Winter 2010 - Vol.5, No.4
DELIVERY OF SPECIALIZED CRITICAL CARE FOR TRAUMA PATIENTS: A LANCASTER GENERAL HOSPITAL PERSPECTIVE
John C. Lee, M.D., FACS
Associate Trauma Program, Medical Director
Lancaster General Hospital
|
 |
INTRODUCTION
Trauma has been called “the neglected disease of modern society,”1 akin to a forgotten epidemic. Because those afflicted lose both money and productive years of life, trauma represents a continuing public health problem of enormous proportion. Unlike other fields of medicine or surgery, trauma is invariably a multi-system disease process that can benefit from all advances in medical knowledge. As a result, trauma surgeons must constantly update their knowledge base and be facile not only with diverse areas of surgical care (e.g. general, neurosurgical, orthopedic) but also with medical management of multiple organ systems. Thus, not every surgeon or physician can provide the optimum care required by the trauma patient. The specialization required for the treatment of the severely injured trauma patient can now be acquired through fellowship training. As an acknowledgement that the care of the trauma patient is increasingly non-operative and takes place in the intensive care unit setting, modern day trauma fellowship graduates acquire added qualifications in surgical critical care, through the American Board of Surgery. In that respect, the fully trained trauma surgeon has a dual role as both a general surgeon and an intensivist, fully capable of dealing with the operative needs of the severely injured, and just as ready to handle the myriad complications encountered in the care of these patients.
BACKGROUND
Since optimal care of trauma patients takes place at designated trauma centers, 2 since 1987 Lancaster General Hospital has been committed to maintaining a level II trauma center. The PTSF (Pennsylvania Trauma Systems Foundation) certification standards mirror closely, and in most cases, far exceed those of the ACS-COT (American College of Surgeon-Committee on Trauma) .3,4 In 1997 LGH began in-house coverage by board certified general surgeons on a 24/7 basis, and in the fall of 2005 LGH implemented a new model of trauma delivery, with full-time, hospital-employed trauma surgeon/intensivists in charge of the trauma service.
This change was instituted partially due to very strong evidence that the organizational structure of the critical care unit can influence outcome. The field of critical care medicine has recently espoused the concept and advocated for the creation of dedicated intensivists, physicians with added qualifications in the subspecialty of critical care medicine.5 Reports from both medical and surgical intensive care units have shown improved patient outcomes for those cared for in closed/intensivist-led units, compared with the traditional open-admission models.6 The improvements are so striking, especially in terms of mortality (with reductions on the order of 30% to 40%), that the Leapfrog Group - a coalition of more than 170 public and private U.S. businesses and organizations with a combined health care enrollment of over 36 million people - has made ICU staffing by physicians a metric of quality.7
Surgical critical care is inherently different from its medical counterpart in that surgical patients require ICU-level care as a result of acute surgical intervention and not as a part of an exacerbation of chronic disease. This is especially true in the trauma patient, and for those trauma patients who already suffer from chronic illnesses, the addition of acute traumatic injuries adds to the ever increasing complexity of care that must be provided.
Although neither ACS nor PTSF standards require level II trauma centers to have a “surgically directed, dedicated ICU physician team 24 hours per day,”3-4 LGH elected to put into practice a full-time trauma intensivist model. By using traumatologists with skills and knowledge that go beyond the initial phase of the trauma response that involves resuscitation/hemorrhage control, and extends to the provision of high quality critical care, LGH - though nominally a level II trauma center - is able to provide the type of ICU care seen at Level I facilities. It has been reported that trauma patients in the United States receive over one-quarter of their entire hospital care in the ICU.8 This statistic is even more pronounced at LGH, with over one third being admitted directly to the ICU following resuscitation.
The implementation of the intensivist model for the trauma service has improved quality and throughput in a manner similar to that described in the trauma literature.9 We directly attribute these advances to the fact that as trauma intensivists, we function as captain of the ship (COS) for the care of each patient. This approach replaced the previous norm of decentralized care provided by admitting surgeons who – though they were the attending physicians of record – deferred most non-surgical care decisions to subspecialists. The result was a liberal consultative policy; it was not uncommon for a critically injured patient to be seen by pulmonology, cardiology, nephrology, hematology, infectious disease, and general internal medicine consultants.
By the fall of 2005, trauma intensivists became the attending physicians of record for all admitted trauma patients, even for those they did not directly resuscitate and admit. All patient-related decisions had to be approved by the trauma intensivists prior to actual implementation. Each intensivist assumed a one week block, 24-hours a day, ICU rotation schedule. Decisions regarding consultations with medical or surgical subspecialists were left to the sole discretion of the intensivists. From a beginning of only one intensivist in the fall of 2005, the trauma service now has grown to a full complement of seven trauma intensivists to meet the needs of the community.
EXPERIENCE
We have recently described and published our unique experience of transitioning to the trauma intensivist model.10 We concluded that a trauma intensivist-driven model can be successfully adopted in a community trauma program without the need for surgery residents, and demonstrated that significant improvements in throughput such as reduced ventilator days and ICU length of stay are possible without adversely increasing mortality (Figs. 1 and 2). Additional benefits of a trauma intensivist model include stricter adherence to established, evidence-based ICU protocols, which likely play a major role in the enhancement of throughput. Various ICU best practices have been concisely condensed into a trauma ICU daily rounding checklist, addressing and applying landmark critical care medicine concepts such as low tidal volume ventilation for acute lung injury/ARDS prevention and treatment. Our trauma multi-disciplinary checklist emphasizes measures that will prevent avoidable complications; daily rounds involve asking whether continued mechanical ventilation is necessary, whether an invasive line/catheter can be removed, whether proper enteral nutrition has been initiated, among others. Additionally, earlier involvement of social and rehabilitation services attends to the discharge needs of our patients. Thus, by having the trauma intensivist as the captain of the ship, we are able to significantly streamline the care of trauma patients at Lancaster General Hospital (Fig. 3).
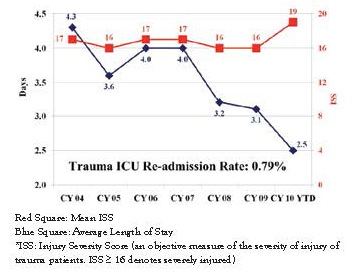
Fig. 1: LGH Average ICU Length of Stay and ISS
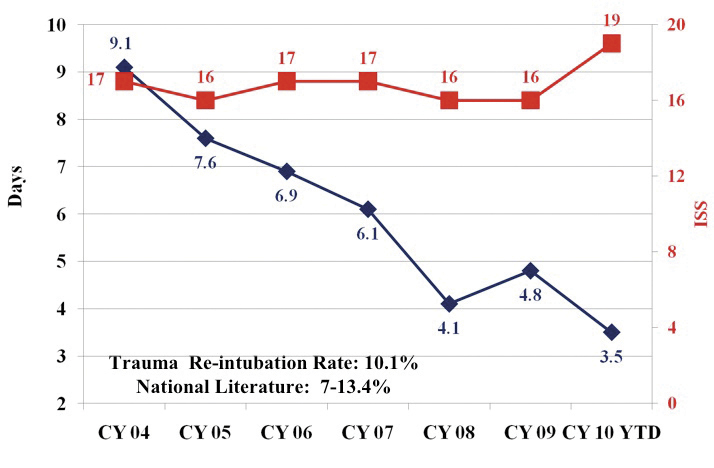
Fig. 2: LGH Average Ventilator Days
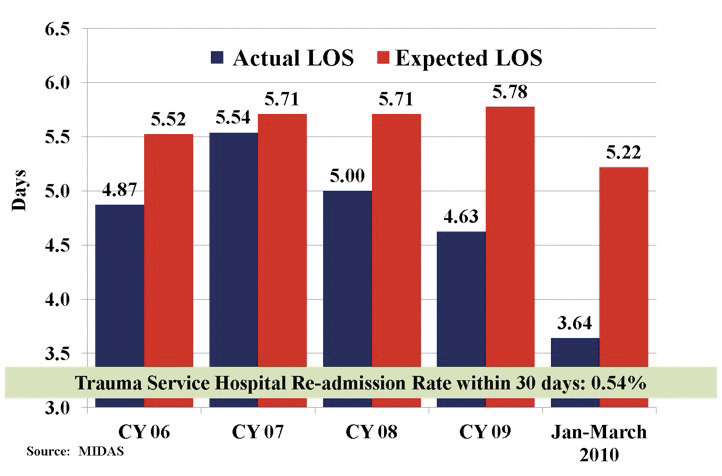
Fig. 3: Risk Adjusted Length of Stay
Our examination of the first three years of the trauma intensivist model here at LGH revealed important differences between surgically-directed and medically-directed ICU care. Specifically as it applies to trauma care, we feel and continue to believe that medical intensivists are no substitute for surgically trained intensivists. For example, our data regarding the ventilator days for those who did not receive tracheostomies demonstrates that there are fundamental variations in critical care practice between the two, despite both being board certified intensivists. We observed statistically significant differences in the ventilator days (3.7 vs. 2.7, p=0.00) between the pre and post trauma-intensivist eras.10 Importantly, there had been no significant advancements in ventilator management in the two comparison periods, 2003-2005 and 2006-2008, to account for the difference. Additionally, in those who ultimately did required tracheostomies, the differences in ventilator days were equally dramatic (19 vs. 13, p=0.00). By the nature of our training, trauma intensivists have the best understanding of the disease process and are in the best position to effect the necessary steps to address these injuries. On the trauma service, bedside, percutaneous dilatational tracheostomy is currently the default procedure of choice, versus its open counterpart in the pre-intensivist period. We were able to significantly streamline patient care, often performing the procedure on the same day as the decision to proceed. This contrasts with the pre-intensivist period when at least two providers had to agree to the operation (pulmonologist and surgeon - usually an otolaryngologist), a process further constrained by the need for operating room block time. The same procedural improvements have been made in other bedside procedures such as gastrostomy and placement of an inferior vena cava filter. Equally as important, as captain of the ship we possess the ability to implement transfer/discharge decisions without the restraint of reconciling the recommendations of multiple consultants, which can create noticeable drag on patient throughput.
CONCLUSIONS
The delivery of trauma critical care at Lancaster General has undergone significant evolution in the past 5 years. The Lancaster community currently enjoys high quality trauma care similar to that available at the finest medical centers in the U.S. With the opening of the state-of-the-art Trauma Neuro Unit (TNU) in the past two years, the trauma service currently provides the full complement of capabilities in critical care medicine to meet the needs of our patients. Our singular experience here at LGH has confirmed our belief that trauma intensivists are uniquely suited to lead the care of traumatized patients.
REFERENCES
1. Committee on Trauma Research, National Research Council, and the Institute of Medicine: Injury in America. Washington, D.C.: National Academy Press, 1985
2. MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354: 366-378.
3. Pennsylvania Trauma Systems Foundation. 2008 Standards for Trauma Center Accreditation. Mechanicsburg. PA: Pennsylvania Trauma Systems Foundation; 2008
4. American College of Surgeons. Resources For Optimal Care of the Injured Patient: 2006. Chicago, IL: Committee on Trauma, American College of Surgeons; 2006.
5. Hanson CW III, Deutschman CS, Anderson HL III, et al. Effects of an organized critical care service on outcomes and resource utilization: a cohort study. Crit Care Med. 1999;27:270-274.
6. Pronovost PJ, Angus DC, Dorman T, et al. Physician staffing patterns and clinical outcomes in critically ill patients: a systematic review. JAMA. 2002;288:2151-2162.
7. Leapfrog Group. ICU Physician Staffing Factsheet. Washington DC: Leapfrog Goup, 2004.
8. American College of Surgeon. National Trauma Databank. Chicago, IL: American College of Surgeon; 2002.
9. Nathens AB, Rivara FP, MacKenzie EJ, et al. The Impact of an Intensivst-Model ICU on Trauma-Related Mortality. Ann Surg. 2006;244:545-552.
10. Lee JC, Rogers FB, Horst MA. Application of a Trauma Intensivist Model to a Level II Community Hospital Trauma Program Improves Intensive Care Unit Throughput. J Trauma. 2010;69:1147-1152.