 Click to Print Adobe PDF
Click to Print Adobe PDF
Summer 2009 - Vol.4, No.2
PET/CT: CURRENT PERSPECTIVE
Thomas Brooks, D.O.
Radiologist, Section Chief, Division of Nuclear Medicine
Lancaster Radiology Associates
|
 |
Background
It may surprise some to know that PET, or positron emission tomography, has been around since the 1970's. In the 70's and 80's, it was mainly used for research, requiring a multimillion dollar combination of a scanner, a cyclotron to produce the radioactive agents, and physicists to run both. In the 1990's, PET became a clinical reality due to technological advances in scanner design, as well as market ingenuity. Of course, changes in insurance and Medicare payments and allowances played a role. The combination of these forces allowed the current rapid advance in clinical utilization of PET for the detection and treatment of many types of cancer.
Methodology
Demystifying PET is often useful to clinicians, patients, and, radiologists. PET imaging occurs when a patient is injected with a positron emitting agent such as Fluorine-18, tagged with a glucose substrate, FDG, fluorodeoxyglucose. The glucose localizes at areas of increased metabolism such as tumors, and inflammation, while the agent F-18 decays by positron reaction and gives off photons. These are detected in the PET scanner and localized, which produces an image. Attenuation abnormalities occur during scanning that degrade the image, and PET scanners without CT use a radioactive source in the scanner to create an image of the body as a background, and also help "correct" the images. It was not long before scientists realized that this correction process could be done with a CT scanner. The result was PET/CT, true fusion of one imaging modality to another. This fusion technology allows the highly sensitive PET scan to detect metabolic signals from active cancer cells, while CT reveals detailed anatomy of the location, size, and shape of abnormal cancer or metabolically active areas. Form meets function.
In the typical PET/CT scanner, the CT scan of the body is done first, usually in a minute or so, followed by the PET scan. Advantages of PET/CT over standard PET, in addition to simultaneous anatomic image fusion, are significant decreases in scan times by 30-50%, yielding increased patient comfort, and less patient motion artifacts. It should be noted that there are no allergic reactions in PET and 90% of the radioactivity is gone from the patient by the time the patient leaves the scan area, so families are generally safe with standard precautions.
 |
| Figure 1. PET/CT scanner seen from above: Philips Gemini TF |
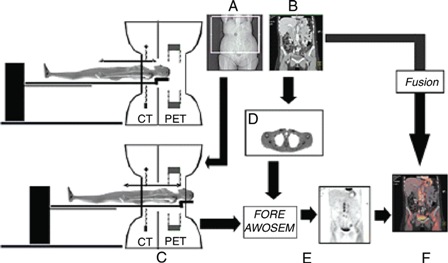 |
| Figure 2. Typical imaging protocol for combined PET/CT: Topogram (A), or scout scan, is obtained for positioning. Spiral CT scan (B) is obtained, followed by a PET scan (C) over the same axial image as B. CT-based attenuation-correction factors are generated (D), and attenuation-corrected PET emission data are reconstructed (E). Finally, fused CT and PET images are displayed (F). (Provided by RSNA Journals.org) |
Clinical Applications
In recent years, proof of the increased accuracy of PET/CT over standard PET has been so conclusive, that even though the first clinical PET/CT wasn't produced until 2000, manufacturers were no longer producing standard PET scanners by 2007, despite the obvious increased cost of adding the CT scanner to the system.[3]
Medicare has traditionally covered the use of PET for workup of cancer, including colorectal, esophageal, head and neck, non-small cell carcinoma of the lung, lymphoma, melanoma, breast, as well as thyroid and cervical cancers. Coverage has now been added to include the use of PET for solitary pulmonary nodules (SPNs). [*Editor's Note]Also covered are non-oncologic applications of myocardial viability, dementia, and refractory seizures. Sensitivity, specificity, and accuracy of PET and PET/CT for most tumors are typically greater than 80-90%.[3]
PET as a decision making tool can help to stage disease, thereby avoiding unnecessary lung surgery by up-staging disease, or making surgery an option by down-staging the extent of disease. PET can direct radiation oncologists to increase the area to be radiated when more cancer is detected than expected, or to decrease the radiation field, as can occur when less tumor is detected than expected from the consolidated lung seen on a routine CT scan. Many oncologists now use PET alone to follow treatment for certain lymphomas, rather than using traditional serial CT imaging. And due to the efforts of the National Oncologic PET Registry (NOPR), Medicare has issued a preliminary (March 2009) statement that offers payment and coverage for PET imaging of pancreatic, ovarian, testicular, prostatic, small cell lung, sarcoma, and solid tumors. This was accomplished as a result of overwhelming evidence from scientific studies of the power of PET.
The NOPR results reveal the current clinical impact of PET. The NOPR started in May, 2006. In May, 2008, the results of 40,863 PET studies performed at 1,368 centers were tabulated. PET was responsible for a change in intended management for 38% of patients. The impact on intended management for patients with a known cancer was consistent across all cancer types.[4] This result was striking, and certainly promising.
Going forward, as PET/CT software and hardware become more refined, the resolution of PET detection will continue to improve. Whereas a few years ago, a detectable lung cancer had to have a certain critical mass, or a size of typically 10 mm, it is now possible to see cancerous lung nodules in the range of 3-4 mm, depending on the patient and the activity of the tumor.
Confusion still exists over the need for sentinel lymph node surgery in the age of PET. There must be a threshold number of cancer cells to be detected by the scanner, so PET/CT is not flawless, and will not replace the eyes of a pathologist, who can determine if just a few, or even one cancer cell exists. Breast cancer and melanoma, because of their typical locations in the body and lymphatic spread, are well suited to initial evaluation by sentinel sampling. In response to ongoing clinical frustration, and confusion among many physicians who feel overwhelmed by the options for different modalities of imaging, the Journal of Nuclear Medicine published a special supplement entitled "PET/CT in Cancer Patient Management." This reference is available for purchase online.[5]

Fig. 3. PET/CT performed using Philips' Gemini TF identifi es lymphoma in a pelvic lymph node. (Provided by Philips Medical Systems) |
Summary
In just a few years PET has evolved from its rather stagnant status in the 1970s and 1980s to what is now widespread utilization for detecting, staging, and following almost all types of cancer. As this imaging technique takes place at an atomic and cellular level, PET and now PET/CT have helped change Nuclear Medicine into a field many now term Molecular Imaging. New PET agents, substrates, and antibodies are currently being tested not only for cancer, but for neurological, cardiac, and other applications.
References
[1] Cerfolio, RJ et al. Ann of Thor Surg 2004;78:1017-1023: The accuracy of integrated PET-CT compared with dedicated PET alone for the staging of patients with nonsmall cell lung cancer.
[2] Branstter, B. et al. Radiol 2005; 235: 580-586: Head and neck malignancy: Is PET/CT more accurate than PET or CT alone?
[3] Gustav K Von Schulthess, MD, Phd. Ch. 34-57. Molecular Anatomic Imaging. 2007 287-515
[4] Hillner, BE, Siegal, BA, et al. Relationship between cancer type and impact of PET and PET/CT on intended management: Findings of the National Oncologic PET Registry. J Nuclear Med 2008;49:1928-1935
[5] J Nuclear Med 2007;48, Issue 1, Jan. suppl.
[*Editor's Note] Despite the extra cost of using the CT machine, payments for PET and PET/CT are exactly the same, and they are approved for the same indications.
Neither Dr. Bentz nor any member of his immediate family have any relevant relationships to disclose with any corporate organizations associated with the manufacture, license, sale, distribution or promotion of a drug or device.
Thomas Brooks, D.O.
Radiologist, Section Chief, Division of Nuclear Medicine
Lancaster Radiology Associates
555 N. Duke Street
Lancaster, PA
717-299-4173
tabrooks@LGHealth.org