Fall 2011 - Vol.6, No.3
Letters to the Editor
Conflicts of Interest - Stefan P. Kruszewski, M.D.
skruszewski@spkmd.com
The spring 2011 edition published the extremely important comments of the Editor-in-Chief, Lawrence I. Bonchek, MD about conflicts of interest (COI). I disagree with Dr. Bonchek on only one minor point, and I will start with that incidental footnote. Dr. Bonchek asserts that the requirement to disclose conflicts of interests by authors of medical journals may have the unintended consequences of producing an effect opposite to the one sought by those who argue for an increase in transparency. He argues, understandably in my opinion, that because so many authors are listing their extensive disclosures of pharmaceutical and medical device payments made on their behalf, the activity becomes commonplace and therefore may paradoxically serve to minimize the bias inherent in those disclosures. While that may be true, I believe that it may be better to look at full disclosure policies as one stepping-stone in a progressive and continuing effort to illuminate bias in research authorship. This is particularly true when clinical research is done and authorized by pharmaceutical and medical device makers who have a vested interest in positive results.
The process of COI investigation begins when the disclosures of authors, researchers and/or spokespersons identify individuals or groups who receive monies from one or more companies whose products are positively endorsed by them. With disclosures available, fraud specialists and consumers can evaluate the extent to which the authors accept money for their efforts. That knowledge may help to identify bias in the particular research article, speech, CME product or advertisement—or the information may help future discovery. For example, examination of disclosures can help us to understand whether the authors or speakers have disclosed all of the relevant conflicts of interest. This process is already employed by the US Department of Justice and the US FDA because often—and this may be a surprise to the reader—when an author or speaker is writing or talking about a specific product, he or she sometimes, despite an avalanche of self-disclosures, fails to reveal specific identification or bias with the subject matter in question. It’s a simple deception: A researcher receives, for example, grant monies from Companies X, Y and Z that support the research and subsequent publications from his/her work on several different pharmaceuticals. In the publication of the study relevant to Company X and their particular drug, the researcher discloses only his financial ties to Companies Y and Z. This gives the appearance of disclosure but obscures the bias inherent in failing to disclose the relationship that matters. That finding begins the process of COI investigation.
In the past several years, I have written at length about conflicts of interest. Rather than repeat any of those specific comments, I will list some of them in the references section that support my investigations.1-5 Perhaps the most important thing I can add here is to question why so many colleagues, particularly my psychiatric colleagues, refuse to lend their voices, regardless of their position, to this debate. As has been reported in many states, the number and amounts of monies accepted by psychiatrists to research, write or advocate for pharmaceuticals and medical devices has continued to climb, while at the same time the credibility of some of those individuals has been seriously questioned both in the nature and scope of the information disseminated.
Let me give a few examples from the abundance that are searchable in Internet archives. Although these examples are generally derived from psychiatry, psychiatric research and education have no monopoly on conflicts of interest, which have eroded credibility in every area of clinical medical research, direct-to-consumer sales, and education. Those conflicts have altered the risk/benefit analysis in medical marketing devoted to gabapentin (Neurontin), pregabalin (Lyrica), diet drugs, biphasic release oxycodone (OxyContin), natalizumab (Tysabri), modafanil (Provigil) and in a host of other drugs to support and treat neurological, hematological, sleep, pain and oncologic disorders. In psychiatric devices, the Vagal Nerve Stimulator (VNS) and, more recently, the trans-magnetic stimulator, both approved for the treatment of depression, represent devices whose efficacy claims are heralded by those individuals paid to market them, but are not supported by the breadth of the data used to determine efficacy.6,7 Some of the conflicts of interest have been more blatant. Obviously, erroneous information about devices is not limited to psychiatry, but involves, for example, drug-coated stents8 and knee and hip replacement hardware.9
A few specific examples from psychiatry: Dr. Louis Fabre, a psychiatric investigator in Texas, was sanctioned by the Texas medical board for research fraud involving clozapine;10 Dr. Scott Reuben, anesthesiologist, was accused of erroneous research results and then sanctioned for his research in rofecoxib (Vioxx), Celecoxib (Celebrex) and pregabalin (Lyrica);11 and Drs. Richard Borison and Bruce Diamond were judged guilty for a number of different problems while they were at the Medical College of Georgia.12 They did pivotal work on Zyprexa and other second generation atypical antipsychotics and antidepressants, and were both subsequently incarcerated and debarred from the US FDA related to their multiple fraud convictions. Dr. Maria Carmen Palazzo was found guilty of felony fraud and debarred from work with the US FDA for problems related to antidepressant research.13 Tonmoy Sharma, whose work was funded by Lilly, Janssen, and Sanofi, was eventually de-registered by the British BMC Fitness to Practice panel because of serious professional research misconduct.14
As the partial list of names noted above indicate, widespread and increased research and publication fraud in the medical sciences has been reported. However, perhaps akin to the relatively small percentage of adverse events suspected for any medicine or medical device that are reported to the FDA, the number of individuals who have been the subject of fraud investigations probably seriously under-represents the reality. Some of the single-research fraud may be explained by the need to publish in academic venues and the need, more often, to publish positive results. However, the majority of work that has come to the attention of the legal authorities has, at its basis, underpinnings of financial bias.
Conflicts of interest in meta-analyses present a more significant problem. This issue was outlined in the conclusions of a sentinel piece from JAMA, March 9th, 2011 when authors Roseman et al reviewed 29 meta-analyses of pharmacological treatments whose reviews were published in widely-disseminated and high impact scientific journals.15 Their conclusions: funding of the primary studies, and author COIs, were only rarely reported. This is a key finding because healthcare professionals often look to meta-analyses to help them determine the credibility and generalizeability of scientific findings. The reasoning is simple: the combination of several studies will be less influenced by a single study, will have higher statistical power, and will be generalizable to multiple populations. The hope and desire is a minimization of publication bias. Of course, meta-analyses, unfortunately, incorporate the very bias that is inherent in their collective methodology. In my opinion and fear, a collection of biased studies can result in a greater bias, not less, skewing single reports or studies that are already suspect by exaggerating bias that is neither accounted for nor disclosed.
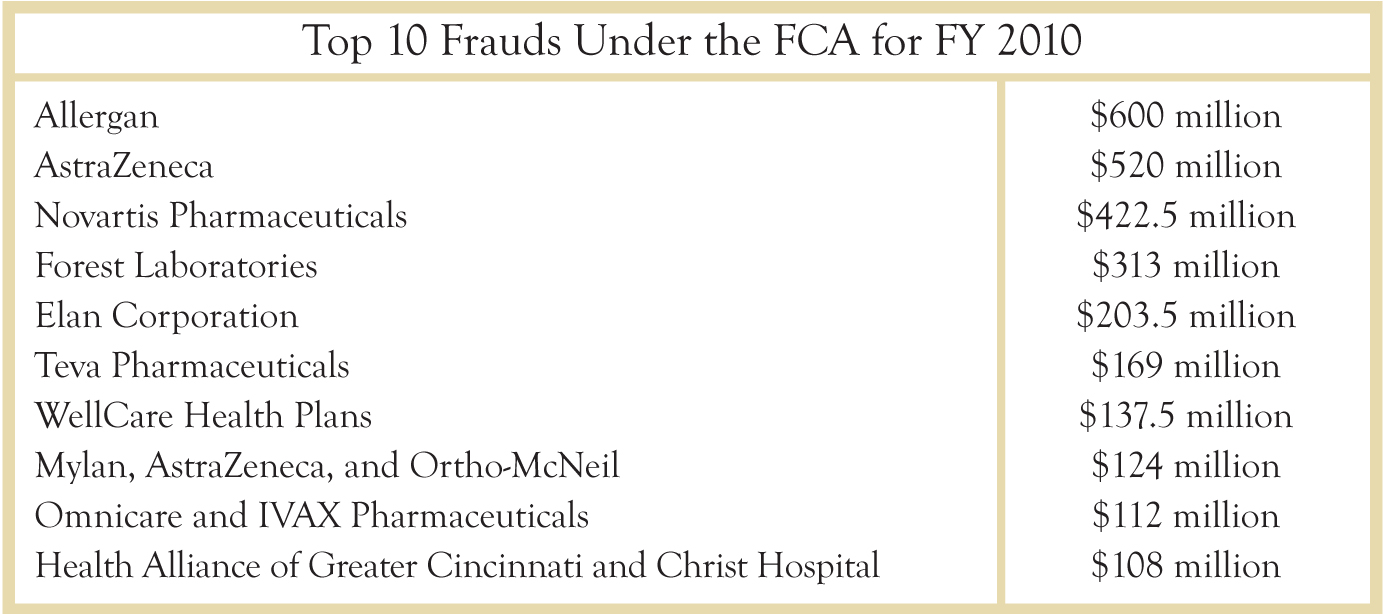
The problems associated with clinical research fraud based upon conflicts of interest are more than just a few rotten researchers who may have gotten greedy. Healthcare organizations, pharmaceutical manufacturers and medical device makers have all been repeatedly cited. All of them are conflicted because, while they have a duty and obligation to help and protect the human condition, they have a vested interest in financial results. From the Taxpayers ’ Against Fraud website (www.taf.org), the following list shows the “Top 10 frauds of 2010,” companies fined and penalized for fraudulent misrepresentations. Their violations, prosecuted under the federal False Claim Act (FCA), included AstraZeneca’s Seroquel, Forest Lab’s Celexa, Novartis’ Trileptal and Allergan’s Botox. The list is a tiny window to the scope of the problem incurred by corrupted science, misbranding, off-label promotion, and dissemination of inaccurate information.
Medical Conflicts of interest also affect the legal profession. As of this writing, former GlaxoSmithKline associate general counsel, attorney Laura Stevens, is being prosecuted for failing to disclose to the US FDA that Wellbutrin, an antidepressant manufactured by GSK, was being illegally promoted as a weight loss drug by the company.16*
The debate about conflicts of interest is not a theoretical one. It has a human face, despite the fact that many times that face is obscured by the same conflicts that obscure the science. Of the many examples I could offer, I will provide one from medical cases that I have reviewed.
A primary care doctor has been educated, by the company’s detailing agent and by authors whose written expert opinions have been subsidized by the drug’s manufacturer, about the benefits of prescribing gabapentin for pain associated with post-herpetic neuralgia. In this particular case, the instruction is on-label because the US FDA has approved gabapentin for this indication. The doctor starts his patient on gabapentin 600mgs in divided doses. The pain doesn’t respond. The patient, on no other medications, feels depressed and she tells him. The doctor raises the dose, assuming that his previous prescription was too small to minimize her pain. His patient now takes 900 mgs per day, 300mgs in the am and 600mgs at night. In a follow-up visit, she says that it isn’t doing much for her pain, but her mood, she believes, has worsened. The doctor raises the dose to 1800 milligrams per day. The patient subsequently reports some equivocal pain relief, but re-alerts the doctor that she feels sad, that her mood has “blackened.” Her husband calls the doctor, saying that she is talking about suicide. The doctor tells her to continue the medicine. Several days later, the patient, a wife and mother of two pre-teens and whose history is absent for suicidality, psychiatric or psychological counseling, hangs herself in the family basement. This is a catastrophic outcome.
What the family doctor didn’t know, and couldn’t have known, is that the company representatives who were selling the drug and reimbursing authors for articles which touted the benefits of gabapentin were, at the same time, failing to reveal the small but identifiable increased risk in suicidality associated with this antiepileptic drug. I have preserved confidentiality, but this story is one true and tragic outcome. The doctor was unable to assess the risk/benefit of the drug because some of the information provided to him was biased in order to misrepresent an adverse event known to occur with it.
This last point is generalizeable. If we physicians and surgeons, dentists and nurses, podiatrists and veterinarians, physicians assistants and nurse anesthetists do not receive unbiased and rigorously evaluated and accurately represented clinical information to guide our practices, we cannot hope to effectively or safely care for our patients.
EDITOR'S NOTE
* This action was recently dismissed by a Federal Court.
DISCLOSURE
Dr. Kruszewski does not have any current business or financial arrangements with any pharmaceutical company. Dr. Kruszewski previously participated, until 2001, on the speaker’s bureaus of the following companies: Pfizer, Inc., GlaxoSmithKline, Janssen (Johnson and Johnson), AstraZeneca, Sanofi, Wallace Labs, Eli Lilly, GE-Amersham Biosciences; and previously served on an Eli Lilly Northeast Advisory Panel (1998.) In 2003, due to his whistle-blowing activities, Dr. Kruszewski was terminated from a part-time position working for the Pennsylvania Department of Public Welfare and, subsequently in 2004, his clinical professorship at Hershey-Penn State College of Medicine was not renewed. In federal and state courts, Dr. Kruszewski serves as general and case-specific expert for national litigation re OxyContin, Neurontin and Zyprexa. He has served as Relator and co-plaintiff with the United States federal government on multiple qui tam litigations, three of which have been successfully settled and publicly unsealed: v. Southwood psychiatric facility; v. Pfizer; v. AstraZeneca.
Free Market in Healthcare - S. Scott Paist, III, M.D.
To the Editor:
I read with enthusiasm Dr. Bonchek’s The Free Market in Health Care: Why We Favor Choice Aver Access in the most recent issue of JLGH. His points are well-made, cogently argued and correct. It remains wondrous that Americans tolerate and even fight to maintain a system that costs so much and delivers so little. Our system of health care delivery is an ongoing national embarrassment that costs money and lives on a daily basis. I agree that the reasons for this are cultural and irrational and congratulate Dr. Bonchek for his editorial.
As a physician long in favor of a single-payer government-run system, I am equally certain that the free market generally establishes prices fairly EXCEPT in health care. While the market will set the price for cosmetic surgery or a Chevrolet as perfectly as it can be set, any consumer, when asked how much he would pay to have his life saved by, say, a cardiologist preparing to open a coronary artery in the midst of an acute myocardial infarction, could only answer, “I’ll give you everything I have.” Any private business person, when faced with this kind of market, will do exactly what the healthcare industry has done, keep pushing the price up.
Resources
1. Kruszewski SP. Doctors’ Conflicting Interests Can Cost Money and Lives, and Hinder Medical Discoveries. Available at ABC World News: abcnews.go.com/Health/medical-conflicts-interest-disaster-patients/story?id=13060973
2. Kruszewski SP. Credibility Gap, Revisited. Psychiatric News, the official publication of the American Psychiatric Association. 15 August 2008
3. Kruszewski SP, Paczynski R. Conclusions inconsistent with results with amphetamines and divalproex. American Journal of Psychiatry 2005 Nov; 162(11): 2197.
4. Kruszewski SP. Conclusions inconsistent with results with citalopram. American Journal of Psychiatry 2005 Nov; 162(11): 2195-2196.
5. Kruszewski SP, Bialy M, Paczynski RP. State Medical Board Responses to an Inquiry on Physician Researcher Misconduct. Federation of State Medical Boards, Journal of Licensure and Discipline. April-May 2008; 94(1): 16-22.
6. Calat, D. J. (2006, December 1). Vagus Nerve Stimulation and Depression: Conflict of Interest’s “Perfect Storm”. Psychiatric Times, 23 (14).
7. Wikimedia contributors. (n.d.). Transcranial magnetic stimulation. Retrieved May 5, 2011, from Wikipedia, The Free Encyclopedia: en.wikipedia.org/wiki/Transcranial_magnetic_stimulation
8. Surgery Deemed More Effective Than Boston Scientifics’ Taxus Stent. (2008, September 2). Retrieved from NewsInferno: www.newsinferno.com/legal-news/surgery-deemed-more-effective-than-boston-scientifics%E2%80%99-taxus-stent/
9. Smith, M. B. (2011, February 12). Zimmer vs. Dr. Berger: Nexgen Kneee Replacement Has High Failure Rate. Retrieved from Injuryboard BlogNetwork: atlanta.injuryboard.com/medical-devices-and-implants/zimmer-vs-dr-berger-nexgen-knee-replacement-has-high-failure-rate.aspx?googleid=288364
10. In the Matter of the License of Louis Fernand Fabre, Jr. M.D. Before the Texas Medical Board, Mediated Agreed Order, License No. D-5986 (Texas Medical Board October 6, 2006).
11. Rubenstein, S. (2009, March 11). A New Low in Drug Research: 21 Fabricated Studies. The Wall Street Journal. New York, NY, USA.
12. Office of the Attorney General. (1998, October 9). Attorney General Announces Guilty Plea in Medical College of Georgia Fraud Case. Atlanta, GA, USA.
13. Maria Carmen Palazzo: Debarment Order, Docket No. FDA-2010-N-0450 (Department of Health and Human Services, Food and Drug Administration March 28, 2011).
14. Cockcroft, L. Talking Head Psych who did Studies for Lilly - Banned From Practising In Britain: BBC psychiatrist Tonmoy Sharma is struck off. Telegraph (U.K.) http://www.telegraph.co.uk/news/main.jhtml?xml=/news/2008/04/01/nexpert101.xml. 1.4.2008.
15. Roseman et al. Reporting of Conflicts of Interest in Meta-analyses of Trials of Pharmacological Treatments. JAMA. 2011; 305 (10): 1008-1017
16. www.bnet.com/blog/drug-business/glaxo-lawyer-says-disclosing-illegal-activity-would-be-8220misleading-8221-to-the-fda/8074