 Click to Print Adobe PDF
Click to Print Adobe PDF
Fall 2009 - Vol.4, No.3
Radiotracer-Guided Thoracoscopic Biopsy of Indeterminate Lung Nodules
Richard B. Thompson, M.D., F.C.C.P.
Cardiothoracic Surgeons of Lancaster, P.C.
|
 |
INTRODUCTION
With the advent of 64-slice CT technology and the increasing use of CT scans to evaluate patients at high risk for lung cancer, thoracic surgeons are being asked to determine the best diagnostic course of action for small indeterminate lung nodules with increasing frequency. Unfortunately, many small lung nodules are not amenable to CT-guided fine needle aspiration (FNA) and the responsibility resides with the surgeon to determine whether the nodule is benign or malignant. Nodules as small as 2 mm to as large as 1.2 cm can be notoriously difficult to find with traditional video-assisted thoracoscopic surgery (VATS), particularly if the nodules reside beneath the pleural surface. Utilizing standard imaging scopes and relying on instruments to "palpate" the lungs often lead surgeons to convert VATS surgery to traditional thoracotomy to get a diagnosis. This conversion increases the length of stay, the pain experienced by the patient, and the cost to the health care system. On average, a minimally invasive VATS patient would be in the hospital for 2 days, whereas a thoracotomy patient would be in the hospital for anywhere from 3 to 5 days.
By combining some existing technologies with some new instrumentation we are now able to locate and remove many of these subpleural lung nodules with minimally invasive techniques. Utilizing a technetium 99m gamma-emitting radiolabel and CT-guided injection in the region of the nodule, surgeons can now have an intraoperative map that indicates where to biopsy the lung.
MATERIALS AND RESULTS
At the University of Virginia, where this technique was pioneered by Dr. Thomas Daniel, close to one-hundred of these procedures have now been performed with excellent results. In a report of their initial experience with 77 patients published in the Annals of Thoracic Surgery and presented at the 2006 Annual Meeting of the Society for Minimally Invasive Thoracic Surgery, the UVA group found that the lesion was successfully localized 95 percent of the time.[1] Of these lesions under one centimeter, 50% were benign, 39% were primary lung cancer, and 11% were solitary metastases or lymphoma. The major morbidity from the procedure was pneumothorax at the time of injection, which occurred in 8 of 77 patients and was easily treated in the radiology suite with a pigtail catheter. The other major technical mishap in the group's initial experience was spillage of radiotracer into the pleural space. Though it is harmless, pleural space radiotracer increases the background radioactivity and makes localization more difficult.
PROCESS
tients are identified as potential candidates for the procedure after consultation with a pulmonologist, a thoracic surgeon and an interventional radiologist. The determination that surgery is indicated is based on both the size and location of the lesion, together with the specific risk factors of the individual patient. On the day of the procedure, patients are brought to the interventional radiology suite where a limited CT scan is performed to confirm the location of the nodule. Unless the nodule in question can be seen on the CT that same day, the procedure is cancelled. The radiologist and the surgeon proceed jointly.[2] (Fig.1) A 20 gauge needle is positioned just proximal to the pleural cavity and a 22 gauge spinal needle is then advanced through the other needle to a position just deep to the lesion. Once positioning is confirmed on CT, 0.1 ml of Tc99mm is injected deep to the lesion. A nuclear scintigram is then obtained and the patient is then taken to the operating suite for the operative part of the procedure.
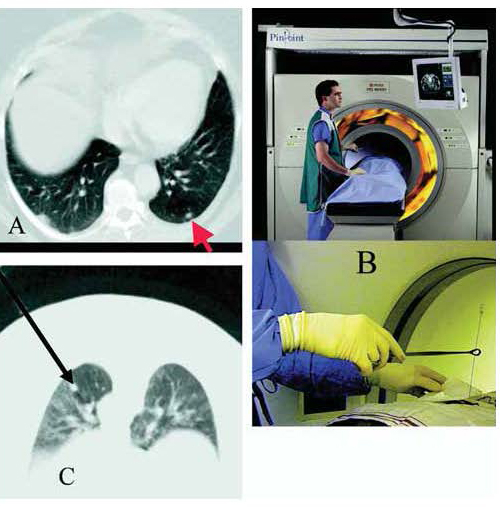
Figure 1. CT–guided percutaneous placement of technetium 99m macro-aggregated albumin radiotracer near a lung nodule. (A) The arrow on this CT scan points to an 8-mm nodule. (B) The radiologist uses CT fluoroscopy to place the radiotracer near the nodule. (C) The appearance of nodule on prone CT scan, with the long arrow showing track of the needle containing the tracer solution.
|
General anesthesia is induced and a dual-lumen endotracheal tube is placed for single lung ventilation. The patient is then positioned with the appropriate side up and 3 thoracoscopic port site incisions are made, each about 1.0 to 1.5 cm in size. Utilizing a specially designed radioprobe, the area in the lung parenchyma with maximal signal uptake is grasped and elevated. This area is then removed with successive firing of a commercially available stapler and removed in an endocatch bag. The specimen is then cut on the back table to be sure the lesion has been removed. The radioprobe is further used to document both the activity of the lesion on the back table and the background in the lung parenchyma beneath the lesion.
A pathologist then examines the specimen. If it is benign the procedure is finished and the patient will likely only be hospitalized overnight. If the lesion is a primary lung cancer, a traditional thoracotomy is performed with lobectomy and mediastinal lymph node dissection.
DISCUSSION
The diagnostic evaluation and treatment of small lung nodules is becoming increasingly important for the family doctor, internist, pulmonologist, and thoracic surgeon. Indeterminate nodules less than 1.2 cm in size are notoriously difficult to evaluate with PET scanning and often are not amenable to CT-guided FNA. Unfortunately, close to 50% of these lesions in higher risk patients are early stage lung cancers. The novel technique presented here allows thoracic surgeons to locate these small lesions without having to convert a minimally invasive VATS procedure into a traditional thoracotomy. This technique combines the expertise of multiple specialties and applies new technology to reduce hospital stay, reduce post operative pain, reduce patient anxiety, and most importantly, to catch early stage lung cancer when it is most treatable.
The technique has also been demonstrated to be cost effective. Using a decision analysis tool, the group at the University of Virginia found that radiotracer guided biopsy was more cost effective than thoracotomy.[3] The average cost for radiotracer biopsy was $27,887, while thoracotomy was $32,271.
Lancaster General Hospital and the Cancer Center have just made this technique available, and we look forward to offering the patients in our region a technique that is currently available at only a few other centers throughout the country.
References
[1] Stiles BM, Altes TA, Jones DR, et al. Clinical experience with radiotracer-guided thoracoscopic biopsy of small, indeterminate lung nodules. Ann Thor Surg 2006;82:1191-1197
[2] Grogan EL, Jones DR, Kozower, BD, et al. Identification of Small Lung Nodules: Technique of Radiotracer-Guided Thoracoscopic Biopsy. Ann Thorac Surg 2008;85:S772-777.
[3] Grogan EL, Stukenborg GJ, Nagji AS, et al. Radiotracer-guided thoracoscopic resection is a cost-effective technique for the evaluation of subcentimeter pulmonary nodules. Ann Thor Surg 2008;86:934 – 940
Richard B. Thompson, M.D., F.C.C.P.
Cardiothoracic Surgeons of Lancaster, P.C.
540 North Duke Street – Suite 110
Lancaster, PA 17602
717-544-4995
ctsl@cardiacsurgeons.com