Spring 2024 - Vol. 19, No. 1
SCIENTIFIC REPORT
Katlyn Wood, PharmD, BCPS
Clinical Pharmacy Specialist, Pain Management
Penn Medicine Lancaster General Health
Editor’s note: This is a synopsis of a study conducted at Penn Medicine Lancaster General Health and recently published elsewhere.1 JLGH
invites primary study authors to publish brief reports of their work for the purposes of further disseminating potentially practice-changing findings such as those discussed here. For more information, contact us.
The unique pharmacokinetic profile of buprenorphine makes it the perfect therapy for a patient with opioid use disorder (OUD) to prevent cravings as well as diminish the full effects of opioids. But what happens when that same patient is in a motor vehicle accident and requires analgesia?
Surgeons, anesthesiologists, family medicine providers, and addiction specialists in the past may have recommended that the patient hold buprenorphine
2 — presumably based on concerns regarding its pharmacokinetic profile and not based on recognized clinical outcomes. Pharmacokinetic data show a dose-dependent relationship between buprenorphine and
mu-opioid receptor occupancy, in which up to 95% of
mu-opioid receptors can be occupied by buprenorphine at a dose of 16 mg/day.
3,4
The most recent Substance Abuse and Mental Health Services Administration Treatment Improvement Protocol (SAMHSA TIP 63)
5 provides options for buprenorphine management in the perioperative setting. Providers are encouraged to consider split-dosing, which takes advantage of peak concentrations and may be optimized by having patients take the total daily dose of buprenorphine divided into three-times-a-day or even four-times-a-day dosing. Alternatively, patients may need to utilize higher adjunct doses of full opioid agonists for pain and/or opt to hold or reduce buprenorphine doses. Yet, SAMHSA guidance urges further study.
While some previous reports suggested poorly controlled postoperative pain when patients continue on buprenorphine management, more recent literature and guidance supports continuation of buprenorphine without poor analgesic outcomes.
4,6-9 This continuation strategy is based on data that has shown, despite the high
mu-opioid receptor affinity of buprenorphine, that some
mu-receptors remain available for full
mu-opioid agonist activity.
4,6,10
An equally important consideration, when devising a perioperative pain plan, is that after a period of temporary buprenorphine hold, reinitiation can become a complicated process. This is due to several concerns. While there may be a potential need to provide high-risk patients with a short course of opioid therapy to be used after discharge, patients also may run the risk of illicit substance use while buprenorphine is being held. Finally, providers may be concerned about the risk of precipitated withdrawal when buprenorphine is resumed.
3-8,11
With overdose deaths soaring and medication for OUD (MOUD) treatment becoming more commonly prescribed, there is an urgency to provide these patients with the highest quality care in the perioperative setting. For this reason, we aimed to determine, in adult patients requiring acute pain management and maintained on buprenorphine prior to admission, whether:
- There were differences in MME (morphine milligram equivalents) or pain scores for patients whose buprenorphine was held versus continued.
- There were differences in MME or pain scores for patients on >12 mg/day versus ≤12 mg/day of buprenorphine.
A retrospective chart review was conducted on the cases of 78 patients who were hospitalized at Penn Medicine Lancaster General Hospital from 2017 to 2021. The findings of our study aligned with the recent literature supporting continuation of buprenorphine therapy perioperatively, as patients had significantly increased MME requirements when buprenorphine was held.
We were also delighted to find that continuation of buprenorphine at a daily dose of >12 mg/day compared to ≤12 mg/day did not confer a significant difference in the daily average total of MME requirements, nor daily average pain scores (see Fig. 1).
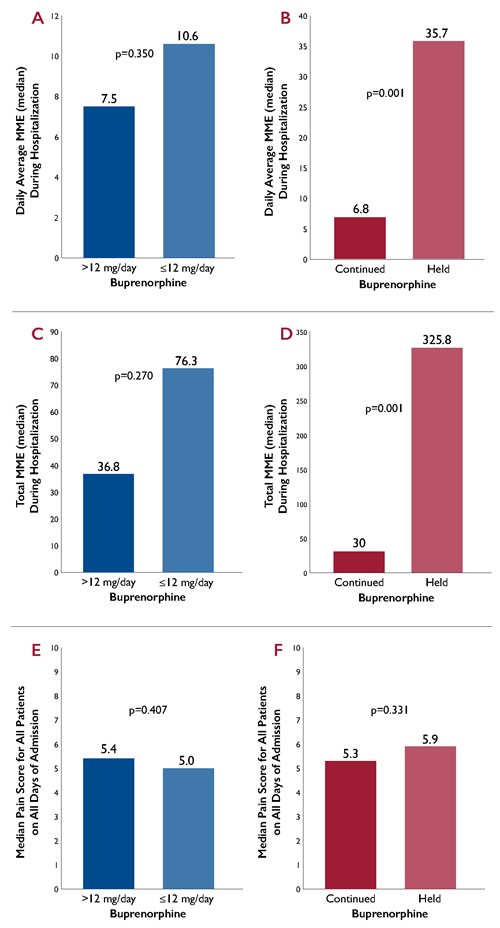 Fig. 1. Comparison of outcomes when buprenorphine continued at a daily dose of >12 mg/day compared to ≤12 mg/day and when continued versus held.
Fig. 1. Comparison of outcomes when buprenorphine continued at a daily dose of >12 mg/day compared to ≤12 mg/day and when continued versus held.
A secondary, but notable, finding identified significantly reduced opioid prescription rates at discharge for those patients whose buprenorphine was continued versus held during the admission (11.3% vs. 31.3%).
Overall, continuation of buprenorphine therapy throughout hospitalization provides a simplified management strategy for OUD patients in acute pain, requires significantly fewer MME to achieve similar pain scores, reduces opioid prescription rates at discharge, and allows us to avoid problems associated with buprenorphine reinitiation.
The takeaway was simple: fear not buprenorphine.
Clinicians should feel comfortable knowing they may continue patients on their prescribed doses of buprenorphine perioperatively or during episodes of acute pain, and expect that by encouraging their patients with MOUD to continue buprenorphine treatment, they can expect better outcomes than if they were to encourage holding/stopping this vital treatment for OUD.
1
REFERENCES
1. Haines AJ, Wood KC, Costello JL, Tawil T. Acute pain management for patients maintained on sublingual buprenorphine as medication for opioid use disorder.
J Addict Med. 2023;17(6):662-669.
2. Clinical Guidelines for the Use of Buprenorphine in the Treatment of Opioid Addiction. Center for Substance Abuse Treatment. Substance Abuse and Mental Health Services Administration (US); 2004.
3. Quaye A, Zhang Y. Perioperative management of buprenorphine: solving the conundrum.
Pain Med.2019;20(7):1395-1408.
4. Lembke A, Ottestad E, Schmiesing C. Patients maintained on buprenorphine for opioid use disorder should continue buprenorphine through the perioperative period.
Pain Med. 2019;20(3):425-428.
5. Medications for Opioid Use Disorder for Healthcare and Addiction Professionals, Policymakers, Patients, and Families. Substance Abuse and Mental Health Services Administration (US); 2021.
6. Ward EN, Quaye AN, Wilens TE. Opioid use disorders: perioperative management of a special population.
Anesth Analg. 2018;127(2):539.547.
7. Kohan L, Potru S, Barreveld A, et al. Buprenorphine management in the perioperative period: educational review and recommendations from a multisociety expert panel.
Reg Anesth Pain Med. 2021;46:840-859.
8. Quaye A, Potter K, Roth S, et al. Perioperative continuation of buprenorphine at low-moderate doses was associated with lower postoperative pain scores and decreased outpatient opioid dispensing compared with buprenorphine discontinuation.
Pain Med. 2020;21(9):1955-1960.
9. Culshaw J, Philpott C, Bradshaw P, et al. Acute pain management in traumatically injured patients with outpatient buprenorphine therapy.
J Surg Res. 2023;289:27-34.
10. Gudin J, Fudin J. A narrative pharmacological review of buprenorphine: a unique opioid for the treatment of chronic pain.
Pain Ther. 2020;9(1):41-54.
11. Warner N, Warner M, Cunningham J, et al. A practical approach for the management of the mixed opioid agonist-antagonist buprenorphine during acute pain and surgery.
Mayo Clinic Proc. 2020;95(6):1253-1267.