 Click to Print Adobe PDF
Click to Print Adobe PDF
Summer 2011 - Vol.6, No.2
Animal Assisted Therapy: Effects on Stress, Mood, and Pain
Peggy Nepps, PsyD.
Charles Stewart, Ph.D.
Stephen Bruckno
|
 |
 |
 |
ABSTRACT
The purpose of this study was to measure the effects of Animal-Assisted Therapy (AAT) in 218 hospitalized psychiatric patients. It was hypothesized that AAT would improve anxiety, depression and pain ratings along with associated physiological measures. Self-ratings of anxiety, depression, and pain were collected before and after a session of AAT, and blood pressure, pulse, and salivary cortisol were measured. The same information was also taken from patients participating in a stress management program. There were significant decreases in depression (p<0.0001), anxiety (p<0.0001), pain (p<0.0001), and pulse (p<0.038) before and after AAT, but no differences between the two groups.
INTRODUCTION
It is thought that prehistoric man forged a bond with the most sociable and least fearful of wild wolves, leading to the evolution of Canis lupus familiaris, the domesticated dog.1 Such human-animal relationships are the focus of the multidisciplinary field of anthrozoology, which has research centers at the University of Pennsylvania, Purdue, and the University of Missouri.2 Much of that research has to do with the effects of relationships with animals on human health and well-being.
Domesticated animals have been used as an adjunct in the treatment of illness for over a hundred years.3 In the late 19th century, Florence Nightingale wrote:4
“A small pet animal is often an excellent companion for the sick, for long chronic cases especially. A pet bird in a cage is sometimes the only pleasure of an invalid confined for years to the same room.”
World War II convalescent hospitals used animals,5 and today both the U.S. Army and the Veterans’ Association are beginning studies to evaluate the widespread anecdotal evidence that therapy dogs can be used effectively as part of the treatment of post-traumatic stress disorder (PTSD) in soldiers returning from Iraq and Afghanistan.6 Many hospitals, psychiatric facilities, nursing homes, and rehabilitation centers routinely include trained animals, especially dogs, for socialization as well as therapeutic activities.
Animal-Assisted Therapy (AAT) is defined as the use of trained animals in facilitating patients’ progress towards therapeutic goals.7 The vast majority of AAT animals are dogs, although other species (e.g. horses and dolphins) are also sometimes used. The AAT dogs do not have the same task-oriented training as service animals (e.g. seeing-eye dogs who are trained to scan for oncoming traffic before the owner crosses a street). AAT dogs are, however, used in a more deliberate way than are animals in less-structured Animal Assisted Activities (AAA), such as dogs brought simply to visit residents in a nursing home.8 An AAT dog, for example, may be used as an adjunct to physical therapy. Patients can work on mobility skills while walking the dog, or they may increase range of motion by throwing a ball which the dog retrieves.9 Working with a dog may increase a patient’s willingness to engage in physical therapy. In mental health settings, AAT dogs have shown promise in getting resistant patients to engage in counseling, build trust in others, and express emotion.
AAT dogs typically complete both obedience and specific therapy training under the auspices of an organization such as the Delta Society, which sets standards and maintains a registry. Training topics for therapists include interpersonal skills, understanding the needs of specific client groups; client confidentiality; and safety and health codes for different types of facilities. Locally, most training is done by Keystone Enhanced Pet Therapy Services (KPETS), which has over 250 registered teams throughout Pennsylvania and Maryland.
PREVIOUS STUDIES
Animal-Assisted Therapy programs have been associated with positive effects in many studies10 although poor designs and small sample sizes have limited conclusions. A comprehensive literature search conducted by Nimer and Lundahl11 reviewed 250 studies, of which only 49 met their criteria for inclusion in a meta-analysis. Only 23 of the 49 used a control group, and the mean number of subjects receiving AAT in those studies was only 18. They found that the demonstrated improvement in symptoms was high in studies of autism-spectrum disorders, moderate in medical and behavior disorders, and low in disturbances of emotional well-being.
It can be challenging to design objective studies of psychological variables. In AAT studies, such variables have often been assessed by self-report, without measuring their physiological correlates. Barker and Dawson,12 for example, used the self-reported State-Trait Anxiety Inventory in a study of hospitalized psychiatric patients who participated in either AAT or another recreational therapy program. There was a statistically significant reduction in anxiety with both types of therapy, but no difference in effectiveness between them. Importantly, no physiological measurements were done; such measurements are important to corroborate self-reports and to more directly assess the impact of emotional distress on physical health.
Studies that address physiological variables are typically done with non-psychiatric patients. In one of the best studies done on AAT, Cole and coworkers13 showed that hospitalized heart failure patients who received a 12-minute visit from an AAT dog and its handler had lower anxiety scores as well as cardiopulmonary pressures and neuro-hormonal levels than did similar patients who were either left alone or had only a human visitor.
A small pilot study done at Lancaster General Hospital in 2007, looked at the effects of AAT with rehabilitation patients. Significant decreased in depression and anxiety scores were found along with a strong trend towards decreases in pain and pulse.14
CURRENT STUDY
The purpose of this outcomes research was to assess the effects of an existing AAT program on psychological as well as physiological variables in an inpatient mental health population. The study was carried out at Lancaster General Hospital over a two-year period, using measures of blood pressure, pulse, salivary cortisol, pain, depression, and anxiety. This study also compared the effects of AAT on these variables to the effects of a stress management program at the same site.
METHODS
After approval by the hospital’s institutional review board, all patients on the Mental Health Unit were offered the opportunity to attend one-hour weekly group sessions of AAT or the stress management program. The goal of the AAT sessions was to encourage social interaction and to improve coping through interaction with the dog and its handlers. Towards this goal, patients were encouraged to ask questions about the AAT dog and to share their own experiences with pets and animals while they petted and played with the dog. The comparison group was a video-based stress management program emphasizing cognitive restructuring and coping through humor. This group, unlike the pre-existing AAT group, was begun specifically for this study.
Participation was voluntary, and informed consent was obtained. Patients could participate in as many sessions as they wished, but could only participate in the study once. Before and after each session, participants filled out a questionnaire that assessed anxiety, depression, and pain. The depression and anxiety scales were validated instruments developed by David Burns, MD and used with permission.15 Pain was measured using the hospital’s standard 10-point rating scale. Age and gender, but no other patient identifiers, were collected. The participants had their blood pressure and pulse measured by trained staff who also collected saliva samples for cortisol analysis, which was used as an index of the stress response. Saliva samples were frozen and later analyzed by Salimetrics, L.L.C., in State College, Pennsylvania.
Data were analyzed for evidence of treatment effects and differences between the groups using a general linear model and a factorial analysis of variance.
RESULTS
218 participants were studied; their characteristics are summarized in Table 1. The mean age was 39.3 years, and diagnoses included the full range of psychiatric disorders. There were more women in the AAT group and more men in the stress management group (Chi Square p = 0.039). Women tended to have lower blood pressure (systolic and diastolic) at both measurement points.
Participants in both programs showed some significant improvement on psychological as well as physiological measures. Those who attended an AAT session showed decreases in depression (P<0.001), anxiety (P<0.001), pain (P<0.001), and pulse (P<0.038) as shown in Figures 1, 2, 3, and 4. The stress management program showed similar reductions in these variables, with neither program being significantly better than the other, according to factorial analysis.
Fig. 1: Changes in depression ratings
.jpg)
Fig. 2. Changes in anxiety scores
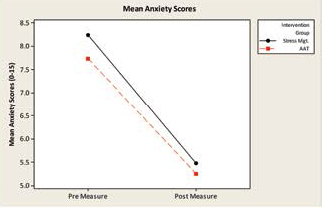
Fig. 3. Changes in pain scores
.jpg)
Fig. 4: Changes in pulse rate
.jpg)
DISCUSSION
The results of the study support the hypothesis that AAT can improve ratings of stress, mood, pulse, and pain, as well as, but no better than, a more traditional stress management program. These findings are consistent with those found by Barker and Dawson.12 This was shown by changes in anxiety, depression, pain scores, and pulse rates, although hypothesized changes in blood pressure and cortisol were not observed in either group.
The present study expands upon Barker and Dawson’s work by demonstrating that in addition to changes in the psychological variables, there were changes in the physiological variables of pulse and pain. The lack of change in blood pressure (also found by Cole13 ) may be explained in part by the fact that my psychiatric drugs can affect blood pressure response. In addition, the female subjects tended to have lower blood pressure at baseline, and there were more women in the AAT group than in the stress management group. These gender differences in group composition may have influenced results. Such issues can be hard to avoid in the clinical setting, particularly when participation is voluntary.
Since participants were self-selected to groups, a large sample size was used in order to minimize the effect of confounding variables. The two programs occurred at the same time of day and in the same room. They were standardized by having most (38 of 43) of the AAT sessions done by the same dog/handler team, and by presenting the stress management program in a videotape format to ensure a consistent experience. Valid and reliable rating scales were used to assess psychological variables.
This study cannot be regarded as an experiment in which participants are randomly assigned to treatment conditions because the patients were free to select the mode of therapy they would receive. Results could not necessarily be generalized to non-psychiatric patients or to those significantly different in age or culture from those in this sample. Interestingly, however, the results replicated the findings of the earlier pilot study done at Lancaster General with rehabilitation patients, so the type of patient may not make a difference in terms of efficacy. The AAT program would likely be ineffective for patients who disliked or feared animals, but those patients would not have participated in the AAT group in this study.
OBSERVATIONS
The AAT program was safe as well as extremely cost-effective because AAT teams were all volunteers and it was delivered in a group format. For patients who like animals, this may be a more acceptable alternative to the typical therapeutic programs on an inpatient mental health unit. This possible benefit is also supported by the observation that the AAT sessions were the most popular of all therapeutic activities offered on the unit. That may be important to a non-psychiatric population who could be expected to be less open than psychiatry patients to the idea of behavioral health services. There were also instances in which the AAT session served as a clinical bridge, with patients revealing significant issues (or, in one case, speaking for the first time in days) while interacting with the AAT team.
Further research is needed to evaluate how long the positive effects of AAT last, the amount needed to produce a durable effect, and ways to extend the benefits beyond the hospital and to other types of patients. There are also unanswered questions as to the conditions under which AAT is most effective. We are currently collecting data at the Lancaster Rehabilitation Hospital to determine if the use of AAT dogs in physical therapy improves outcomes or shortens length of stay.
ACKNOWLDEDGEMENTS
The authors want to thank Michael Horst, Ph.D. from the Research Institute of Lancaster General Health for help with statistical analysis and Elizabeth Lynn from Franklin and Marshall College for assisting in data collection. In addition, our special thanks go to the AAT volunteers and their dogs who made this study possible.
This research was funded with a grant from the Lancaster General HealthCare Foundation.
RESOURCES
1. Derr, M. Dog’s Best Friend. Chicago: University of Chicago Press. 2004, p. 21.
2. Herzog, H. Some We Love, Some We Hate, Some We Eat: Why It’s So Hard to Think Straight About Animals. New York: Harper. (2010).
3. Jones, B. (1985). The Psychology of Human/Companion Animal Bond: An Annotated Bibliography, Philadelphia: University of Pennsylvania Press. http retrieved 1/12/11
4. Nightingale, F. Notes on nursing: What it is, and what it is not. New York: Dover, 1969. P.103
5. Netting, FE, Wilson, CC, and New, JC. The human-animal bond: implications for practice. Social Work 1987; 32(1): 60-64.
6. Thompson, Mark (2010). Bringing dogs to heal: Care for veterans with PTSD. Time Magazine http://www.time.com/time/printout/0,8816,2030897,00.html Retrieved 1/10/11
7. Voelker, R. Puppy love can be therapeutic, too. JAMA 1995; 274:1897-1899.
8. Howie, A. Team training course manual (5th ed.), Renton, WA: Delta Society. 2000.
9. Chandler, C.K. Animal Assisted Therapy in Counseling. New York, Routledge.
10. Fine, A.H. (ed.). Animal-assisted therapy: Theoretical foundations and guidelines for practice (2nd ed.). San Diego, CA: Elsevier. 2000
11. Nimer, J. & Lundahl, B. Animal-assisted therapy: A meta-analysis. Anthrozoos 20(3), 225-238.
12. Barker, SB and Dawson, KS. The effects of animal-assisted therapy on anxiety ratings of hospitalized psychiatric patients. Psychiatric Services . 1998; 49:797-801.
13. Cole, KM, Grawlinski, A, and Steers, N. Animal-assisted therapy in patients hospitalized with heart failure. American Journal of Clinical Care 2007; 6(6):575-585.
14. Bruckno, SR. Man’s best friend: Efficacy of Animal-Assisted therapy [unpublished manuscript]. Lancaster: Lancaster Catholic High School: 2007.
15. Burns, DD. Therapist’s Toolkit: Comprehensive assessment and treatment tools for the mental health professional, Monterey, California: David D. Burns Press, 1995.