 Click to Print Adobe PDF
Click to Print Adobe PDF
|
Summer 2009 - Vol.4, No.2
SWINE INFLUENZA 2009
A LESSON IN HOW NEW INFLUENZA VIRUSES EMERGE
Joseph M. Kontra, M.D.
Infection Specialists of Lancaster
|
 |
Abstract
While scientists have been preparing for the specter of an Avian Influenza pandemic, this year we have been challenged and tested by the evolution and emergence of a new novel strain of Influenza A that began in Mexico in March 2009. This new swine-origin influenza A strain is the latest pandemic threat to global health. The magnitude and severity of this new strain have yet to be fully realized. This paper discusses the mechanism by which new influenza A strains emerge, the human and animal variables involved, and implications for laboratory testing and vaccine development.
Virology and Nomenclature
Influenza A virus is a single-stranded, negative sense RNA virus of the family Orthomyxoviridae. Its genome consists of eight separate genetic segments that together encode ten important proteins. Each genetic segment has its own nucleocapsid. As we shall discover, this unique configuration is a major reason for the dynamic and rapidly evolving nature of this pathogen.
Influenza viruses are classified on the basis of their core protein (A, B, or C), their species of origin (swine, bird, etc.), their geographic origin (Spanish, Asian, etc.), strain number, and year of isolation. In addition, Influenza A viruses are further sub-classified on the basis of two key surface glycoproteins: Hemagglutinin (HA) and Neuraminidase (NA), which play key roles in the pathogenesis of influenza infection. Sixteen HA and nine NA types have been identified.
The last major pandemic in 1968-1969 was due to Influenza A/Hong Kong/H3N2. The Avian flu strain, which I discussed in the audio portion of this Journal in Volume 1, Issue 2, is referred to as Influenza A/Avian/H5N1, and is still struggling to emerge as a pandemic pathogen. The 2009 post-seasonal outbreak of influenza A has been classified by the CDC as Swine-origin influenza A (H1N1), or swine-origin influenza virus, S-OIV.
Historical Perspective
There have been 31 well-documented pandemics of influenza since 1580, with a highly variable inter-pandemic interval that averages 27.5 years.[1] It has been 41 years since the last major pandemic in 1968, which was due to Influenza A/Hong Kong/H3N2. Since 1977, influenza subtypes H3N2 and H1N1 have remained endemic in human populations. These strains are the ones responsible for the yearly seasonal influenza epidemics, and the ones that drive annual reformulations of the influenza vaccine. It is worth remembering that these strains of seasonal human influenza kill approximately 36,000 Americans annually, resulting in a cumulative death toll that exceeds the total during the infrequent pandemics.
Pandemics of influenza are characterized by the rapid global spread of severe disease unconstrained by the usual seasonal timing. There are usually multiple waves of disease after the initial spread, with high attack rates in all age groups, and high mortality rates, particularly in the young. The H1N1 pandemic of Spanish influenza during 1918-1919, for example, devastated the globe in three distinct waves, infecting an estimated 30% of the world's population, and killing 21 million individuals, including 549,000 in the U.S.[2]
Swine Flu
Swine influenza was first isolated from humans in 1974. A significant outbreak of Swine Flu occurred in soldiers in Fort Dix, New Jersey in 1976.[3] Thirteen cases and one death were reported. An analysis of swine influenza illness from 1958-2005 demonstrated 37 human cases.[4] The cry for the rapid development of a vaccine after the Fort Dix incident, and its distribution to a large portion of the U.S. population was then associated with cases of Guillain-Barré Syndrome, a lesson about rush to judgment not to be forgotten.
This March in Mexico, three clusters of acute respiratory illness were identified. Epidemiologic investigation demonstrated a novel influenza A virus as the pathogen, S-OIV (H1N1). As of May 13, 2009, over 5700 laboratory confirmed cases have occurred in 33 countries. In Mexico 2059 cases with 56 deaths have been confirmed. In the U.S., 45 states have reported a total of 3352 cases with 3 deaths.[5]
To better understand how such sudden and sometimes devastating disease can develop, we must explore the fascinating mechanism that governs the evolution of this virus. We must also understand the critical role of animals, and of human-animal contact.
Influenza in Animals
Where does the flu go in the summer? While it is true that in tropical climates, human influenza can be transmitted year round, animals play a key role in the global ecology and epidemiology of influenza. While influenza B and C are human viruses, in the case of influenza A, the animal kingdom plays a crucial role.
The natural reservoir for all type A influenza is aquatic birds. Many other species, however, can harbor the virus by virtue of having the appropriate respiratory epithelial cell receptors needed for infection. Though each influenza A strain has a tropism for a specific animal, many avian species as well as mammals, particularly swine, can be co-infected with multiple strains of influenza A virus simultaneously from different species.[6]
Genetic Re-Assortment
The co-infection with multiple strains, combined with the genomic structure of the virus, are the engines that drive evolution of the influenza virus at such a frenetic pace. In a respiratory epithelial cell of a pig infected with multiple strains of influenza A virus, the eight separate encapsulated genetic segments from each virus co-mingle in the cytoplasm. During viral assembly, genetic components can then be combined, or re-assorted, to create an influenza A strain with a unique hybrid of combined genetic segments: a novel strain of the flu.
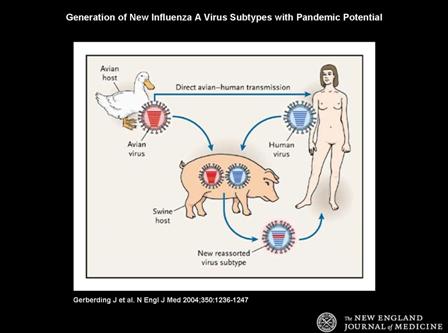 |
(Fig. 1) Diagram illustrating the development of a novel virus by re-assortment of viral genetic material from multiple sources. Gerberding J et al. N Engl J Med 2004;350:1236-1247.
Copyright © 2004 Massachusetts Medical Society. All rights reserved. |
Not all of these experiments of nature are viable, of course. Many re-assorted strains are either not capable of efficient reproduction, not contagious to humans, or not virulent. From time to time, however, the resultant novel strain is at once replicatively fit, virulent, and contagious to humans. Thus is born a potential pandemic threat.
As would be anticipated from the above discussion, novel influenza strains tend to evolve and emerge in rural areas where there is close contact between humans and animals. This is the next necessary variable in the pandemic equation. It is the reason for justifiable concern about the densely populated regions of southeast Asia where close human co-habitation with birds and swine is the norm. It may also explain the genesis of the S-OIV (H1N1) in a country that harbors one of the most concentrated pork producing industries on the planet.
The S-OIV (H1N1) strain genome has been analyzed at the CDC. This truly unique strain has been determined to be a hybrid of swine, human, and avian influenza A viruses.[7]
Implications for Laboratory Testing
Once a clinical influenza outbreak is identified, there remains the task of defining the specific pathogen. A new strain of Influenza A may not react to the protocols for rapid testing that are available. Appropriately collected and transported specimens are first tested using real-time polymerase chain reaction (RT-PCR) methods against known circulating strains of Influenza A. Assays specific for influenza A, B, H1 and H3 targets are employed at the State Lab level.
The current swine-origin influenza A (H1N1) strain reacts to the RT-PCR assay for influenza A, but not with the H1 or H3 assays. This pattern of reactivity would then define the viral isolate as a novel influenza A strain. Final confirmation as an S-OIV (H1N1) is then carried out at the CDC. The readily available rapid influenza antigen assay can identify potential influenza A infections locally. It is important to point out that point of care (office or clinic) testing is not recommended due to the elevated bio-safety level requirements for testing specific to the S-OIV.[8]
Implications for Vaccine Development and Production
Strain surveillance supervised by the World Health Organization is an ongoing process. Data are summarized twice a year, in preparation for flu seasons in both the northern and southern hemispheres. A decision as to which vaccine components to include in the six month production runs is based on these surveillance results. The 2008-9 northern hemisphere vaccine contained 3 strains not previously included in prior production runs: A/Brisbane/59/2007(H1N1), A/Brisbane/10/2007(H3N2), and B/Florida/4/2006. Nine companies around the world, based on WHO/CDC/FDA recommendations, carry out production currently.
In the setting of a pandemic, however, vaccine development requires much more time. The novel strain must first be isolated and characterized. The decision to embark on emergent pandemic vaccine preparation must also include consideration of the severity of disease, which often cannot be predicted at the onset. By definition, vaccine development and deployment cannot precede the onset of human disease, as is the case with seasonal influenza. Recall the obstacles to the development of a vaccine for Avian H5N1, including the co-existence of multiple sub-strains of circulating virus, problems with antigen potency, adjuvant use, etc. Subsequent preparation of vaccine, according to WHO estimates, could then take 4-6 months.[9] In addition, emergency preparation of a pandemic vaccine would detract from production of seasonal vaccine, with its own potential deleterious consequences.
Conclusions
Three variables are key to the development of new influenza A viruses. The first is the unique genomic makeup of influenza A involving eight encapsulated genetic segments. The second is the ability of influenza strains from different species to simultaneously infect certain mammalian cells, providing a crucible in which potentially pandemic novel strains of flu are forged by genetic re-assortment. The third is the requirement of close contact between humans and animals that facilitates the inter-species transmission which fans the pandemic flame.
The challenges of managing the swine H1N1 potential pandemic are many, and have to a significant extent been both aided and compounded by our preparation for the threat of avian H5N1 influenza. Dissemination of information from public health officials is now seamless and instantaneous. But the digital age of real-time information on cable news and the internet regarding case and mortality counts, and endless 'what if' scenarios, can lead to unwarranted anxiety and even panic. Our preparations for an accelerated ramp up of vaccine production and distribution also leaves us vulnerable to its premature launch for a pandemic of relatively mild intensity, which could burn itself out before vaccine distribution could even begin. Epidemiology is well-suited to describe ongoing pandemics in real time and to analyze those that are past. The capricious nature of disease epidemics, however, always leaves the uncertainty of the future just out of the grasp of epidemiologic science.
What is certain is that pandemics of influenza have been with us throughout history, and will continue to plague the human race. Hopefully the latest outbreak of swine H1N1 flu will be little more than a test of our preparedness, and one from which we will learn valuable lessons for the future.
References
[1] Sydenham T. Influenza: of the epidemic diseases. In: Major RH, ed. Classical Descriptions of Disease. Springfield, Ill: Charles C. Thomas; 1955:201.
[2] Crosby, AW. Epidemic and Peace, 1918. Part IV. Westport, Conn: Greenwood Press 1976.
[3] Gaydos, JC et al. Swine influenza A at Fort Dix, New Jersey (January-February 1976). I. Case finding and clinical study of cases. J Infect Dis 1977; 136 Suppl:S356.
[4] Myers, KP et al. Cases of swine influenza in humans: a review of the literature. Clin Infect Dis 2007; 44:1084.
[6] Scheld, WM (ed). Emerging Infections. 2007; 7:1-22.
[7] United Stated Centers for Disease Control and Prevention. CDC Briefing on Public Health Investigation of Human Cases of Swine Influenza, April 23, 2009.
Joseph M. Kontra M.D.
Infection Specialists of Lancaster
2106 Harrisburg Pike, Suite 301
Lancaster, PA 17601
717-544-3517
jmkontra@LGHealth.org