Summer 2023 - Vol. 18, No. 2
SCIENTIFIC REPORT
Tenosynovitis and Lymphangitis in the
Setting of Mpox Infection


Cantu Golden
Alexander T. Cantu, MD
Lisa A. Golden, MD
Family Physicians, Family Medicine Residency Program
Penn Medicine Lancaster General Health
INTRODUCTION
Mpox, previously called monkeypox, is a viral disease in the same genus as smallpox. The disease was first noted in monkeys in a Danish laboratory in the 1950s. Mpox was considered rare and was confined to central and western Africa prior to the 2022 global public health emergency. In general, mortality is low; however, individuals who are very young or immunocompromised are more likely to die or have severe illness.1
The classic presentation includes flu-like symptoms followed by a characteristic rash. The rash usually begins as macules and progresses to umbilicated papules, vesicles, pustules, and finally scabs. It can be on the extremities, genitals, chest, and/or face.
The 2022 Mpox global public health emergency was unique in that flu-like symptoms were not always present, but when present, could occur before, after, or concomitantly with onset of the rash. Mpox is spread through direct contact, with the most recent outbreak being transmitted primarily through sexual contact.1 Vertical transmission from mother to fetus is also possible. The incubation period for the disease is 3-17 days.1,2 The individual is contagious until the rash has healed.
Individuals with a rash consistent with Mpox or who have known or suspected exposure should be tested. Mpox cases were first noted in Europe in May 2022 and quickly spread to the United States, including Lancaster, with incidence of infections reaching a peak in August 2022.3
CASE
At the height of the Mpox epidemic in the summer of 2022, a 51-year-old male presents via email to his primary care provider with a lesion on his left distal index finger which he reports has been present for three days. He is concerned about Mpox infection, as he has sex with men and, although he is married, he does have a new sexual partner as of two weeks ago. His recent sexual partner reports being negative for Mpox; however, it is unknown if the partner was tested.
The patient had been healthy until this presentation; his only medications are emtricitabine/tenofovir disoproxil fumarate (Truvada®) for HIV prophylaxis and hydroxyzine as needed for insomnia. He has no flu-like symptoms nor symptoms suggesting lymphadenopathy. He sends a day 3 photo via the online health portal, which was reviewed by his provider. (See Fig. 1 for photos showing progression of an Mpox finger lesion.) He receives reassurance from his provider, who recommends follow-up as needed.
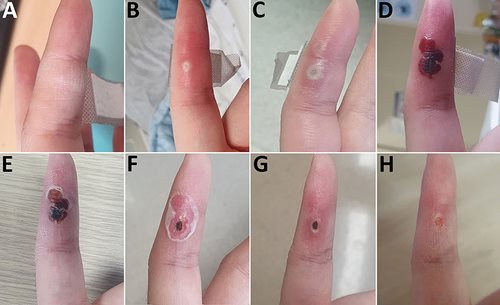
Fig. 1. Photos showing progression of Mpox finger lesion, similar to that on patient’s left distal index finger: A) day 1; B) day 6; C) day 8; D) day 18; E) day 22; F) day 25; G) day 34; H) day 40. Photos from https://wwwnc.cdc.gov/eid/article/29/5/23-0028-f1.
On day 5, he sends another photo to his PCP and is instructed to go to an urgent care center for Mpox testing. When he presents to urgent care on day 6, the lesion appears pustular and is unroofed for Mpox testing. The patient is also started on an outpatient course of trimethoprim-sulfamethoxazole. Polymerase chain reaction (PCR) testing on day 6 confirms Mpox within four days.
On day 8, he reports he has been abstaining from sex and has stopped taking his Truvada®; it is unclear if the patient did this on his own or by recommendation from a physician.
By day 9, the patient has developed mild pain at the site of the lesion, and on day 10, the patient presents to his PCP office with a second lesion on his left wrist, although he has no other systemic symptoms. His PCP performs an incision-and-drainage, which yields only minimal serous drainage and no improvement in pain. On day 13, the patient’s pain worsens and is unrelieved by ibuprofen. It is reported that the patient’s husband has tested negative for Mpox.
The patient is reevaluated in the office on day 14, after again submitting photos via the online health portal. The exam is concerning for necrosis at the site of the initial lesion, superimposed cellulitis, and tenosynovitis with lymphangitis extending up the entire left upper extremity (see Fig. 2). An X-ray reveals no evidence of osteomyelitis. His PCP recommends referral to the emergency department for evaluation and pain control.

Fig. 2. Day 14 photos showing cellulitis and tenosynovitis.
The patient is subsequently hospitalized and treated with IV piperacillin-tazobactam (Zosyn®) and vancomycin. Infectious Disease and Orthopedics are consulted. Blood cultures are negative, bloodwork shows negative inflammatory markers, and a complete blood count is notable because it shows no leukocytosis.
Oral tecovirimat is started on day 15, and a C-reactive protein test is slightly elevated for the first time during his hospitalization. Orthopedics service recommends observation. Vancomycin is stopped, as the patient had a negative MRSA swab. The patient begins to experience pain relief by day 17.
On day 18, IV Zosyn® is stopped, and the patient is discharged on oral Vantin® and TPOXX® to complete a 14-day course per Infectious Disease recommendations. The patient’s complete blood count and comprehensive metabolic panel are within normal limits at discharge. Inflammatory labs are not repeated as the patient is improving overall.
At his transition-of-care appointment on day 23, the patient’s left finger pain is much improved. The necrotic lesion on his left finger and left wrist are healing. He is noted to have three additional lesions on his right lower extremity that are crusted and asymptomatic. Follow-up three months later at his PCP reveals that the patient has recovered completely.
DISCUSSION
The differential diagnosis for this case included an alternative viral infection such as hand, foot, and mouth disease, as well as molluscum contagiosum. These seem less likely due to characteristic physical exam findings of a bacterial infection and positive Mpox testing of the lesion.
Other sexually transmitted infections (STIs) could have been implicated, and although STI testing was not performed, testing could have ruled out primary syphilis and other STIs. Studies suggest a high rate of concurrent STIs among individuals diagnosed with Mpox, so testing might have been appropriate even after Mpox was confirmed.2 An autoimmune etiology was unlikely, as this patient did not have a personal history of autoimmune disorders.
The unique aspect of this case is the development of tenosynovitis, lymphangitis, and necrosis associated with the Mpox lesion. Ultimately, these complications were due to a secondary bacterial infection; this conclusion is supported by clinical improvement with antibiotic therapy.
Necrosis and lymphangitis characteristic of bacterial infection was a rare occurrence in the 2022 pandemic of Mpox. In an international case series, soft tissue infections only occurred in 18 individuals out of 528 patients with Mpox. The case series did include individuals with HIV (who were mostly gay and bisexual men), but the study did not indicate if the 18 individuals with soft tissue infections had HIV nor whether their HIV was appropriately treated.2 The patient in this case did not have HIV and was appropriately on Truvada® for preexposure prophylaxis. He was taking it as prescribed prior to his Mpox infection; therefore, it is highly unlikely he was immunocompromised by an active HIV infection.
It is also notable that the patient did not develop a rash in the typical anogenital or oral regions, which is the usual site of inoculation for Mpox. While his sexual practices and exposure were not discussed in detail, the specifics of this case support the conclusion that any contact site on the skin can lead to development of the characteristic Mpox rash. This patient also developed a secondary bacterial infection that undoubtedly contributed to his pain. The fact that his rash-related pain was unrelieved with over-the-counter medication is one reason why hospitalization was necessary for this patient, and in fact, pain is often a reason for inpatient care of patients with Mpox.2
Among the 30,286 cases as of March 2023, there were 38 deaths in the United States due to Mpox.1 Additional history is not available for these cases, so it is unknown to what extent other concomitant conditions contributed to these deaths. The low case fatality rate is likely due to the less virulent strain of Mpox that affected most patients in the United States.4 Severe illness and death are more likely to occur in immunocompromised individuals. Our patient met criteria for severe illness as he required hospital admission for IV pain medications and antibiotics. However, it should be noted that he was relatively healthy with no other chronic conditions.
This case highlights that although it is unusual, health care providers should be aware of the potential to develop secondary bacterial infections with Mpox lesions. It should also be noted that patients who are on antiretroviral therapy for HIV do not appear to have increased complications or hospitalizations when contracting Mpox during this outbreak.4
As stated previously, it is common for patients to have a concomitant STI, including a new diagnosis of HIV, at the time of Mpox diagnosis, so STI and HIV screening is indicated for all individuals with suspected Mpox. This patient provided almost daily pictures of his finger lesion which allowed his primary care providers to consistently monitor his progression. Health care providers can utilize available technology to remotely monitor patients with potentially transmissible pathogens.
REFERENCES
1. Mpox. Centers for Disease Control and Prevention. March 29, 2023. Accessed April 10, 2023. https://www.cdc.gov/poxvirus/monkeypox/index.html
2. Thornhill JP, Barkati S, Walmsley S, et al. Monkeypox virus infection in humans across 16 countries — April-June 2022. N Engl J Med. 2022;387(8):679-691.
3. Foley AVA, Brady E, Carr Reese P. A clinical primer on the 2022 monkeypox outbreak in the United States. JLGH. 2022;17(3):68-74. http://jlgh.org/Past-Issues/Volume-17-Issue-3/Foley_Monkeypox.aspx
4. Moore MJ, Rathish B, Zahra F. Mpox (monkeypox). In: StatPearls [Internet]. StatPearls Publishing; 2022. Accessed April 6, 2023. https://www.ncbi.nlm.nih.gov/books/NBK574519/