The article by Dr. Chory in this issue describes an innovative and less invasive technique for the repair of paraesophagial hernias. Imaging, of course, plays a pivotal role in the recognition of diseases that bridge the diaphragm, and the capability of CT scans to provide cross-sectional information in a multiplanar format has greatly enhanced our ability to identify congenital and acquired diaphragmatic defects. While barium studies remain vital in assessing diaphragmatic hernias pre- and post-operatively, plain film studies do not directly visualize the diaphragm, while CT, MRI, and ultrasound do.
Congenital Defects
Congenital diaphragmatic hernia (CDH) is a well-described condition that occurs in about 1 in 5000 live births. The condition is usually sporadic, though association with various genetic syndromes has been reported. CDH consists of herniation of bowel, and occasionally solid organs, into the chest, usually thru the Foramen of Bochdalek, a potential weak spot in the posterolateral diaphragm. 80 % of CDH occur on the left side, as the liver provides a relative barrier on the right. A number of cases have now been diagnosed in utero using screening ultrasound, but infants typically present shortly after birth with respiratory distress (Fig 1). The major clinical problem is pulmonary hypoplasia, a result of the lung having failed to develop in utero as the thoracic cavity is filled by abdominal contents. Treatment is surgical, with the prognosis typically dependent on the degree of lung abnormality. Infants who present less than 6 hours after birth experience a 70% mortality, with much better survival if presentation occurs 12-24 hours after delivery.
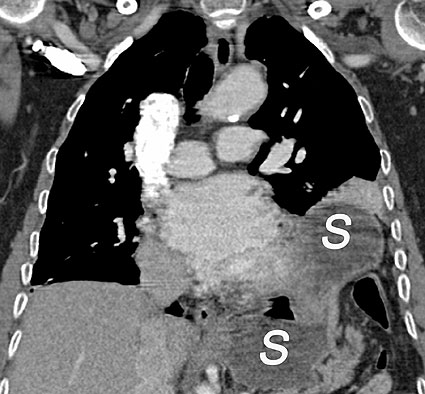
These congenital diaphragmatic defects have also been described in the adult population, and the widespread use CT scanning has led to the recognition that these hernias are not uncommon and are often asymptomatic (Fig 2). In one series, 0.2% of over 13,000 patients undergoing CT examinations for other reasons were found to have hernias through the Foramen of Bochdalek. Most contained only omental fat, but bowel and solid organs were sometimes present. A much less common form of hernia may occur thru the Foramen of Morgagni, another potential defect in the diaphragm in the anteriomedial portion, near the heart. These account for only about 2% of CDH in the newborn period, but may present as paracardiac masses in the adult (Fig 3). Here again, the ability to view the diaphragm directly and to reconstruct the data in the most advantageous plane for viewing greatly aids in diagnosing these conditions.
Hiatal Hernias
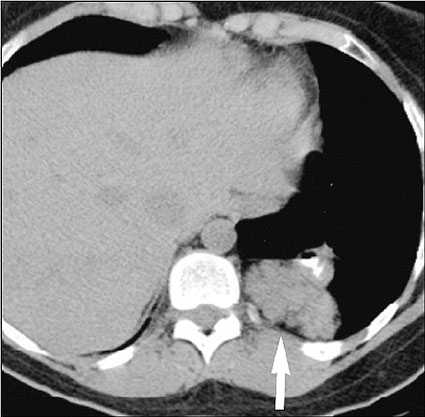
By far the most common form of diaphragmatic hernia is the hiatal hernia, a subject already reviewed in Dr. Chory’s article. As he mentions, the vast majority of these are Type 1, with simple elevation of the esophagogastric junction into the chest. Aside from their association with reflux, they are typically an incidental finding during chest radiography, barium studies, or CT. (Fig 4) The other three types mentioned all include more complicated anatomy and carry the risk of torsion and infarction.
The postoperative evaluation of patients after repair of diaphragmatic hernias is also dependent on imaging. Early postoperative leaks or strictures are most often identified with fluoroscopic studies that use radioopaque contrast, first water-soluble, then barium. Later in the patient’s course, a variety of other problems may occur, including strictures, dehiscenses, and recurrent hernias (Fig 5)
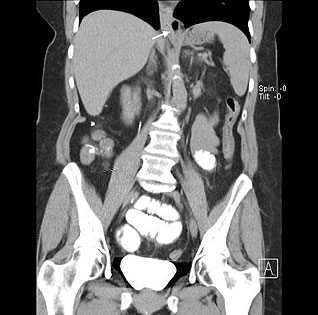
In this era of high speed vehicular trauma, diaphragmatic rupture has become a more frequent cause of defects in the diaphragm. (Fig 6) Before the widespread use of multislice CT and the ability to reconstruct the images in any desired plane, this condition was notoriously difficult to recognize. Now, most injuries to the diaphragm are evident, and the surgeon knows prior to surgery where the defect is and what has gone through it, which leads to improved surgical outcomes.
REFERENCES
- Langham MR Jr, Kays DW, Ledbetter DJ, et al: Congenital diaphragmatic hernia. Epidemiology and outcome. Clin Perinatol 1996 Dec; 23(4): 671-88
- Mullins ME, Stein J, Saini SS, et al: Prevalence of Incidental Bochdalek’s Hernias in a Large Adult Population. AJR 2001 Aug; 177:363-366
- Pineda V, Andreu J, Caceres J, et al: Lessons of the Cardiophrenic Space: Findings at Cross-sectional Imaging Radiographics 2007; 27:19-32
- Abbara S, Kalan MMH, Lewicki AM: Intrathoracic Stomach Revisited. AJR 2003; 181:403-414
- Canon CL, Morgan DE, Einstein DM, et al. Surgical Approach to Gastroesophageal Reflux Disease: What the Radiologist Needs to Know. Radiographics 2005; 25: 1485-1489
- Iochum S, Ludig T, Walter F, et al. Imaging of Diaphragmatic Injury: A Diagnostic Challenge. Radiographics 2002 22: S103-S118
Leigh S. Shuman, M.D.
Staff Radiologist, Lancaster General Hospital
Lancaster Radiology Associates, Ltd.
P.O. Box 3555
Lancaster, PA 17604
717-544-4900
LSShuman@LGHealth.org
Figure 1. Congenital diaphragmatic hernia in a newborn

|
(Reprinted with permission from the American Journal of Roentgenology. Kammen BF et al, AJR 2002;178:185-189
|
Figure 2. A small Foramen of Bochdalek hernia in an adult with bowel and the pancreatic tail in the left hemithorax (arrow)
|
(Reprinted with permission from the American Journal of Roentgenology. Mullins ME et al, AJR 2001;177:363-366)
|
Figure 3. Sagittal CT view of a small Foramen of Moargagni hernia with colon above the diaphragm (arrows)

|
(Lesions of the Cardiophrenic Space: Findings at Cross-sectional Imaging. Pineda et al. Radiographics 2007; 27: 19-32. Copyright by the Radiological Society of North America 2007.)
|
Figure 4. Coronal view of a typical small type I hiatal hernia (arrow)
|
(Surgical Approach to Gastroesophageal Reflux Disease: what the radiologist needs to know. RadioGraphics 2005;25:1485-1499. Copyright by the Radiological Society of North America 2005)
|
Figure 5. Barium study on a patient post Nissen fundoplication with herniation of the wraps (asterisks) back through the diaphragmatic hiatus (arrow)

|
(Imaging of Diaphragmatic Injury: A diagnostic challenge. Radiographics 2002; 22:S103-S116. Copyright by the Radiological Society of North America 2005)
|
Figure 6. Coronal CT view of traumatic diaphragmatic rupture with portions of the stomach (S) above and below the diaphragm.