ABSTRACT
The time interval between the onset of symptoms of acute myocardial infarction (AMI) and the initiation of reperfusion therapy is a major determinant of patient outcome. To minimize this interval, we developed an emergency response system known as ‘Code R’ that organizes all those involved in AMI care. The system has reduced the delay between presentation and treatment of patients who present with AMI.
INTRODUCTION
An acute myocardial infarction (AMI) is a medical emergency requiring immediate intervention. More than 90% of myocardial infarctions are caused by an acute thrombotic obstruction in a coronary artery that prevents the circulation of oxygenated blood to a portion of the heart. Irreversible, ischemia-induced myocardial necrosis begins within as little as 20 minutes of occlusion.1 The longer the duration of the occlusion, the greater the volume of necrotic myocardium and the larger the final infarct size.
Although opening the infarct-related coronary artery as soon as possible after the onset of symptoms is key to preventing morbidity and mortality, there are multiple challenges to minimizing the time to treatment for patients presenting with AMI.
The first challenges arise from patients’ behavior: they often delay seeking medical attention because they fail to recognize the signs and symptoms of an AMI; they misinterpret symptoms (e.g., believe chest pain to be indigestion); they believe symptoms are transitory and endurable; or they transport themselves to the hospital rather than calling an ambulance. Unfortunately, community-wide patient education campaigns generally produce few permanent changes in how patients behave.2
Challenges also arise after the patient arrives at the hospital. For example, delays may be caused by a lack of coordinated hospital protocols. An emergency room (ER) physician may diagnose an AMI, but be delayed by a requirement to consult a cardiologist before administering pharmacologic treatment or activating the personnel needed to perform primary percutaneous coronary intervention (PCI).3 Similarly, some hospitals may require that the attending physician contact a patient’s primary care provider before administering any treatment, again prolonging the duration of ischemia.3 Or, ambulance teams may be instructed to transport patients to the nearest hospital, regardless of whether that hospital has the resources to appropriately treat AMI patients. This creates the need for a subsequent transfer to another hospital and further delays. Likewise, in the absence of pre-existing treatment protocols, valuable time may also be lost while hospital personnel decide which type of reperfusion therapy to administer.
The systems used to coordinate the triage, diagnosis, and treatment of AMI patients are multi-faceted and complex; prompt treatment of an AMI requires coordinated and cooperative care from multiple specialists including cardiologists, interventional cardiologists, emergency physicians, pharmacists, nursing staff, paramedics, and 911 operators. With so many involved in the care of an AMI patient, it is essential to have predetermined and agreed to protocols that delineate the responsibilities of each participant and clearly define treatment pathways. Fortunately, all those involved recognize the seriousness of the problem, and the opportunity to actually save lives. At Lancaster General Hospital (LGH), we developed an emergency response system known as Code R that greatly reduces the delay between patient presentation and treatment.
Reperfusion Therapy
Reperfusion therapy with fibrinolytic agents or primary PCI is indicated in AMI patients presenting within 12 hours of symptom onset and in patients with a new left bundle branch block. Although fibrinolytic therapy continues to be a guideline-approved treatment used worldwide, in clinical trials primary PCI is associated with higher infarct-related artery patency rates, lower mortality rates, and a lower risk of bleeding complications including intracranial hemorrhage.4,5 The cardiology community and current guidelines from the American College of Cardiology/American Heart Association (ACC/AHA) generally consider primary PCI preferable to fibrinolysis, provided it can be performed by skilled operators in centers with readily available surgical backup within less than 90 minutes of the patient’s arrival at the hospital (referred to as door-to-balloon time—the interval between the time a patient arrives and the time PCI is performed) (Table 1).6
Time to Treatment
The guideline’s insistence that primary PCI be performed rapidly is based on a wealth of data demonstrating that prolonged delays to intervention worsen short-, mid-, and long-term outcomes. For example, an analysis of the National Registry of Myocardial Infarction (NRMI) calculated in-hospital mortality rates according to door-to-balloon times among 27,080 consecutive AMI patients who underwent primary PCI.7 The study found that as door-to-balloon time increased, so did in-hospital mortality (Figure 1).
Delays to treatment also adversely affect mid-term outcomes. A retrospective analysis of 1,791 AMI patients who underwent primary PCI evaluated the risk of 1-year mortality based on total ischemic time—the delay between symptom onset and treatment.8 In this study, each 30-minute delay to treatment increased the risk of a patient’s being discharged with severe left ventricular dysfunction (ejection fraction less than 30%), and it increased the risk of mortality at one year by 7.5%. Women and patients considered to have high-risk characteristics—age more than 70 years, diabetes, or previous revascularization—were the most likely to receive delayed treatment.
The adverse effects of prolonged delay to primary PCI can also be seen in long-term outcomes. In 2006, Brodie et al. analyzed 7-year mortality rates according to door-to-balloon time among 2,322 consecutive AMI patients who underwent primary PCI. As in the studies quoted above, as delay increased, the risk of in-hospital and long-term mortality increased (Table 2).9 Prolonged delays appeared to have the most impact on high-risk patients—those who have the most to gain from early intervention.
Hospital Networks
The goal of performing primary PCI within 90 minutes of first medical contact poses both logistical and geographic challenges. The availability of primary PCI is improving, but is still limited, and not all hospitals have cardiologists and catheterization laboratories that meet ACC/AHA criteria. Moreover, even where PCI capable hospitals meet the criteria, it may not be available 24 hours per day 7 days per week.
Complicating the situation is the organization of emergency medical services (EMS), and the availability of in-hospital staff. In many communities, emergency responders are instructed to transport patients to the nearest hospital rather than to one that can perform primary PCI. And, the physical transportation of patients may be complicated by distance, geography, weather, road construction, or traffic. In the hospital, there is the challenge of quickly notifying and mobilizing all the staff needed to perform interventional procedures. Overall, valuable time (which equals heart muscle) may be lost between the time a patient first presents and is diagnosed, until the procedure can be performed in a catheterization laboratory with the necessary personnel mobilized and assembled.
To address these issues, hospital systems throughout the United States, including LGH, are developing regionally specific protocols designed to minimize the delay between first patient contact and intervention. The details of each system vary. Some utilize helicopters, some diagnose patients in the field with portable electrocardiograms (ECG), and some transport patients directly to catheterization laboratories, bypassing emergency departments. Some networks are based on pre-existing trauma networks, whereas others were specifically developed for AMI treatment. Regardless of the resources employed, all utilize specific, predetermined algorithms for identifying and diagnosing AMI, and organizing patient care.
Code R: Reperfusion Therapy at LGH
Code R was developed at LGH by Dr. Seth Worley of The Heart Group in 1988, when fibrinolytic therapy was considered the best available treatment. Dr. Worley reasoned that if the ER physician was given the authority to simultaneously activate a team that included cardiology, pharmacy, radiology, and laboratory services, fibrinolytics could be given sooner. When PCI became the treatment of choice, the system was extended to include the cardiac catheterization laboratory. Similarly, when designers of the emergency network looked for ways to improve door-to-balloon times at LGH, they identified sources of delay in the existing system, considered the size and geography of Lancaster County, and coordinated with local ambulance services to develop a system that rapidly delivers patients and necessary medical personnel to the catheterization laboratory. Over the last 24 months, LGH has extended the Code R process so that it may be triggered by an ECG that is transmitted by paramedics in the field. With the implementation of the pre-hospital ECG leading to earlier activation of the Code R process, the percentage of patients treated within 90 minutes of first medical contact has improved from 70% to 76%, and currently 33% of patients are treated in less than 65 minutes.
Lancaster County consists of almost 1,000 square miles with a population of approximately 500,000 people. The key to the Code R network is its central activation by an ER physician at LGH. The algorithm is shown in Figure 2. Code R follows two pathways depending on where a patient presents. If a patient contacts EMS, an ECG is obtained on the scene by the paramedics, and the tracing is transmitted to the hospital ER for interpretation. If the ER physician suspects an AMI, the ambulance is instructed to transport the patient to LGH where primary PCI is available 24 hours a day. While the patient is in transit, the ER physician, with a single call, pages all the personnel needed to perform primary PCI. In Lancaster, approximately 74% of AMI patients utilize EMS. For the remaining 26% of patients who drive to the ER, an ECG is done immediately upon arrival, regardless of other ER waiting times. If the tracing is positive for an AMI, the ER physician activates the Code R system.
Elsewhere, in some networks where admission through the ER has been associated with delay, EMS-triaged patients may be brought directly to the catheterization laboratory (some hospitals even have a separate entrance to the laboratory).10 However, the examination in the ER provides the cardiologist an opportunity to explain to the patient what is happening, and the treatment plan. It is also where a second ECG is done to confirm the diagnosis. Another reason for passing through the ER is that transport times are usually less than 30 minutes from any point in Lancaster County, in which case it is possible for the patient to arrive at the hospital before the catheterization laboratory can be made ready.
Importantly, the ER physician can begin adjunctive pharmacologic therapy, which may include analgesics, aspirin, clopidogrel, intravenous nitroglycerin, beta-blockers, and/or heparin. Thus, when the patient arrives in the laboratory, the interventional cardiologist can immediately begin the procedure.
Ongoing Initiatives
Nationwide, only about 35% of hospitals achieve an average door-to-balloon time of less than 90 minutes.11 To help improve the quality of care for AMI patients, the ACC recently launched the Guidelines Applied in Practice-Door to Balloon (GAP-D2B) initiative. GAP-D2B is a nationwide quality improvement program designed to help hospitals achieve door-to-balloon times of less than 90 minutes in 75% or more of patients, a goal that LGH has already met. The program provides participating hospitals with strategies for reducing door-to-balloon times by implementing six core measures: authorization of the ER physician to activate the catheterization laboratory; one call to activate the catheterization laboratory; a team that can be ready within 20-30 minutes of the call; prompt data feedback to all participating physicians; a commitment from senior management to reducing door-to-balloon time; and use of a team-based approach. As of March 2007, more than 800 hospitals, including LGH, were enrolled in the initiative.
In addition to such large-scale initiatives, there are several measures that primary care and other physicians can take to help reduce door-to-balloon times. Physicians should educate all patients at risk for an AMI on its signs and symptoms, and instruct patients to contact EMS as soon as symptoms occur. Physicians should also provide information on treatment options, the importance of time, the location of treatment facilities, and advise patients that they can request EMS to transport them to a specific hospital. With this information, even if patients insist on driving themselves to the hospital, they will at least know the most appropriate hospital in their area. And, for patients who do call EMS, they will know which hospital to request.
CONCLUSION
Reducing time to treatment in the management of AMI is key to improving patient outcome. Although patient behavior and patterns of presentation are difficult to change, systems can be established to improve time to treatment. Implementation of an organized network for the systematic care of AMI is possible, and reducing door-to-balloon times to less than 90 minutes for all patients is an obtainable goal. Although efforts to reduce time to treatment have been in place for many years at LGH, all members of our team understand that for an AMI patient, time is muscle, and we continue to look for ways to treat patients as quickly as possible.
REFERENCES
- Reimer KA, Jennings RB, Tatum AH. Pathobiology of acute myocardial ischemia: metabolic, functional and ultrastructural studies. Am J Cardiol. 1983;52:72A-81A.
- Leupker RV, Raczynski JM, Osganian S, et al. Effect of a community intervention of patient delay and emergency medical service use in acute coronary heart disease. JAMA 2000;284:60-67.
- Lambrew CT, Bowlby LJ, Rogers WJ, Chandra NC, Weaver WD. Factors influencing the time to thrombolysis in acute myocardial infarction. Time to thrombolysis substudy of the National Registry of Myocardial Infarction. Arch Intern Med 1997;157:2577-2582.
- Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003;361:13-20.
- Keeley EC, Hillis LD. Primary PCI for myocardial infarction with ST-segment elevation. N Engl J Med 2007;356:47-54.
- Antman EM, Anbe DT, Armstrong PW, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction—Executive Summary. J Am Coll Cardiol 2004;44:671–719.
- Cannon CP, Gibson CM, Lambrew CT, et al. Relationship of symptom-onset-to-balloon time and door-to-balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA 2000;283:2941-2947.
- De Luca G, Suryapranata H, Ottervanger JP, Antman EM. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction. Every minute of delay counts. Circulation 2004;109:1223-1225.
- Brodie BR, Hansen C, Stuckey TD, et al. Door-to- balloon time with primary percutaneous coronary intervention for acute myocardial infarction impacts late cardiac mortality in high-risk patients and patients presenting early after the onset of symptoms. J Am Coll Cardiol 2006;47:289-295.
- Amit G, Carfi C, Gilutz H, Ilia R, Zahger D. Benefit of direct ambulance to coronary care unit admission of acute myocardial infarction patients undergoing primary percutaneous intervention. Int J Cardiol 2006; [Epub ahead of print].
- Nissen NE, Brush JE. GAP-D2B: An alliance for quality. J Am Coll Cardiol 2006;49:1911-1912.
Paul N. Casale, M.D., F.A.C.C.
The Heart Group
217 Harrisburg Avenue
Lancaster, PA 17603
717-397-5484
pncasale@LGHealth.org
Table 1. ACC/AHA recommendations for performing primary PCI
|
Primary PCI is the preferred strategy if the following conditions are met:
- Skilled PCI laboratory with surgical backup available
- Medical contact-to-balloon or door-to-balloon time is <90 minutes
- Operators perform >75 procedures per year
- Hospital performs >200 procedures per year, at least 36 for AMI
Preferable in high-risk patients
- Cardiogenic shock
- Killip class ≥3
Contraindications to fibrinolysis
Late presentation (>3 hours after symptom onset)
Uncertain diagnosis
|
Fibrinolysis preferable
- Early presentation (3 hours or less from symptom onset) and delay to PCI
- PCI is not an option
- Prolonged delay to PCI (>90 minutes from first medical contact)
- Experienced center or operators are not available
|
|
Adapted from: Antman EM, Anbe DT, Armstrong PW, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction—Executive Summary. J Am Coll Cardiol 2004;44:671–719.
|
Table 2. Risk of in-hospital and long-term mortality according to door-to-balloon time
| |
Door-to-Balloon Time (hours)
|
|
| |
0-1.4
|
1.5-1.9
|
2.0-2.9
|
≥3.0
|
P value
|
|
In-hospital mortality
|
4.9
|
6.1
|
8.0
|
12.2
|
<0.0001
|
|
7-year mortality
|
12.6
|
16.4
|
20.4
|
27.1
|
<0.0001
|
|
Adapted from Brodie BR, Hansen C, Stuckey TD, et al. Door-to- balloon time with primary percutaneous coronary intervention for acute myocardial infarction impacts late cardiac mortality in high-risk patients and patients presenting early after the onset of symptoms. J Am Coll Cardiol 2006;47:289-295.
|
Figure 1. In-hospital mortality according to door-to-balloon time among 27,080 consecutive AMI patients.
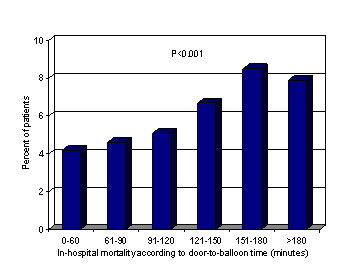
Cannon CP, Gibson CM, Lambrew CT, et al. Relationship of symptom-onset-to-balloon time and door-to-balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA 2000;283:2941-2947.
Figure 2. LGH algorithm for the management of AMI.
Click here for PDF file