Care of a trauma patient with multiple injuries can pose complex problems of prioritization. For orthopedic injuries, we prefer to perform definitive fixation of all fractures in one trip to the operating room. This approach not only makes the most efficient use of the operating room and the orthopedic surgeon, but it permits the other injuries to be treated promptly, and allows the patient to be mobilized for tests and therapy.
Unfortunately, there are several scenarios in which immediate definitive fixation of all fractures is not best for the patient. In particular, some patients are too unstable from multiple injuries to undergo a sometimes lengthy operation with associated blood loss. This group has a primary indication for DCO - Damage Control Orthopedics.
The Empirical and Physiological Basis for Damage Control Orthopedics
The concept of damage control surgery was initiated by general trauma surgeons who found that some patients with severe injuries were best served by a quick laparatomy to control major bleeding and to pack off areas of diffuse tissue injury.1 German trauma surgeons then applied this principle to fractures of the femur, after noticing that their most severely injured patients seemed to have better survival if their femoral fractures were treated with external fixation as a temporizing measure. If they performed more extensive internal fixation with the standard intramedullary nail, there was a higher incidence of multi-system organ failure.2
Further study led to the “two-hit hypothesis” of the systemic inflammatory response syndrome (SIRS). In this concept of the body’s response to trauma, there is an immediate inflammatory response, and a second insult causes a second, cumulative inflammatory response. The combined levels of inflammatory mediators are then high enough to cause generalized tissue damage and can lead to multi-system organ failure. As distasteful as it may seem to those of us who fix femoral fractures, nailing a femur is a systemic insult that is large enough to fill the role of a second “hit.”3,4,5
The primary inflammatory mediators released after trauma include Interleukins 6 and 8. Any major operative procedure that is carried out while there is still a high level of these mediators has a significant likelihood of serving as the second “hit,” which can push the patient towards multi-system organ failure. Since the levels of IL6 and IL8 remain high for five days after major trauma, we generally wait at least that long after the original injury to perform definitive fixation for severely injured patients. 4,5
Damage Control Orthopedics thus seeks to avoid provoking a severe inflammatory response, and confines itself to more modest goals: sufficient stabilization of fractures to prevent further tissue damage and the possibility of compartment syndrome; and allowing the patient to be mobilized for tests and improved pulmonary care. For most upper extremity injuries, simple external stabilization with splints or a sling will suffice. For closed fractures below the knee, splinting is usually the best option, though there are other considerations to be discussed below.
DCO in Complex Injuries
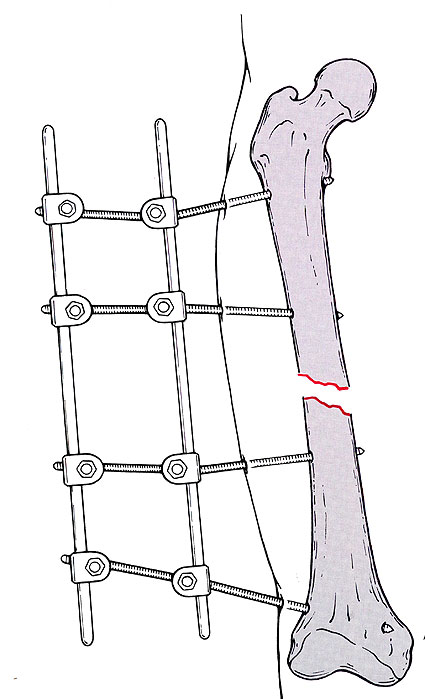
Fractures of the femur are a challenging orthopedic injury. Splinting without traction is not effective because the joint above the fracture, the hip, cannot be immobilized. Traction splints do work, but they apply high pressures to the skin on the dorsum of the foot, are unsuitable for more than several hours, and confine the patient to a recumbent position. Fortunately, external fixation of femoral fractures is rapid, involves very little blood loss, and is not invasive enough to act as a second “hit.” External fixation consists of the percutaneous insertion of 5mm pins into the femur above and below the fracture, which are then connected outside the skin by a series of bars (Figure 1).
The next decision is when to convert temporary fixation to definitive fixation, since inordinate delay raises the risk of infection. As discussed above, it takes at least 5 days for interleukin levels to decline. Clinical research has shown that if definitive repair with an internal rod is completed within 14 days of external fixation, there is no increase in the risk of infection.7 This window of opportunity between 5 and 14 days for definitive treatment of the DCO-treated femur is adequate for the vast majority of trauma patients, but in the occasional patient whose other injuries prevent definitive internal fixation within 14 days, an alternative definitive treatment method, submuscular plating, is used. This is a less biomechanically favorable method of fixation, but it does avoid any contact with the external pin sites in the skin and bone. It uses standard plates and screws, but rather than requiring a large incision, the plate is slid beneath the intact soft tissues through a small incision above or below the fracture, and the screws are then placed percutaneously. In comparison with placing the standard intramedullary nail, submuscular plating is less traumatic, and causes less blood loss. In a patient who is too unstable after external fixation to allow conversion to an intramedullary nail, the external fixation apparatus can be used to maintain the reduction while submuscular plating is carried out.
Patients with a severe intracranial injury that accompanies their orthopedic injury also benefit from DCO. Because the cerebral perfusion pressure is marginal in patients with intracranial hypertension, any drop in their systemic blood pressure may lower cerebral perfusion pressure and compromise brain perfusion. This then leads to increasing ischemic damage of cerebral tissue, leading to more swelling and increased intracranial pressures. Because definitive fixation of fractures, again especially femoral fractures, can result in enough blood loss to incite a minor drop in systemic perfusion pressure, we often employ the principles of DCO to stabilize the fractures and permit the patient to be transferred without compromising cerebral perfusion pressures.8,9
The third indication for DCO protocols is the presence of local soft tissue damage. This principle was first realized in high energy fractures of the distal tibia. (The horizontal articular surface of the distal tibia, as opposed to the medial malleolar portion, is termed the tibial plafond or pilon. Most plafond fractures are high energy injuries that have massive swelling and a tenuous soft tissue envelope because of the lack of muscle around the distal tibia.) At one time, fractures with severe open wounds or extensive closed soft tissue contusions that were immediately treated with definitive open reduction and internal fixation had a frighteningly high infection rate.10,11 This led to the practice of using temporary external fixation to stabilize the fracture and allow monitoring of skin and soft tissue status, followed by definitive fixation 10-21 days after the injury.12 This approach is now commonly used with proximal tibia fractures as well, reducing the concern about exposed hardware and infection. External fixation also allows advanced imaging studies to be obtained, which aid in preoperative planning of incisions and fixation methods for complex periarticular fractures.
Conclusions
DCO has proven to be a powerful tool for the orthopedic surgeon who treats trauma victims. It has improved patient care from systemic, neurologic, and orthopedic viewpoints.
REFERENCES
- Hirshberg A, Mattox KL: ‘Damage control’ in trauma surgery. Br J Surg 1993; 80:1501-150
- Pape HC, Hildebrand F, Pertschy S, et al: Changes in the management of femoral shaft fractures in polytrauma patients: from early total care to damage control orthopedic surgery. J Trauma. 2002;53(3):452-461.
- Keel M, Trentz O: Pathophysiology of polytrauma. Injury2005;36(6):691-709.
- Harwood PJ, Giannoudis PV, van Griensven M, et al: Alterations in the systemic inflammatory response after early total care and damage control procedures for femoral shaft fractures in severely injured patients. J Trauma 2005; 58(3):446-52.
- Pape HC, Grimme K, Van Griensven M, et al: Impact of intrameduallary instrumentation versus damage control for femoral fractures on immunoinflammatory parameters: prospective randomized analysis by the EPOFF Study Group. J Trauma 2003;55(1):7-13
- Smith RM, Giannoudis PV, Bellamy MC, et al: Interleukin-10 release and monocyte human leukocyte antigen-DR expression during femoral nailing. Clin Orthop 2000;373:233-240.
- Harwood PJ, Giannoudis PV, Probst C, et al: The risk of local infective complications after damage control procedures for femoral shaft fracture. J Orthop Trauma 2006; 20(3):181-9.
- Townsend RN, Lheureau T, Protech J, et al: Timing of fracture repair in patients with severe brain injury. J Trauma 1998;44:977-982.
- Giannoudis PV, Veysi VT, Pape HC, et al: When should we operate on major fractures in patients with severe head injuries? Am J Surg 2002;183:261-267
- Teeny SM, Wiss DA: Open reduction and internal fixation of tibial plafond fractures: Variables contributing to poor results and complications. Clin Orthop 1993;292:108-117
- Sirkin M, Sanders R, DiPasquale T, Herscovici D Jr: A staged protocol for soft tissue management in the treatment of complex pilon fractures. J Orthop Trauma 1999;13:78-84
- Marsh JL, Hartsock L. 2005. Fractures of the tibial plateau. Chapter 36 of Orthopedic Knowledge Update: Trauma 3,ed. Michael R. Baumgartner, Paul Tornetta III. Rosemont IL: American Academy of Orthopedic Surgeons.
James H. Carson, M.D.
Orthopedic Associates of Lancaster
170 North Pointe Boulevard
Lancaster, PA 17604
Phone – 717-299-4871
jcbonefixer@comcast.net
Figure 1. Skeletal Trauma: Fractures, Dislocations, Ligamentous Injuries; Browner D., Jupiter J., Levine A., Tafton P.; 1992; page 1554, Figure A. Copyright permission granted by Elsevier.