 Click to Print Adobe PDF
Click to Print Adobe PDF
|
Winter 2008 - Vol.3, No.4
TUNNELED CATHETER PLACEMENT IN THE MANAGEMENT OF MALIGNANT ASCITES AND PLEURAL EFFUSIONS
Leigh S. Shuman, M.D.
Lancaster Radiology Associates, Ltd.
|
 |
ASCITES
Patients with a variety of abdominal malignancies may develop a troubling and painful complication in the final months of life: intractable ascites. These patients suffer from abdominal pain, shortness of breath, and nausea, and are often unable to engage in the activities of daily living. Theraputic paracentesis is a low risk procedure, but it must be done repeatedly to provide relief from distention and discomfort. Weekly trips to the hospital for repeated paracentesis detract from the patients’ ability to enjoy the little time they have left, and are painful reminders of their disease.
A variety of procedures have been used to treat ascites, including shunts from the abdominal cavity to either the venous system, the stomach, or the urinary bladder; all suffer from substantial morbidity and high failure rates.1 Standard drainage catheters, such as those used to drain abdominal abscesses, are not tunneled, and therefore frequently become infected and must be removed. Tunneled catheters have long been used for peritoneal dialysis, and their percutaneous placement is well-described,2 so it was a logical extension of this technique to use these catheters to allow patients to drain their own ascites. It should be noted that this is an off-label used of these devices.
A Tenckhoff peritoneal dialysis catheter or a similar soft catheter with a cuff (such as the catheters mentioned below) is inserted into the largest collection of ascites under ultrasound and fluoroscopic guidance, and the catheter is tunneled to a convenient location on the abdominal wall.3,4 The peritoneal fluid is drained and the patient and/or caregivers are trained in basic sterile technique for catheter care. Once home, the patient simply places the catheter over the toilet or a suitable container, opens a valve, and allows the fluid to drain out as needed. The catheter end must be kept sterile and cleansed after each use to minimize the risk of infection, so the patients or family must be capable of this task. If not, visiting nurses or the hospice may be utilized. Patients return to the hospital only if problems occur.
Complications are infrequent in most reports and in our own experience. Infection of the tunnel tract or of the ascites, occurs uncommonly, and is usually manageable with antibiotics alone. Less than 5% of catheters have to be removed due to infection. Rarely, loculations may prevent adequate drainage and require catheter removal and re-placement. Leakage of ascitic fluid along the tract, soaking bandages and clothing, can be troubling, but has been successfully treated in most cases by increasing the frequency of drainage or by sclerosing the tract. Patients do need to monitor the output and replace lost fluids with a suitable electrolyte solution.
The average lifespan of patients with malignant ascites is 1–4 months, and most patients die with their catheter in place and functioning. We have heard from a number of families about the profound difference this procedure has made in the last days of these unfortunate individuals.
PLEURAL EFFUSIONS
Rapid accumulation of pleural fluid is a frequent late stage complication of many intrathoracic malignancies, including lung cancer, metastatic disease, and mesothelioma. These patients are troubled by shortness of breath, cough, and pain, and often return to the hospital for frequent thoracenteses.
Pleurodesis is the standard technique for treating malignant pleural effusions by using a variety of sclerosing agents including talc, bleomycin, or doxycycline. However, success rates vary widely in the literature, and the procedure usually involves hospitalization to fully drain the effusion with a chest tube, to introduce the sclerosing agent, to control the pain of the resulting pleural inflammation, and to await cessation of pleural drainage, which indicates that the pleural surfaces are approximated. Again, given the limited lifespan of many of these patients, an outpatient procedure that would permit home drainage would be helpful, and would also allow treatment of those patients who fail pleurodesis.
|
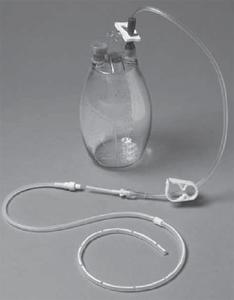
Figure 1. The Pleurx Drainage System (image courtesy of Cardinal Health).
|
Figure 2. The Aspira Drainage System (image courtesy of Bard Access Systems). |
 |

|
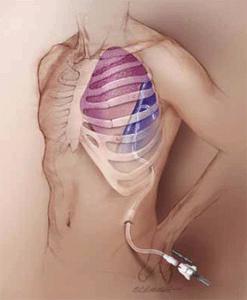
| Figure 3. Typical pleural catheter placement (image courtesy of Bard Access Systems). |
 |
The pleural space differs from the abdominal cavity in significant ways, however. One cannot simply open a catheter to drain into a container, as negative intrathoracic pressure will suck air in and create a pneumothorax, so a one-way valve is required in any drainage system to isolate the pleural space from the atmosphere. There are two commercial catheter systems which satisfy the need for a valved system that is compatible with home suction.
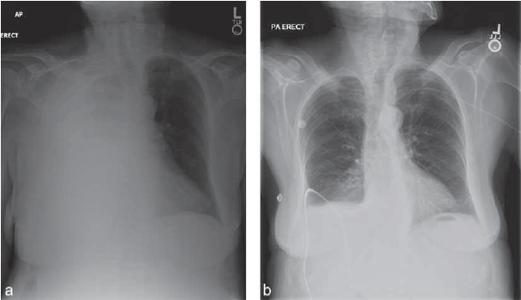
5 The PleurX® catheter (Cardinal Health, McGaw Park, IL) (Fig. 1) and the Aspiria® catheter (Bard Access Systems, Salt Lake City, UT) (Fig. 2) are both FDAapproved for long-term drainage of malignant pleural effusions. They use similar catheters that are placed into the pleural space and tunneled to the upper abdominal wall (Fig. 3). A special valve on the end that can only be accessed by the associated drainage system precludes the introduction of air. We have used both systems, but prefer the Aspira® because the drainage system is substantially less expensive. Though many insurance plans cover the cost of catheter placement, they do not reimburse the cost of the single-use drainage equipment. A typical case is illustrated in Figure 4.
| Figure 4. a) A large right pleural effusion filling virtually the entire right hemithorax. b) After placement of a tunneled drainage catheter, the pleural effusion has resolved. |
|
|
When drainage is successful and the lung re-expands, nearly half of patients will undergo spontaneous pleurodesis, which permits removal of the catheter. Complications are infrequent, but can include infection, pneumothorax from catheter migration, and development of a fibrin sheath around the intrathoracic portion of the catheter that prevents drainage. Care must be taken to limit the amount of fluid removed at any one time to avoid rapid lung re-expansion with the associated pain and coughing that results from reapproximation of the pleural surfaces.6
As with the abdominal catheters, patients, their families, and nursing personnel must be carefully educated in the safe use of these catheters. When this is accomplished, patients report a very high level of satisfaction; they spend much less of their precious time undergoing repeat thoracentesis, and more time with their families.
REFERENCES
1. Pollak JS, Burdge CM, Rosenblatt M, Houston JP, Hwu WJ, Murren J. Treatment of malignant pleural effusions with tunneled long term drainage catheters. J Vasc Interv Radiol 2001;12:201-208.
2. O’Neill MJ, Weissleder R, Gervais DA, Hahn PF, Mueller PR. Tunneled peritoneal catheter placement under sonographic and fl uoroscopic guidance in the palliative treatment of malignant ascites. Am J Radiol 2001;177:615-618.
3. Barnett TD, Rubins J. Placement of a permanent tunneled peritoneal drainage catheter for palliation of malignant ascites: a simplified approach. J Vasc Interv Radiol 2002;13:379-383.
4. Rosenberg S, Courtney A, Nemcek AA, Omary RA. Comparison of percutaneous management techniques for recurrent malignant ascites. J Vasc Interv Radiol 2004;15:1129-1131.
5. Savader SJ. Percutaneous radiologic placement of peritoneal dialysis catheters. J Vasc Interv Radiol 1999;10:249-256.
6. Stather DR, Tremblay A. Use of tunneled pleural catheters for outpatient treatment of malignant pleural effusions. Current Opinion in Pulmonary Medicine 2007;13:328-333.
Neither Dr. Shuman nor any member of his immediate family have any relevant financial relationships with any corporate organizations associated with the manufacture, license, sale, distribution or promotion of a drug or device to disclose.
Leigh S. Shuman, M.D.
Staff Radiologist, Lancaster General Hospital
Lancaster Radiology Associates, Ltd.
P.O. Box 3555
Lancaster, PA 17604
717-544-4900
LSShuman@LGHealth.org