 Click to Print Adobe PDF
Click to Print Adobe PDF
Fall 2009 - Vol.4, No.3
Cognitive Reserve in Alzheimer's Disease
Implications for Detection and Prevention
Matthew J. Beelen, M.D.
Program Director, Geriatric Medicine Fellowship
Department of Family and Community Medicine
Lancaster General Hospital
|
 |
ABSTRACT
Azheimer's disease is a progressive neurodegenerative illness for which there is currently no cure. Pathologic lesions are present in the brain long before patients manifest symptoms of the disease. There is wide variation in the correlation between anatomic pathology and clinical severity, a variation that the hypothesis of cognitive reserve seeks to explain. Patients growing old today are more educated than those of previous generations, which likely impacts cognitive reserve. This factor affects how and when they will present with Alzheimer's disease, their clinical course, and how we can best diagnose this disorder. Evidence suggests that cognitive reserve is modifiable to some extent, which may lead to new approaches to healthy aging and prevention of Alzheimer's. Many physicians are now seeing patients who express concern about their memory. Even when the physician shares that concern, basic testing doesn't always reveal a diagnosis, and it may not be clear if further evaluation is needed, or whether the symptoms are "normal" manifestations of aging. This review discusses this problem by looking at the hypothesis of cognitive reserve: its definition, supporting evidence, and clinical implications.
INTRODUCTION
The elderly population in the United States is expected to double from 35 million in 2000 to over 70 million in 2030.[1] As this segment of the population grows, we also expect the number of people suffering from Alzheimer's dementia to increase, with estimates suggesting that 7 million Americans will be suffering from this disease by 2030.[2] The natural history of this disease is such that the neurodegenerative lesions (neuritic plaques (Fig. 1), neurofibrillary tangles (Fig. 2), and β-amyloid deposits) develop slowly over time, eventually producing recognizable clinical symptoms. For this reason there is a long "preclinical" phase during which the pathology is present but symptoms are not noticed by the patient, family, or physician. Unfortunately, the disease may not be recognized until its more advanced pathologic stages, when it begins to cause significant functional impairment or behavioral disturbance.
Prior to a formal diagnosis, patients may suffer from subtle symptoms of memory loss or executive dysfunction, which are some of the earliest cognitive changes of Alzheimer's. These changes can cause difficulty with driving, management of finances and medication, general safety, and overall self-care. Early recognition of these symptoms is crucial to developing a plan of care before a crisis occurs. Life expectancy is on average 5-8 years from the onset of symptoms, and late diagnosis would limit the time available for care planning before the patient is no longer able to meaningfully participate in these discussions.[3]
THE COGNITIVE RESERVE HYPOTHESIS DEFINED
The idea of cognitive reserve originates from observations that the degree of brain pathology in Alzheimer's does not have a direct relationship to the degree of clinical symptoms.[4] These discrepancies may be the result of both passive and active differences in brain structure and function. The passive differences are due to brain size or neuronal count, while the active differences relate to neuronal changes, new synapse development, or increased efficiency of processing networks. The cognitive reserve hypothesis posits that these active changes develop in response to education and other cognitive stimuli throughout a person's lifetime. The resulting changes to neuronal processing networks provide more advanced compensatory approaches that the brain can use in the face of a neurodegenerative disease such as Alzheimer's. The end result is that individuals with Alzheimer's who have greater cognitive reserve will show symptoms of neurodegeneration later in the disease process.[5]
Cognitive reserve is thought to be a result of accumulated cognitive stimulation, most easily measured by years of formal education. However, cognitively complex occupations[6] and leisure activities[7] are also thought to contribute to cognitive reserve. Other factors such as innate intelligence, genetics, nutrition, and access to healthcare may impact educational and occupational status and therefore contribute to differences in an individual's ability to compensate for neurodegenerative changes in Alzheimer's. It also appears that physical activity may contribute to cognitive reserve to a small extent, but the exact mechanism by which this occurs is not entirely clear.[8] The actual variations in cognitive reserve observed among individuals are likely due to a combination of all of these factors.
CLINICAL CORRELATES OF THE COGNITIVE RESERVE HYPOTHESIS
Education and Cognitive Reserve
The cognitive reserve hypothesis predicts that higher educational levels would correlate with higher scores on cognitive testing in otherwise similar individuals. Hall et al. analyzed data on 117 non-demented community dwelling elderly individuals who eventually developed dementia. [9] Higher educational levels correlated with higher scores on multiple cognitive tests upon entry to the study and at multiple assessments preceding the diagnosis of dementia. Koepsell et al. compared dementia severity based on anatomical autopsy findings with most recent clinical assessment by Mini Mental State Exam (MMSE) prior to death. At all levels of anatomical Alzheimer's severity, they found that higher education correlated with higher scores on the MMSE. [10] This correlation was most pronounced in the earlier stages of the disease. O'Bryant and colleagues found that for college-educated individuals, using an MMSE score cut point of 27/30 rather than the standard 24/30 was more sensitive in diagnosing dementia (89% vs. 66%), while retaining specificity that was almost as good (89% vs. 99%).[11]
These studies support the expectation that individuals with more education (and thus cognitive reserve) would demonstrate better cognitive performance in the face of neurodegenerative diseases than people with less education.
Cognitive Reserve and Age of Onset
If cognitive reserve helps individuals compensate for neurodegenerative changes, we would expect individuals with higher education to be older when they manifest symptoms and are diagnosed with cognitive impairment. We would also predict that at any older age, there would be fewer highly educated people with significant cognitive impairment. Langa et al. studied these relationships using the Health and Retirement Study, comparing the educational level and cognitive status of two cohorts of over 7000 patients, one from 1993 and one from 2002. They found that the 2002 cohort had significantly more formal education and a significantly lower prevalence of cognitive impairment. They determined that about 40% of the decline in prevalence of cognitive impairment in the 2002 cohort was due to higher levels of education.[12] Thus, though other factors are surely involved in the decreased prevalence of cognitive impairment, it appears that education and cognitive reserve play a large role.
In another study that looked at how educational attainment impacts the eventual diagnosis of Alzheimer's, Ngandu et al. evaluated over 1300 people first at mid-life (mean age 50) and again in later life (mean age 71). At the second evaluation, they assessed cognition and analyzed educational levels and other lifestyle factors that could influence cognitive health. Compared to lower education (5 years or less), they found that higher education (9 or more years) was protective against Alzheimer's disease as compared to lower education (Odds Ratio 0.15, 95% CI 0.05-0.41). Adjustment for other individual potential confounding factors did not significantly change this association. In their discussion, the authors do note that since this was an observational study they were unable to demonstrate that the formal education actually produced the cognitive reserve, but they found a significant association between educational attainment and decreased risk of developing Alzheimer's disease.[13]
Cognitive Reserve and the Clinical Course of Alzheimer's
The hypothesis of cognitive reserve not only predicts differences in the risk of developing Alzheimer's dementia, but also differences in the clinical course once it is diagnosed. The progressive neuropathology of Alzheimer's predicts a pattern of gradual cognitive decline, until the time at which an individual's cognitive reserve is breached. When the brain can no longer compensate for the neurodegeneration, we expect to see more rapid decline in cognitive function, followed by the decompensation of social and occupational function that solidifies the diagnosis of Alzheimer's. When cognitive reserve is ample, we would expect this change point to more rapid cognitive decline to be delayed until it is closer to the clinical diagnosis of Alzheimer's dementia. Indeed, this pattern of decline was confirmed in the study by Hall et al. 9 The change point occurred 0.21 years closer to the actual diagnosis of dementia for each year of education beyond the median. For patients who had 4 years of formal education, the change point occurred 6.4 years prior to diagnosis, while it didn't occur until 3.8 years prior to diagnosis in those with 16 years of education. (Fig 3)
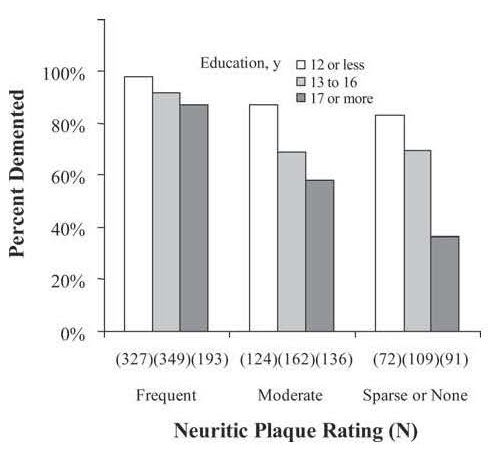
Figure 3: Proportion of participants diagnosed as clinically demented within 1 year of death at each neuritic plaque rating, categorized by years of education. Ns indicates the total number of participants, both demented and nondemented, with each combination of education category and neuritic plaque rating. Copyright permission was obtained for the use of this figure. (Roe, Roe CM, Xiong C, Miller JP, et al. Interaction of neuritic plaques and education predicts dementia. Alzheimer Dis Assoc Disord. 2008;22:188-193) |
A final, and more concerning implication of the cognitive reserve hypothesis is that because they do not manifest symptoms until later in the disease process, more highly educated people may have a quicker decline and shorter survival once they are diagnosed with Alzheimer's. Since they have a much greater degree of neurodegeneration at diagnosis, more rapid deterioration of cognitive function would be expected from that point. Multiple studies provide evidence for this clinical pattern. Branduet et al. followed 670 patients diagnosed with Alzheimer's dementia over three years and found that the rate of cognitive decline (as measured by MMSE and Mattis Dementia Rating Scale) was significantly higher in those with medium (9-12 years) and high (>12 years) levels of education compared with those with less education (<9 years). They adjusted for several variables that can impact the rate of decline in dementia.[14] Similarly, in a study of nearly 500 patients with Alzheimer's who were given a battery of cognitive tests at several points over 3 years, Wilson and colleagues found that a higher educational level predicted a more rapid rate of decline in global cognition.[15]
As previously mentioned, having a more complex occupation or participating in mentally stimulating leisure activities appear to impact cognitive reserve in a manner similar to that of formal education. When looking at a cohort of 171 patients with Alzheimer's over 2.5 years, Andel et al. found a significant association between lifetime occupational complexity and rate of cognitive decline as measured by MMSE in patients with Alzheimer's.6 Helzner et al. studied the relationship between leisure activity and cognitive decline and found that there was an association between participation in intellectual leisure activities such as reading and playing games (as opposed to more social or physical activities) and a faster rate of cognitive decline in areas of memory and executive speed.[16] While the results of these studies of rates of cognitive decline do support the cognitive reserve hypothesis, the impact of this association on clinical outcomes is still unclear. Larger prospective studies of longer duration will need to be completed to answer this question.
Cognitive Reserve and Survival with Alzheimer's
On the basis of the studies cited thus far, we would expect more highly educated people, who are diagnosed with Alzheimer's later in the disease process, to have shorter average survival after diagnosis than those with lower education. In a systematic review on this subject, Paradise et al. actually found no association between education and post-diagnosis survival in Alzheimer's. While this would seem to contradict the hypothesis of cognitive reserve, the authors discussed why this is not necessarily the case. The reviewed studies looked at all-cause mortality, not Alzheimer's disease-specific mortality. Because higher education is associated with better health and survival in general, the use of all-cause mortality may have limited the observed differences in survival between the more and less educated groups with Alzheimer's.3
STRUCTURAL AND FUNCTIONAL EVIDENCE FOR COGNITIVE RESERVE HYPOTHESIS
In addition to considerable clinical evidence that supports the cognitive reserve hypothesis, there is also structural and functional evidence that adds more objective support. If it is true that highly educated people can compensate for a greater degree of neurodegenerative pathology before expressing clinical symptoms of dementia, autopsy findings should confirm this association. Roe and her colleagues studied this question by reviewing over 1500 patients whose Alzheimer's was confirmed by autopsy. They were enrolled in designated Alzheimer's Disease Centers throughout the United States and therefore had standardized cognitive testing and historical data available prior to death. Approximately 80% had clinically diagnosed dementia prior to death. The amount of neuritic plaques was measured and categorized for each patient according to a Neuritic Plaque Rating Scale. The researchers found that at each level of neuritic plaque burden, subjects with higher education were less likely to have a clinical diagnosis of dementia. The difference was most profound at the lower levels of plaque burden, where the compensatory effects of cognitive reserve may be the most effective.[17] As Alzheimer's progresses to more severe stages the cognitive reserve will be overwhelmed, limiting the clinical difference between lower and higher educated patients. (Fig. 4)
To look at neurodegenerative changes of Alzheimer's, it is now possible to use PET imaging in living individuals using carbon-11 labeled Pittsburg Compound B, which binds specifically to the fibrillar β-amyloid protein. This protein is the characteristic finding in the neuritic plaques of brain tissue in patients with Alzheimer's, and this imaging technique makes it possible to estimate the degree of neurodegenerative changes. Roe and her colleagues also studied the correlation of cognitive function, Pittsburg Compound uptake, and educational level. They found that in patients with a similar degree of Pittsburg Compound uptake, higher educational level predicted significantly higher performance on multiple global measures of cognitive function.[18] These findings support the cognitive reserve hypothesis by showing that individuals with higher education have better cognitive performance than those with lower education in the face of similar degrees of pathology due to Alzheimer's disease.
Another way to study the effects of Alzheimer's in the brain is to use SPECT scanning to look at regional cerebral perfusion, which has been shown to correlate with the severity of Alzheimer's disease. In 132 patients with clinically diagnosed Alzheimer's disease, Liao et al. looked at the association between education, cerebral perfusion (SPECT imaging), and cognitive performance (Clinical Dementia Rating scale). They found that for a patient with mild or moderate dementia, higher education predicted lower cerebral perfusion, suggesting that while the clinical severity may be similar, more highly educated patients are carrying a larger burden of disease. Looking at the data another way, in patients with similar levels of disease pathology determined by SPECT, higher education was predictive of better cognitive performance.[19] A strength of this study was that cognitive function was assessed using the Clinical Dementia Rating scale which is not impacted by level of education. These findings provide further support for the cognitive reserve hypothesis.
COGNITIVE RESERVE AND THE DIAGNOSIS OF ALZHEIMER'S
The baby boomer cohort is aging, and will be more highly educated than previous generations, making the issue of cognitive reserve more relevant in this patient population. Therefore it is important to understand a patient's background including educational level, occupation, and major leisure activities in order to get a sense of their cognitive reserve. It is no longer sufficient for a social history to include information only on tobacco, alcohol, and drug use.
Though highly effective medical treatment of Alzheimer's is limited at this time, early diagnosis is still useful for several reasons. First, it allows more time to plan care in advance with meaningful participation from the patient. Because Alzheimer's is invariably a progressive disease, families will need to begin planning changes in living arrangements, care giving, and finances, and will also need to complete documents for advanced directives and powers of attorney. Waiting until a crisis develops or until cognitive impairment is moderate to severe will not allow optimal planning. Second, earlier diagnosis will give the patient and family more time to learn about and process the diagnosis. Finally, earlier diagnosis would allow more benefit from existing and developing treatments for Alzheimer's as they become available.
We need to be alert to the possibility of cognitive impairment before it presents as a crisis. This is especially important in our more highly educated patients, as obvious symptoms appear later and may herald more rapid decline than in patients with lower education. Some of the first subtle signs of Alzheimer's may be difficulty with executive function and memory – things that are not tested in depth with the MMSE. In fact, it is possible to have a verified diagnosis of Alzheimer's dementia and still score a 30/30 on an MMSE.[20] Subtle symptoms and signs that may suggest problems with memory could include forgetting appointments and having difficulty following instructions regarding medications. Family may mention that patients are forgetting conversations and events; patients themselves may recognize subtle changes in memory. Loss of executive function may be demonstrated by difficulty with complex activities that the patient could previously accomplish easily, such as shopping, cooking, managing finances, driving, and performing other routine household tasks. The patient may participate less in previously enjoyed hobbies and social activities due to difficulties organizing, planning, and initiating the tasks involved.
One difficulty in making an early diagnosis of Alzheimer's is that – as noted earlier - many of the commonly used cognitive assessment tools such as the MMSE are not sensitive enough to detect early cognitive changes, especially in more educated patients. More in-depth tools are often not practical to use in a busy outpatient office setting. One validated tool that provides more in-depth assessment useful in the outpatient office is the Montreal Cognitive Assessment,[21] which includes more in-depth testing of executive function and memory than the MMSE, and covers other key cognitive domains. It can be completed in 10 minutes and can be a useful tool in the primary care setting. If cognitive impairment is suspected but cannot be easily confirmed in the office, a patient may be referred for more in-depth neuropsychological testing. Such testing can not only determine whether the patient's symptoms are more likely age-related or due to a neurodegenerative process, but can also serve as a baseline for future assessments to determine extent and rate of decline.
In certain patients, a comprehensive geriatric assessment may be useful to help characterize the cognitive and functional deficits using input from patient and family. This assessment can be the basis for further evaluation, management, education, and counseling regarding the changes the patient is experiencing. Quite often the symptoms of early Alzheimer's can overlap with other medical conditions, mental health disorders, and medication side effects. A comprehensive geriatric assessment can be useful in assessing all of these factors.
IPLICATIONS FOR PREVENTION OF ALZHEIMER'S
Given the evidence that cognitive reserve is important, it is useful to ask how it could impact the prevention of Alzheimer's dementia. The evidence supports the idea that intellectual stimulation earlier in life (education, occupation, and leisure activity) creates a more efficient and robust brain that can more easily compensate for the early pathology of Alzheimer's. But can continued mental stimulation in later life prevent or delay the clinical symptoms of Alzheimer's? In fact, there is evidence that specific cognitive training exercises in the elderly can sustain cognitive function. Ball et al. found that this effect was maintained for the 2 years of their study, but their study was not long enough to detect a delay in functional decline or symptoms of dementia.[22] In two observational studies of the same elderly population, Verghese and his colleagues found that participation in cognitive leisure activities (reading, writing, playing music, playing board or card games) was associated with a decreased risk of developing both dementia and amnestic mild cognitive impairment, a frequent precursor of dementia.7, [23]
So should we prescribe these types of intellectual activity to help prevent dementia? There is not sufficient evidence to support specific recommendations on type and amount of activity, but the cognitive reserve hypothesis and supporting observational evidence give us good reason to suggest these activities to our patients throughout life. Cognitive leisure activities are a low-risk intervention we can offer to our patients that may delay the manifestations of a devastating illness for which there are currently no highly effective treatments. From a public health perspective, if we are able to delay the presentation of Alzheimer's in some patients, we could mitigate the high social and economic costs that accompany decline in cognition. Mathematical modeling suggests that if we were able to increase the cognitive reserve in our population by just 5%, we could prevent 1/3 of Alzheimer's cases.[24] These patients would die of other conditions before they developed the clinical symptoms of Alzheimer's.
CONCLUSIONS
With the growth of the elderly population and the medical advances in treating conditions such as cancer and cardiovascular disease, we will be faced with an ever-increasing number of patients suffering from "brain failure" due to Alzheimer's and other neurodegenerative diseases. The cognitive reserve hypothesis suggests that these patients will be harder to diagnose until later in their disease, as the baby boomers are more highly educated than previous generations. If diagnosis is delayed, there will be less time for patients and families to prepare for the changes ahead and to make use of available therapy and counseling. The available evidence suggests that we should encourage all of our aging patients to actively engage in cognitively stimulating activities as they grow older, perhaps allowing them to live a natural life span without suffering the devastating effects of advanced dementia. Physicians should take subtle signs and symptoms of cognitive impairment seriously and offer further evaluation to patients when the limitations of time or basic screening tools do not allow a clear diagnosis to be made.
References
[1] Federal Interagency Forum on Aging related Statistics: Older Americans 2008: Key Indicators of Well-Being. http://www.agingstats.gov/ (accessed July 12, 2009).
[2] Plassman BL, Langa KM, Fisher GG, et al. Prevalence of dementia in the United States: The aging, demographics, and memory study. Neuroepidemiology 2007;29:125-132.
[3] Paradise MP, Cooper C, Livingston G. Systematic review of the effect of education on survival in Alzheimer's disease. Int Psychogeriatr 2009;21:25-32.
[4] Katzman R. Education and the prevalence of dementia and Alzheimer's disease. Neurology 1993;43:13-20.
[5] Stern Y. Cognitive reserve and Alzheimer disease. Alzheimer Dis Assoc Disord 2006;20:112-117.
[6] Andel R, Vigen C, Mack WJ, et al. The effect of education and occupational complexity on rate of cognitive decline in Alzheimer's patients. J Int Neuropsychol Soc 2006;12:147-152.
[7] Verghese J, Lipton RB, Katz MJ, et al. Leisure activities and risk of dementia in the elderly. N Eng J Med 2003;348:2508-2516.
[8] Scarmeas N, Stern Y. Cognitive reserve: Implications for diagnosis and prevention of Alzheimer's Disease. Curr Neurol Neurosci rep 2004;4:374-380.
[9] Hall CB, Derby C, LeValley A, et al. Education delays accelerated decline on a memory test in persons who develop dementia. Neurology 2007;69:1657-1664.
[10] Koepsell TD, Kurland BF, Harel O et al. Education, cognitive function, and severity of neuropathology in Alzheimer disease. Neurology 2008;70:1732-1739.
[11] O'Bryant SE, Humphreys MA, Smith GE, et al. Detecting dementia with the Mini-Mental State Examination in highly educated individuals. Arch Neurol 2008;65:963-967.
[12] Langa KM, Larson EB, Karlawish JH, et al. Trends in prevalence and mortality of cognitive impairment in the United States: Is there evidence of a compression of cognitive morbidity?
[13] Ngandu T, von Strauss E, Helkala EL, et al. Education and dementia: What lies behind the association? Neurology 2007;69:1442-1450.
[14] Bruandet A, Richard F, Bombois S, et al. Cognitive decline and survival in Alzheimer's Disease according to educational level. Dement Geriatr Cogn Disord 2008;25:74-80.
[15] Wilson RS, Li Y, Aggarwal NT, et al. Education and the course of cognitive decline in Alzheimer disease. Neurology 2004;63:1198-1202.
[16] Helzner EP, Scarmeas N, Cosentino S, et al. Leisure activity and cognitive decline in incident Alzheimer's Disease. Arch Neurol 2007;64:1749-1754.
[17] Roe CM, Xiong C, Miller P, et al. Interaction of neuritic plaques and education predicts dementia. Alzheimer Dis Assoc Disord 2008;22:188-193.
[18] Roe CM, Mintun MA, D'Angelo G, et al. Alzheimer Disease and cognitive reserve: Variation of education effect with carbon 11-labeled Pittsburg Compound B uptake. Arch Neurol 2008;65:1467-1471.
[19] Liao YC, Liu RS, Teng EL et al. Cognitive reserve: A SPECT study of 132 Alzheimer's Disease patients with an education range of 0-19 years. Dement Geriatr Cogn Disord 2005;20:8-14.
[20] Shiroky JS, Schipper HM, Bergman H, et al. Can you have dementia with an MMSE score of 30? Am J Alzheimers Dis Other Demen 2007;22:406-415.
[21] Nasreddine ZS, Phillips NA, Bedirian V et al. The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. J Am Geriatr Soc 2005;53:695-699.
[22] Ball K, Berch DB, Helmers KF. Effects of cognitive training interventions with older adults. JAMA 2002;288:2271-2281.
[23] Verghese J, LeValley MA, Derby C et al. Leisure activities and the risk of amnestic cognitive impairment in the elderly. Neurology 2006;66:821-827.
[24] De la Fuente-Fernandez R. Impact of neuroprotection on incidence of Alzheimer's Disease. PloS One 2006 Dec 20;1:e52.