 Click to Print Adobe PDF
Click to Print Adobe PDF
Spring 2010 - Vol.5, No.1
OBESITY-RELATED HYPERTENSION AND OTHER RENAL ISSUES
Jeffrey L. Martin, M.D., FASN
Hypertension and Kidney Specialists
|
 |
Introduction
Obesity has well recognized but often underappreciated effects on the kidneys, and it thus plays a role in hypertension (HTN). This review will focus on these important relationships.
Chronic kidney disease (CKD) and obesity are commonly seen together. This pairing may occur simply because diabetes and hypertension are co-morbidities that are commonly seen with obesity and they are the main etiologies of CKD. However, there are also data to suggest that overweight and obese individuals have a higher prevalence of chronic kidney disease independent of the association with diabetes and hypertension. A meta-analysis by Wang et al showed that, compared with individuals who had normal BMI, overweight and obese individuals had a relative risk for kidney disease of 1.40 and 1.83 respectively.1 Clearly, if the burden of CKD is superimposed on obesity-related diabetes and hypertension, the combination is hazardous to health. Furthermore, there are other pathophysiologic mechanisms besides the obvious effects of obesity-related diabetes and hypertension on renal function.2
Renal Damage in Obesity
One of the early signs of obesity and the metabolic syndrome is hyperfiltration at the glomerulus. While this may seem initially as a beneficial function, over time this hyperfiltration leads to glomerular injury. This hyperfiltration is primarily driven by the activation of the Renin-Angiotensin-Aldosterone system (RAAS), and it occurs independently via local generation of Angiotensin II by adipocytes. Higher levels of ATII in turn cause increased constriction of the efferent renal arteriole and increased glomerular pressure. Higher levels of ATII also lead to increased aldosterone activity which in turn leads to increased sodium and water reabsorption and hypertension. Other effects of activation of the RAAS include endothelial dysfunction which may also play a role in glomerular dysfunction. The higher protein intake seen in obese individuals also can cause glomerular hyperfiltration.
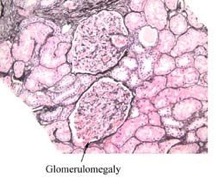
The typical lesion seen initially is simply large glomeruli (glomerulomegaly). (Figure 2) This effect in turn leads to focal areas of scaring and a histo-pathological lesion called secondary Focal Segmental Glomerulosclerosis (FSGS). It is in these areas of focal scar that albumin can be “leaked” into Bowman’s space and eventually into the urine. The detection of either micro-albuminuria (30-300mg/day) or macro-albuminuria (>300mg/day) is the hallmark of obesity-related FSGS, but it comes years after the original pathophysiologic changes occur. Interestingly, this same pathologic lesion is seen in Obstructive Sleep Apnea, a condition which commonly coexists with obesity, and compounds the glomerular damage.
Hypertension in Obesity
Hypertension by itself is also very common in obesity. Besides the above mentioned activation of the RAAS, a main factor in the pathogenesis of obesity-related HTN is activation of the sympathetic nervous system, either from higher levels of leptin or as a part of underlying sleep apnea. Left Ventricular Hypertrophy and absence of the usual “nocturnal dip” in blood pressure are two of the ominous markers for cardiovascular disease seen in obesity. Another important contributing factor is the tendency of obese individuals to have a higher sodium intake. Also, they usually have high insulin levels, which may independently add to HTN.
Treatment
The treatment of hypertension and CKD in obesity should focus on blockade of the RAAS. This can be accomplished with the use of ace inhibitors or angiotensin blockers as initial therapy, followed by the addition of Spironolactone if proteinuria or hypertension persists. Obviously renal function and potassium need to be monitored closely when these agents are used, particularly if in combination or in patients with advanced renal insufficiency.
Beta-blockers can be useful, particularly given the increased activation of the sympathetic nervous system. If required, carvedilol (Coreg®) should be the beta blocker of choice because of its relative neutral effects on insulin resistance and glucose intolerance.3
Diuretics, particularly thiazide diuretics, can be an important adjuvant for the treatment of hypertension, but they can worsen insulin resistance and impair glucose tolerance. Lower doses and avoidance of hypokalemia help to mitigate these effects.
Central alpha agonists such as clonidine and guanfacine are also helpful, again given the propensity towards activation of the sympathetic nervous system in obese patients. These drugs stimulate presynaptic α2 receptors in the vasomotor center in the brainstem with the effect of decreasing presynaptic calcium levels, and inhibiting the release of norepinephrine. The net effect is a decrease in sympathetic tone. Peripheral alpha blockers (doxazosin, terazosin) and calcium channel blockers can also be used without deleterious effects on glucose metabolism.
Other useful measures are treatment of Obstructive Sleep Apnea if present, and restriction of dietary sodium intake to less than 2000mg per day. The Table lists common measures to treat HTN, and their expected effects on systolic blood pressure, although these are ranges and individual results may vary.
|
Action
|
Decrease in SBP
|
|
Dietary Sodium Restriction
|
6-12 mm Hg
|
|
Weight Loss
|
5-10 mm Hg
|
|
Treatment of OSA
|
2-12 mm Hg
|
|
Exercise
|
4-8 mm Hg
|
|
Moderate Alcohol Intake
|
2-4 mm Hg
|
|
Drug Therapy
|
5-20 mm Hg per drug
|
References
1. Wang Y, Chen X, Song Y, et al: Association between obesity and kidney disease: A systemic Review and meta-analysis. Kidney Int. 2008; 73:19-33
2. El-Atat, FA et al. J Am Soc Nephrol. 2004;15:2816-2827
3. Bakris GL, Fonseca V, Katholi RE, et al. Metabolic effects of carvedilol vs metoprolol in patients with type 2 diabetes mellitus and hypertension: a randomized controlled trial, JAMA 2004; 292: 2227-2236.