 Click to Print Adobe PDF
Click to Print Adobe PDF
Summer 2009 - Vol.4, No.2
SCREENING FOR CHRONIC KIDNEY DISEASE:
CLINICAL BENEFIT AND BURDEN
Laurence E. Carroll MD, FASN
Hypertension and Kidney Specialists
|
 |
Background
I have previously written in this Journal about the role of the estimated Glomerular Filtration Rate (eGFR) calculated from the Modification of Diet in Renal Disease (MDRD) equation, and the associated classification of Chronic Kidney Disease (CKD) into Stages 1-4.[1] That article was presented in response to the 2002 Kidney Disease Outcomes Quality Initiative (KDOQI), a project of the National Kidney Foundation and the broad-based "kidney community," which defined those Stages.
In January 2005, Lancaster General Hospital added a creatinine-based calculated eGFR value to its blood chemistry panels (BMPs & CMPs). Since then, Pennsylvania and other states have mandated that all clinical laboratories must provide eGFRs, with the result that a national initiative has begun for a "standardized creatinine," to try to provide eGFR results that have greater accuracy and reproducibility.
Benefit
All this activity has raised awareness of CKD and has helped to improve care by allowing earlier referral and the development of new CKD Clinics.[2] Aggressive management of anemia, hyperparathyroidism, and Vitamin D deficiency has become more common, and use of arterio-venous fistulas (AVF) has increased. AVFs are the optimal vascular access for hemodialysis, and their use now exceeds the Healthy People 2010 goal of 50%.[3] (Our local use is >70% - the highest in the Regional Kidney Network.) We're hoping these achievements will pay dividends in future years by lowering mortality rates, especially in Cardiovascular Disease (CVD) for which CKD is now accepted to be an independent risk factor.[4]
Burden
Balancing these benefits is the controversy that has arisen about a "false epidemic" of CKD. Some of this concern was generated by a purported 30% increase in CKD in the last 10 years. According to the National Health and Nutrition Examination Survey (NHANES ) for 2004, the incidence of CKD in the segment of the general population more than 20 years old increased from 10% to 13% compared with previous surveys. This alarming change was attributed to the aging of our population, and to the increased incidence of Diabetes and Obesity.[5] The most heated debate has come over Stage 3 CKD which is the largest CKD sub-population, and makes up 56% of all those with CKD. If the 13% incidence of CKD cited above for all adults in the U.S over 20 years is accurate, there are about 29 million people with CKD, of whom 16 million - 56% - have CKD Stage 3.[6]
The controversy over Stage 3 CKD starts with its definition: an eGFR of 30-60 cc/min, with no requirement for an abnormal imaging study (usually Kidney Ultrasound) or urinary abnormality (albuminuria/proteinuria, hematuria, or both). Critics point out that age related decreases in GFR and kidney function have been known for over 50 years, and that previous population studies have suggested a 10% decrease in GFR every 10 years after the third decade of life.[7] This means that by eGFR alone, 38% of individuals over 70 years will be classified as having CKD.[8]
Since only 24% of Stage 3 CKD patients have albuminuria/proteinuria, 76% of these patients are in this category only because of an eGFR of 30-60 cc/min – a finding that may be more the result of aging than of an actual "disease."[9]
Therapeutic Focus
The absence of albuminuria/proteinuria is an important consideration, because it appears to be a critical marker for the risk of progressive CKD in most diabetics and other patients.[10] A recent Chinese study showed that when Stage 1-2 CKD (GFR >60 cc/min) was associated with albuminuria the risk of developing progressive CKD was increased; without albuminuria, the risk was not increased even in Stage 3 CKD.[11] Previous studies in diabetics (the RENAAL trial - Reduction of Endpoints in Non-Insulin Dependent Diabetes Mellitus with Angiotensin II Antagonist Losartan) have shown that proteinuria, especially above 1 gram urinary protein per gram of urinary creatinine, indicates a high risk for progressive CKD.[12] Reduction of proteinuria in diabetic kidney disease has been shown to be beneficial. In the non-diabetic population, the use of angiotensin converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), and aldosterone blockers (alone or in combination), is a matter of ongoing studies.[13]
Recommendations
The protocol that accompanies this article, "Primary Care in Early Chronic Kidney Disease," is based on the Kidney Early Evaluation Program of the National Kidney Foundation's (KEEP-NKF) (Table 1);[14] the 2008 Guidelines for CKD of the Royal College of Physicians;[15] and some of my personal opinions.
It designates specific populations to screen, and the survey tools to use: blood pressure (BP), serum creatinine, eGFR, urinalysis, and urine albumin/creatinine ratio (ACR). An appendix will be made available at the LGH website for normal values and further information.
Although some have proposed that only stage 4 CKD patients should be referred to a nephrologist to prepare them for dialysis or transplant, such a plan could delay therapy for potentially reversible glomerulonephritis or vasculitis. The protocol therefore focuses on two factors that differentiate patients who need to be referred for specialty care from those who only need to be followed in the primary care office. First, the protocol suggests that all patients with "glomerular" hematuria (dysmorphic RBCs in the urine and RBC casts), should be referred for evaluation, at which time kidney biopsy should be considered. Those with significant proteinuria should be seen with particular urgency.
Second, referral to nephrology is not necessary in older patients with Stage 3 CKD if they have no structural abnormality on imaging studies, have a normal urinalysis, a normal albumin/creatinine ration (ACR) or normal microalbuminuria (abnormal >30 mcg/mg creatinine). They can be followed with measurements of blood pressure and serum creatinine at 3−6 month intervals along with the other primary care goals stated.
Conclusions
Nephrology needs to partner with primary care providers to deal with the burden of CKD in our society. Using the tools available such as this protocol, we should be able to provide appropriate and effective care to enhance outcomes. These measures will slow progression to the more advanced Stages of CKD, where costly and somewhat limited renal replacement therapies become the only alternative.
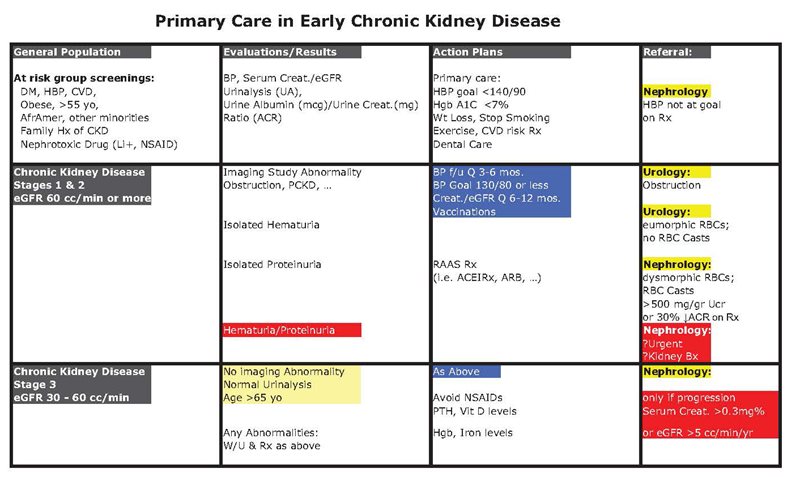
| I would like to acknowledge Dr Pat Eckert's joint authorship on this table. |
References
[1] Carroll LE. The stages of chronic kidney disease and the estimated glomerular filtration rate. J Lanc Gen Hosp. 2006: 1:64-69
[2] Jaar BG, Khatib R, Plantinga L, Boulware LE, and Powe NR: Principles of Screening for Chronic kidney Disease. Clin J AM Soc Nephrol 2008; 3:601-609
[3] Collins AJ, Foley RN, Herzog C, et al: Excerpts from the United States Renal Data System 2008 Annual Data Report. Am J Kid Dis 2009 (Suppl.I); 53: S1-S374
[4] Go AS, Chertow GM, Fan D, McCulloch, Hsu CY: Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Eng J Med 2004;351: 1296-1305
[5] Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, Eggers P, Van Lente F, Levey AS: Prevalence of chronic kidney disease in the U.S.. JAMA 2007; Nov 7;298(17):2038-47
[6] Glassock RJ and Winearls C: An epidemic of chronic kidney disease: fact or fiction? Nephrol Dial Transplant 2008; 23: 1117-1121
[7] Lindeman RD, Tobin JD, Shock NW: Association between blood pressure and the rate of declime in renal function with age. Kid Int 1984;26(6):861-8
[8] Coresh J, Stevens LA, and Levey AS: Chronic kidney disease is common: What do we do next? Nephrol Dial Transplant 2008;23: 1199-1125
[9] De Jong PE and Gansevoort RT: Fact or fiction of the epidemic of chronic kidney disease- let us not squabble about estimated GFR only, but also focus on albuminuria. Nephrol Dial Transplant 2008;23: 1092-1095
[10] Bakris GL:Slowing Nephropathy Progression:Focus on Proteinuria Reduction. Clin J AM Soc Nephrol 2008: 3:S3-S10
[11] So WY, Kong APS, Ma RCW, Ozaki R, Szeto CC, Chan NN, Ng V, Ho CS, Lam CWK, Chow CC, Cockram CS, Chan JCN, Tong PCY: Glomerular filtration rate, Cardiorenal endpoints, and all-cause mortality in type2 diabetic patients. Diabetes Care 2006; 29(9): 2046-2052
[12] Eijkelkamp WBA, Zhongxin Zhang, Remuzzi G, Parving HH, Cooper ME, Keane WF, et al. Albuminuria is a target for renoprotective therapy independent from blood pressure in patients with type 2 diabetic nephropathy: post hoc analysis from the reduction of endpoints in NIDDM with the angiotensin II antagonist Losartan (RENAAL) Trial. J Am Soc Nephrol 2007;18: 1540-1546
[13] Berns JS: Is angiotensin converting enzyme inhibition and angiotensin receptor blockade combination therapy better than monotherapy and safe in patients with CKD? Am J Kid Dis 2009:53(2):192-196
[14] Brown WW, Collins A, Chen SC, et al: Identification of persons at high risk for kidney disease via targeted Screenings: The Kidney Early Evaluation Program (KEEP) Kid Int Suppl 2003; 83: S50-S55
[15] Chronic kidney disease, National Clinical Guideline for early identification and management in adults in primary and secondary care. National collaborating centre for chronic conditions London RCP Sept 2008 (www.rcplondon.ac.uk/pubs/…)
Neither Dr. Carroll nor any member of his immediate family have any relevant relationships to disclose with any corporate organizations associated with the manufacture, license, sale, distribution or promotion of a drug or device.
Laurence E. Carroll, M.D., F.A.S.N.
Hypertension Kidney Specialists
2112 Harrisburg Pike - Suite 2112
Lancaster, PA 17604
717-544-3232
lecjtc@comcast.net