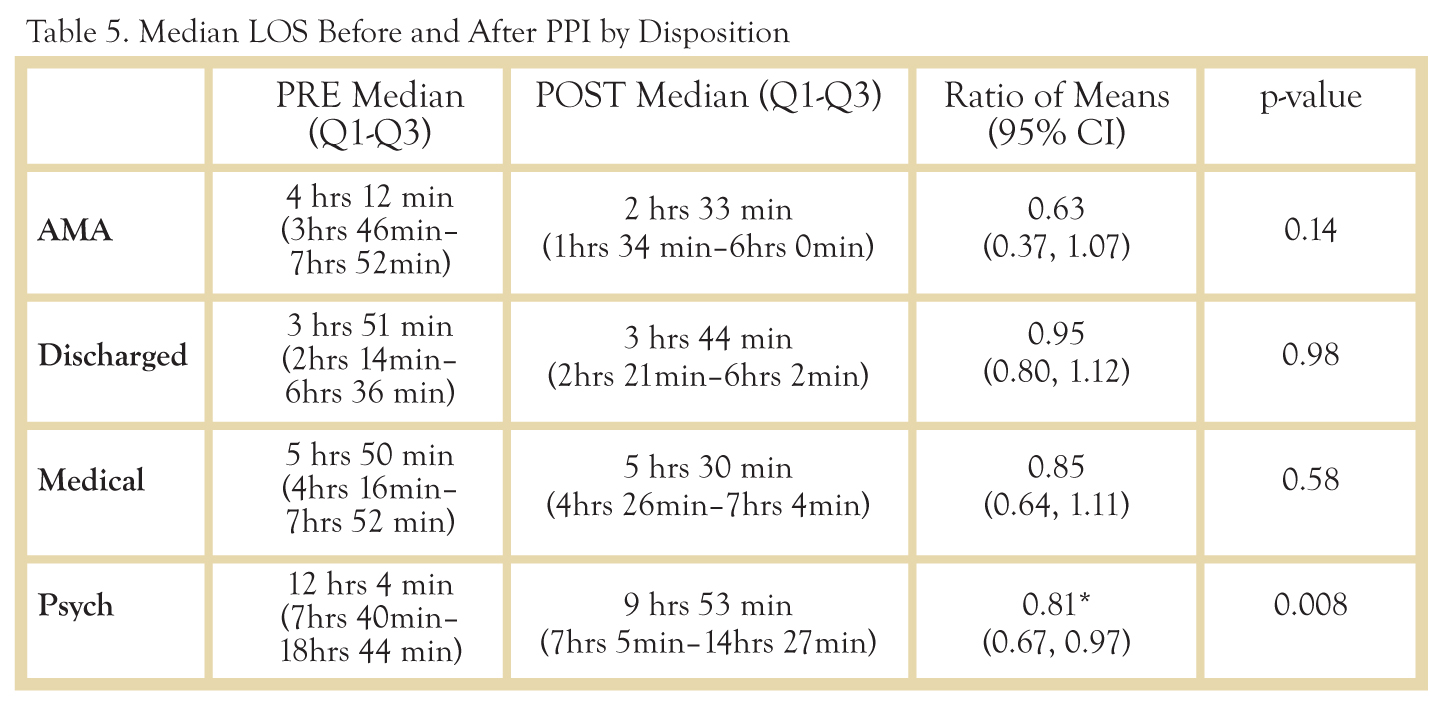
Only patients eventually admitted to a psychiatric hospital showed a significant improvement in ER LOS, with a ratio of means of 0.81 (0.67, 0.97), p<0.008 (Table 5). This translates to a 19% decrease in LOS or 2 hrs 18 min.
DISCUSSION
Average ER LOS of mental health patients in these three regional hospitals was 1 hour and 19 minutes longer than the 2008 national average for all ER patients. (11) This finding reflects the greater time and resources needed by psychiatric patients. Traditional suggestions to decrease LOS for psychiatric patients have emphasized increased funding to allow expansion of ERs, increased staffing, and increased availability of psychiatric beds. The present study shows an association between the creation of a larger psychiatric hospital and a decrease in ER LOS. The average decrease in LOS for the three nearby hospitals was significant at 22 minutes (p<0.0001), but the significance was due entirely to a decrease at one hospital (HMC), where it was 1 hr 33 min; a 32% reduction in LOS.
This finding can be explained by the fact that before the PPI was opened, patients were evaluated by psychiatry residents at HMC. Since the creation of the PPI, this evaluation has been done at the PPI TEC. There was no change in the way patients were being evaluated at CGH and HH except for the adoption of “low medical risk criteria” for transferring them to the PPI, which was implemented in all three hospitals.
It is also interesting to note that among the different dispositions, patients eventually transferred to a psychiatric hospital showed the greatest improvement in ER LOS by 19% or 2 hrs 18 min (p<0.0001). This would have been expected because the creation of the PPI would primarily affect wait times of patients eventually admitted to a psychiatric hospital.
It is still too early to determine whether creation of the PPI has shortened the interval between the initial ER visit and admission to a psychiatric hospital. Shifting the psychiatric evaluation to the PPI may only add to the total delay a patient has to endure before actually being admitted. Studies are currently ongoing at the PPI to determine if this is the case. Nevertheless, psychiatric patients are spending less time in ERs, the places where other patients are affected, the cost of stay is high, and intervals are measured in minutes.
The present study was limited by the dataset gathered from the three different hospitals. ICD 9 coding was not totally reliable in determining which patients were mental health cases. For example, a suicide attempt with overdose of medications was sometimes coded as an “adverse effect of medications;” self-injurious behavior was coded as “lacerations.” Conversely, “breath holding spell,” a psychiatric diagnosis given to certain defiant children, was sometimes coded for infants who were having apneic spells and were not suffering from a psychiatric illness. The dataset also did not include sex, race, and socioeconomic status. These parameters would have been helpful in determining if there were other confounding variables and/or interactions explaining the different ER LOS. Even though the database included insurance, the fact that a patient had medical insurance did not mean that they were covered for mental health, which would distort conclusions based on insurance. Lastly, since the database was de-identified, repeat ER visits by the same individual were undetected. This omission could lead to skewing of the data, which could reduce the validity of the analysis.
CONCLUSIONS
The creation of the PPI was associated with a shortened ER LOS for mental health patients in three nearby hospitals. This was the case for patients as an overall group, with a median reduction of ER LOS by 22 min., but among the three hospitals, HMC experienced the greatest reduction in ER LOS (1 hr 33 min). The reduction was greater among patients who were eventually admitted to a psychiatric hospital (2 hrs 18 min).
FUTURE DIRECTIONS
Studies of health economics need to be conducted to determine the financial impact of an increase in psychiatric bed capacity, particularly in reducing ER expenditures. Other study parameters like race, sex and socioeconomic status need to be included in the dataset and analyzed to determine if they account for differences in ER LOS. Higher order interactions in the analysis of variance also need to be performed to determine the improvement in ER LOS among the different dispositions, and among the different hospitals.
ACKNOWLEDGEMENTS
The authors would like to thank Thomas Lloyd, Ph.D. for his assistance in finalizing the completed paper and to Allen Kunselman for performing and interpreting the statistical calculations. Additional thanks to Roger Boyer and Jane Musser for extracting and compiling the data.
REFERENCES
1. Individual and Societal Effects of Mental Disorders on Earnings in the United States: Results From the National Comorbidity Survey Replication. Kessler, RC et al. 2008, Am J Psychiatry, pp. 703-11.
2. World Health Organization. The Global Burden of Disease: 2004 update. Geneva : World Health Organization, 2008.
3. Tuttle, Georgia A. Report to the Council on Medical Service. s.l. : AMA, 2008.
4. Emergency psychiatry in the 21st century: critical issues for the future. Bruffaerts R, Sabbe M, Demyttenaere K. 2008, Eur J Emerg Med, pp. 15(5):276-8.
5. Torrey, E. Fuller et al. The Shortage of Public Hospital Beds for Mentally Ill Persons. A report of the Treatment Advocacy Center. [Online] March 2008. http://www.treatmentadvocacycenter.org/Reportbedshortage.htm.
6. Some perspectives on Deinstitutionalization. Lamb, H.R, Bachrach, LL. 2001, Psychiatric Serv, pp. 52:1039-1045.
7. Changing demand for mental health services in the emergency department of a public hospital. Kalucy R, Thomas L, King D. 2005, Aust N Z J Psychiatry, pp. Jan-Feb;39 (1-2):74-80.
8. ACEP. American College of Emergency Physicians Psychiatric and Substance Abuse Survey 2008. s.l. : ACEP, 2008.
9. Agency for Healthcare Research and Quality. Mental Disorders and/or Substance Abuse Related to One of Every Eight Emergency Department Cases. AHRQ News and Numbers. July 8, 2010.
10. US Department of Health and Human Services. A Literature Review: Psychiatric Boarding. 2008.
11. Press Ganey. Emergency Department, Patient Perspectives on American Health Care. s.l. : Press Ganey, 2009.