 Click to Print Adobe PDF
Click to Print Adobe PDF
Summer 2007 - Vol.2, No.2
Edward T. Chory, M.D., F.A.C.S
Lancaster Surgical Group, P.C.
|
 |
ABSTRACT
Operative repair is recommended for patients with paraesophageal hernias because of the risks of obstruction, incarceration, or strangulation. Conventional surgical repair can be accomplished through the chest or the abdomen, but as experience with laparoscopic repair has increased, this technique is becoming the preferred approach. This report describes our experience with 20 patients undergoing elective laparoscopic surgery to repair paraesophageal hernias.
INTRODUCTION
Paraesophageal hiatus hernias are relatively uncommon, but their frequency is increasing, and they now account for 5-10% of all hiatus hernias. It is important for clinicians to be aware of the unique clinical characteristics of paraesophageal hernias, as well as the current controversies concerning the management of this complex condition.
Types of Gastroesophageal Hernias
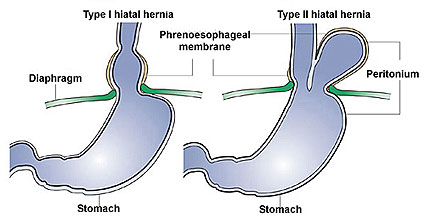
It is estimated that 10% of the general population have hiatus hernias, of which more than 90% are sliding hiatus hernias (Type I). These hernias are associated with laxity of the phrenoesophageal ligament, which allows displacement of the gastroesophageal (GE) junction into the thorax (Figure 1), and they are often associated with gastroesophageal reflux disease (GERD). There is no risk of gastric volvulus or strangulation with Type I hiatus hernias.
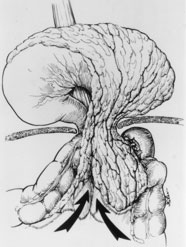
In Type II, or paraesophageal, hiatus hernias (Figure 1), the GE junction remains in its normal anatomic position, but the fundus of the stomach herniates into the thorax. The herniation occurs anterior to the esophagus and within a hernia sac of peritoneum. Paraesophageal hernias typically occur in the elderly, and enlarge with time. As the fundus and body of the stomach migrate into the intrathoracic hernia sac, the stomach “flips” into an “upside down” position (Figure 2), an anatomic condition that is called an organoaxial gastric volvulus.
Type III hiatus hernias have both sliding and paraesophageal components. Type IV hernias are entirely paraesophageal, but in addition to the stomach, they contain other organs such as the spleen or transverse colon.
Clinical Considerations
Most patients with Type II paraesophageal hiatus hernias are asymptomatic, but some experience nonspecific symptoms such as reflux, dysphagia, early satiety, or atypical chest pain. As the hernias enlarge, respiratory symptoms such as shortness of breath can develop, and chronic blood loss from ulcerations of the stomach and or esophagus can cause anemia.
Acute, life threatening complications can develop, and manifest as severe pain in the chest or epigastrium, dysphagia, and often the inability to vomit. Failure to pass a naso-gastric tube heightens the clinical suspicion of obstruction or gastric volvulus with strangulation. The incidence of this life threatening complication is currently debated, but many reports have cited a 35-40% risk of gastric volvulus which mandates emergency surgical intervention. If gastric necrosis and/or perforation have occurred, the mortality of emergency surgery can be as high as 50%. This experience prompted most surgeons to recommend elective surgical intervention in all but the highest risk patients with a paraesophageal hernia.
More recent studies suggest the risks of both strangulation and emergency surgery are in fact much lower. Stylopoulos and coworkers from Massachusetts General Hospital estimated that 18% of patients 65 years of age and older with asymptomatic paraesophageal hiatus hernias develop life threatening complications that necessitate emergency surgery.1 The mortality of emergency surgery in their experience was 5%, though pooled data from large series indicated a 17% mortality rate. In contrast, the mortality of elective surgery was 1%. They recommended watchful waiting in patients with asymptomatic paraesophageal hiatus hernias.
Surgeons have long debated the optimal technique for repair of paraesophageal hiatus hernias. Thoracic surgeons have recommended approaching large hernias through the chest, to allow complete dissection and mobilization of the esophagus. Abdominal surgeons naturally advocated an approach from below, which allowed the addition of anterior gastropexy (fixation of the stomach to the anterior abdominal wall) to minimize the risk of recurrence. Once surgeons became familiar with the techniques of laparoscopic surgery, however, they began to use laparoscopic techniques to repair paraesophageal hernias. This new approach was first used in the early 1990s, and since then laparoscopic repair has gradually replaced open abdominal or thoracic operations as the procedure of choice for repairing paraesophageal hernias.
METHODS
We reviewed the medical records of all 20 patients on whom we performed elective laparoscopic surgery for paraesophageal hiatus hernias at Lancaster General Hospital. Our experience began in January 2003, by which time we had accumulated more than 6 years of experience performing laparoscopic Nissen fundoplication for gastroesophageal reflux due to Type I hiatus hernias. We were asked to evaluate Mr. W.A., a 57 year old male with a large and symptomatic Type II (paraesophageal) hernia. We carried out an elective laparoscopic repair on January 31, 2003.
The basic principles of the laparoscopic approach are well summarized in Seely’s collective review published in 2005.2 Patients are admitted the morning of the planned procedure. General endotracheal anesthesia with full muscular relaxation is used, and the patient is positioned in a low lithotomy position so the surgeon can stand between the patient’s legs. Insertion of the cannulas begins with placement of a 10 mm Hasson cannula in the patient’s midline several centimeters above the umbilicus. This is done with an open technique, which means exposure is through a very short conventional incision that permits direct observation of the process. Once this access route has been safely established, a pnemoperitoneum is induced by insufflating CO2, and 4 additional trocars ( three 5 mm trocars and one 11mm trocar) are placed under laparscopic observation (Figure 3).
The repair then begins with dissection and removal of the hernia’s peritoneal sac from the mediastinum to minimize the risk of recurrence. Repair of the diaphragmatic crura is usually performed with interrupted permanent sutures. Several other adjunctive techniques that are controversial and are not universally performed include the use of mesh for repair of the hiatus, fundoplication to prevent reflux, and gastropexy.
RESULTS
As noted, 20 patients with symptomatic paraesophageal hiatus hernias have undergone surgical evaluation and laparoscopic repair at Lancaster General Hospital since January 2003. There were 13 females and 7 males, who ranged in age from 39 to 82 (average 65). There were no deaths. The average length of stay (LOS) was 6.6 days, but for the 18 patients whose surgery was completed laparoscopically, the average LOS was only 2.8 days (range 1-5).
Two patients suffered intraoperative complications and required conversion to a laparotomy. Both had esophageal perforations that occurred during dissection and removal of the hernia sac. The perforation was recognized during laparoscopic surgery and a laparotomy was performed to repair the esophagus. Gastrostomy and feeding jejunostomy tubes were inserted. A nasoesophageal tube was positioned proximal to the esophageal repair and a Jackson Pratt drain was placed in close proximity to the esophagus. One patient developed a persistent esophageal fistula. His nasoesophageal tube had been inadvertently removed in the early post-op period. The second patient that suffered an esophageal perforation healed promptly as documented on an esophogram on the 8th post operative day.
The most common postoperative symptom is dysphagia, which occurs often but is typically very mild, and has resolved within two months in all patients.
DISCUSSION
Our experience with laparoscopic repair of paraesophageal hernias compares favorably with similar reports in the literature, which emphasize the complexity of both the disease and the surgery to correct it. In our initial experience two patients (10%) suffered an esophageal perforation but there were no deaths. This experience compares favorably with Seeley’s recent review, which found an 11% incidence of esophageal perforation, and a 3% mortality rate.2
The evaluation of patients with paraesophageal hiatus hernias should include both endoscopy and an upper GI barium study. 24-hour pH testing and esophageal manometry are not essential and are typically difficult if not impossible to perform or interpret. Since many patients are elderly and have comorbid conditions, thorough preoperative cardiopulmonary evaluation is often necessary.
All of our patients were symptomatic, and surgery was clearly indicated to relieve symptoms, as well as to prevent the development of potentially serious complications. It is an old adage, however, that no treatment can make an asymptomatic patient feel better, so for those patients we must balance the risk of complications associated with watchful waiting against the morbidity and mortality of elective surgery. It is no wonder that the choice is being debated. As noted earlier, Stylopoulos et al1 recommended watchful waiting in patients with asymptomatic paraesophageal hiatus hernias, but this recommendation has not been universally accepted. First, increasing experience with laparoscopic surgery can be expected to yield lower complication rates. Second, Landreneau and coworkers questioned the outcome analysis in Stylopoulos’ study, which casts doubt on their conclusions. Finally, if emergency surgery becomes necessary, the morbidity and mortality are significantly increased.3
At the very least, if asymptomatic patients are observed they must be made aware of the symptoms associated with gastric volvulus so they will seek prompt evaluation if those symptoms develop. Such patients require close follow up, and UGI studies repeated every one to two years may be useful to monitor the size of the hernia and the development of gastric volvulus. Patients with symptoms, especially if organoaxial gastric volvulus is present on UGI series, should undergo surgery unless comorbid conditions result in prohibitive risk.
CONCLUSIONS
Paraesophageal hiatus hernias are being diagnosed more frequently. Elective laparoscopic surgical reduction and repair has an excellent success rate with low morbidity and mortality. Our experience at Lancaster General Hospital is comparable to published experience from major academic institutions. Laparoscopic repair has allowed shorter hospitalization and recovery with short and long term results comparable to open repair with either an abdominal or thoracic approach. Laparoscopic repair has become the procedure of choice for paraesophageal hernias. As a result of the improvement in laparoscopic techniques and results, there is considerable debate about whether a traditionally aggressive surgical approach should be extended to asymptomatic patients.
REFERENCES
- Stylopoulos N et al. Paraesophageal Hernias: Operation or Observation? Ann Surg 2002; 236: 492-501.
- Seely AJE et al. Principles of Laparoscopic Surgery of the Gastroesophageal Junction. J Am Coll Surg 2005; 200:77-87.
- Landreneau RJ et al. Management of Paraesophageal Hernias. Surg CLNA 2005; 85:411-432.
Edward T. Chory, M.D., F.A.C.S.
Lancaster Surgery Group
2104 Harrisburg Pike – Suite 200
Lancaster, PA 17604
717-544-3626
etchory@pol.net
Figure 1.
|
With sliding or axial hiatal hernia there is thinning and elongation of the phrenoesophageal membrane leading to herniation of the stomach into the posterior mediastinum. As such, there is no potential for incarceration or strangulation. With paraesophageal herniation, visceral elements herniate through a focal weakness in the phrenoesophageal membrane with the potential to lead to the usual array of complications associated with visceral herniation through a constricted aperture. (GI Motility Online, Kahrilas PJ & Pandofino JE, Hiatus Hernia. Medicine Online LLC and Nature Publishing Group. Source: Skinner DB. Hernias (hiatal, traumatic and congenital). In: Berk JE, ed. Gastroenterology, 4th ed. Philadelphia: WB Saunders, 1985:705-716, Copyright Elsevier)
|
Figure 2.
|
Large paraesophageal hernia with stomach and omentum migrating into the intrathoracic hernia sac. (Ann of Thorac Surg, 2001;71-1080-7. Copyright permission granted by Elsevier. Source: Nyhus LM, Baker RJ, fisher JE, eds. Mastery of Surgery. Boston: Little, Brown and Co., Inc. 1996)
|
Figure 3.

|
Approximate location of abdominal trochar access sites used by our group for laparoscopic antireflux surgery. (Ann of Thorac Surg, 2001;71-1080-7. Copyright permission granted by Elsevier. Source: Landreneau RJ, Keenan RJ, Ferson PF. Gastroesophageal reflux disease. In: Cameron JL, ed. Current Surgical therapy, 5th ed. St. Louis: Mosby Year Book, 1995:29)
|
Figure 4.

Preoperative UGI showing large paraesophageal hernia with “upside down" stomach in chest with air-fluid level.