Summer 2023 - Vol. 18, No. 2
SCIENTIFIC REPORT
Pediatric Medical Traumatic Stress and
Trauma-Informed Care
Harry P. Bramley, DO, FAAP
Medical Director, CHOP Hospitalist Program
Lancaster General Hospital
Editor’s note: This article overviews the concept of trauma-informed care; details of treatment are beyond its scope. Case reports are offered at the end to help readers reflect on some of their patients, recognize how medical and other trauma can be negatively impactful, and remind them to be thoughtful during medical traumatic events.
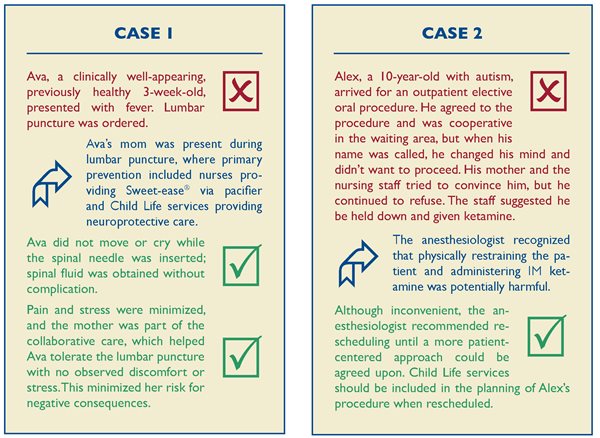
Pediatric medical traumatic stress (PMTS), defined as responses to medical events that include post-traumatic stress symptoms, can occur after any medical intervention.1 Children and adolescents who have poorly managed pain, who undergo repeated procedures, or who experience frightening or invasive treatments are at greater risk.2 Many children do well after medical interventions, such as blood draws, suturing, abscess drainage, wound care, or surgery, but others may struggle.
ADVERSE CHILDHOOD EXPERIENCES
Experiences in childhood have a significant effect on subsequent physical health, mental health, and developmental trajectories.3 Traumatic experiences in childhood can negatively alter developing neurological systems, affecting executive function, creating mental health challenges, and placing children at risk for developing learning disabilities.4-7 The long-term effects of adverse childhood events (ACEs) may be altering the health of more than two-thirds of adults in the United States.8 Reducing exposure to childhood trauma and mitigating post-trauma effects would significantly reduce adult morbidity and mortality.9
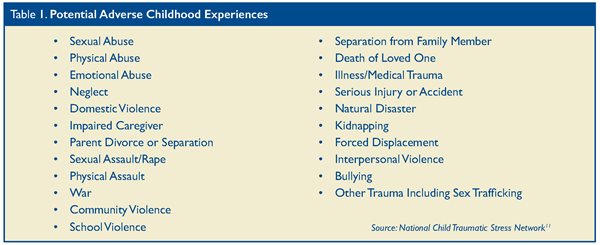
About 34 million children younger than 18 years of age — or almost half of American children — have experienced at least one potentially traumatic early childhood experience.10 Adverse childhood experiences were first defined in 1998, and the list of potential adversities was expanded to 22 by the National Child Traumatic Stress Network (see Table 1).11
Adverse childhood experiences can affect health outcomes, both in the short and long term.12 ACEs can permanently damage the brain and negatively impact the developing neurological and cognitive systems.7 Adversity is common, and symptoms of trauma overlap with the symptoms of other pediatric conditions, therefore the health care provider should consider trauma in the differential diagnosis for patients with developmental, mental health, behavioral, and physical symptoms.3
Children with a history of ACEs are at greater risk to develop medical traumatic stress and may also experience re-traumatization after medical events.13 A history of psychological trauma and ACEs can cause amplification of pain and delayed medical recovery.14-16 Strategies to mitigate the damaging effects of early childhood trauma may promote resilience.17
PEDIATRIC MEDICAL TRAUMATIC STRESS
Pediatric medical traumatic stress is common among injured/ill children and is often associated with elevated distress, noncompliance, and poor health outcomes.18 PMTS occurs when aspects of the child’s medical care are traumatic and defined as responses to medical events that include post-traumatic stress symptoms.1,3 For example, researchers found that circumcision has long-lasting traumatic effects; boys who had been circumcised were more sensitive to pain than uncircumcised boys, and circumcised boys had a greater vaccination response, which may represent a post-traumatic stress disorder triggered by the painful event of vaccination.19 For many children, injury or medical interventions such as procedures or invasive treatments may be potentially traumatizing and/or re-traumatizing.
Providers who care for children must be aware of different types of medical traumatic stress. First, although screening for ACEs is an important part of the medical evaluation, screening itself may be traumatizing or re-traumatizing and lead to further pathology or limited follow-up.20 Further examples may include using restraints on a person who has been sexually abused or placing a child who has been abandoned in a seclusion room.
Factors that may increase the risk for PMTS include undermanaged or undertreated pain, repeated procedures, receiving a serious diagnosis, or experiencing invasive treatments.2 Children with ACEs or a history of trauma may be especially at risk for developing PMTS or re-traumatization after medical procedures.13
The effects of traumatic medical procedures and treatments can be mitigated by being thoughtful to the child’s and family’s experience of medical care and being mindful of ways to reduce the painful aspects of the procedure or treatment.3 Health care providers should ask about fears and worries for both the patient and caregivers, as well as maximize pain management and provide comfort measures by using both non-pharmacological strategies and medications when appropriate. It is also important that family and caregivers are heavily involved in the child’s care, and the entire health care team should work together to ensure their ability to provide effective support.2,3
NEUROPROTECTIVE CARE
Stress can lead to maladaptive brain alterations, which can negatively affect outcomes associated with medical treatment and well-being. Thus, it is important that health care providers and health care systems caring for infants and children understand neuroprotective care. The stress of medical interventions can also lead to maladaptive brain alterations and may negatively impact the potential to maximize health outcomes and well-being.21
Neonatal intensive care units (NICUs) nationally and internationally have developed frameworks of neuroprotective care.2 These strategies are intended to protect infants’ brains and their future development from the potentially traumatic effects of the NICU.22 These strategies of neuroprotective care have recently been introduced into older age groups, such as pediatric cardiac ICUs.23
The five core practices of neuroprotective care include: minimizing pain and stress, promoting activities of daily living, establishing a healing environment, protecting sleep, and supporting family collaborative care.22 Clustering nighttime care when possible, teaching patients to manage pain with non-pharmacologic coping strategies, monitoring the sound in patients’ rooms, and encouraging families to be present during procedures and bedside rounds are a few examples of neuroprotective care.
Post-traumatic symptoms can be correlated with the level of pain a child endures and the level of stress the family feels during the hospitalization.24 Individual components of neuroprotective care can reduce the risk of PMTS and improve consequences of medical intervention.2 Simple non-pharmacological pain and stress management may be able to prevent the negative consequences of child pain and family stress.25
TRAUMA-INFORMED CARE
Trauma-informed care (TIC) is defined by the National Child Traumatic Stress Network as medical care in which all health care teams assess, recognize, and respond to the effects of traumatic stress on children, caregivers, and even health care providers. Practicing trauma-informed care means being aware of trauma-related symptoms, promoting an emotionally safe environment of care, and offering interventions to mitigate the effects of trauma exposure.17
In the health care setting, TIC focuses on the prevention, identification, and assessment of trauma; response to trauma; and recovery from trauma.3 It can be categorized into three main areas:
-
Primary prevention of trauma and promotion of resilience.
-
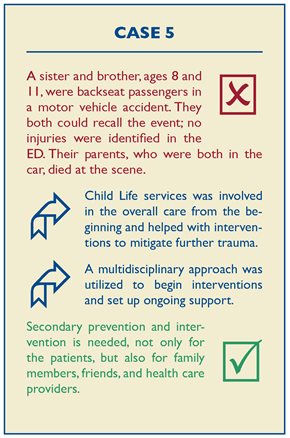
Secondary prevention and intervention for those exposed to potentially traumatic experiences. This includes caregivers, siblings, and health care workers.
-
Tertiary care for children who display symptoms related to traumatic experiences.3
The August 2021 clinical report on TIC by the American Academy of Pediatrics suggests health care providers and organizations caring for children organize TIC into five strategies: awareness, readiness, detection and assessment, management, and integration.3
Awareness
Children living in an environment with a secure relationship that is safe, stable, and nurturing will develop skills that prevent or ameliorate the effects of cumulative traumas.26 Toxic stress may occur when children experience adverse events in the relative absence of protective relationships, which can result in long-lasting or lifelong impairments.21 Reports suggest up to 80% of children and their family members develop trauma-related symptoms after a life-threatening illness, injury, or painful procedure.27
Further, it is important for health care workers to recognize certain populations may be at greater risk of experiencing trauma and may lack an environment with secure relationships. Children who have suffered child maltreatment, immigrant and refugee children, children living in poverty, and children of underrepresented racial, ethnic, and religious groups are examples of these populations.3 In addition, children at greater risk for PMTS include preterm infants, children with chronic medical conditions, and those with serious injury or illness.28
Readiness
Readiness requires health care workers have a compassionate approach that does not suggest blame, while at the same time understanding the context of a child’s community and the strengths and weaknesses of the caregivers. Building on family protective factors and emphasizing strengths rather than deficits is a fundamental part of TIC.3
Services that focus on supporting self-regulation and self-efficacy, as well as on a caregiver’s strengths when providing guidance, help ready the patient for what may be a potential traumatic experience. (See Case 4 below for an example.)
Detection and Assessment
Caring for patients at risk for experiencing trauma can necessitate having protocols and practices in place to help identify and address safety concerns. Detection involves both surveillance and formal screening, and can include purposeful triage, history-taking, examination, and differential diagnoses. Mitigating the stress of a painful procedure can include understanding certain fears, optimizing pain management and comfort measures, and encouraging caregivers to provide effective support.3 Recognizing that a patient may be having trouble moving forward with a procedure, then pausing and assessing fears, might help optimize a potentially traumatic experience and minimize long-lasting negative effects.
Management
Psychoeducation is the first step in management and may include a basic explanation of how trauma can affect a child’s behavior. This simple step may help move a caregiver from frustration to empathy.3
Anticipatory guidance given by health care providers can help families begin to address the effects of trauma as soon as possible.3 For example, a pediatric patient and their family admitted to the hospital following injuries sustained after a trauma may benefit from some education regarding the signs and symptoms of post-traumatic stress disorder and how to seek help if needed.
It is important that children and their families feel emotionally safe and respected.3 An example would be to approach children in a slow and calm manner, allowing them to sit with the caregiver while using a higher pitched voice, which might ease a child’s tension. Individuals with a history of trauma are more sensitive to tone of voice, and low tones may imply danger and stimulate defensive responses.29,30
Integration
Integrating knowledge about trauma into policies, procedures, and daily practice is the next step in creating a trauma-informed medical milieu.31 Educating all team members, developing community partnerships, and addressing the trauma experiences of staff are examples of TIC integration.
One example of integrating TIC is implementing a chaperone policy to provide guidance and awareness to help patients and families feel safe. Additionally, guidelines about a maximum number of IV attempts and necessitating the documentation of difficult IV insertions may underscore the need for appropriate training and re-training. Further, Child Life services, when made a regular part of the health system team, can help bridge gaps in care.
Child Life Services
A Certified Child Life Specialist is credentialed by the Association of Child Life Professionals. These individuals earn bachelor’s degrees and receive special training in the developmental impact of pediatric injury and illness. The American Academy of Pediatrics has determined that Child Life services are essential to overall health care services for children and families, thus funding for their services should be included in the hospital operating budget.32
The January 2021 American Academy of Pediatrics policy statement on Child Life Services further indicates that Child Life programs are an important component of pediatric hospital-based care. Certified Child Life Specialists collaborate with the entire health care team to promote coping skills and minimize the adverse effects of hospitalization and other potentially stressful situations. Child Life services are associated with improved quality and decreased cost, as well as overall patient and family experience.32
SUMMARY
Pediatric medical trauma is one of many potential adverse childhood events. Medical interventions can be traumatic for children, but health care teams can work to mitigate the potential for PMTS.
It is vital that health care providers understand the frequency with which ACEs occur in the pediatric population and the value of inquiring about past events. A history of ACEs may increase the risk of PMTS and can cause chronic, and at times, disabling symptoms. Understanding the history of a patient’s ACEs may help to reduce the risk of unnecessary tests when evaluating ongoing symptoms and help to institute appropriate treatment without delay. Knowing a patient’s history of ACEs may also aid the health care team as it works to mitigate the risk of PMTS and re-traumatizing.
Being aware of the risks for and implications of trauma will help augment risks. Simple neuroprotective strategies, such as encouraging parents and caregivers to be present and a part of medical procedures, can help minimize risk and maximize health outcomes.
Certified Child Life Specialists are experts in TIC and play a vital role in the care of children. Their expertise and knowledge of neuroprotective care strategies can significantly improve the overall outcome for children and families, and can reduce the risk of PMTS. By creating a TIC culture, we can improve the health, safety, and satisfaction of our patients and their families.


REFERENCES
1. Kazak AE, Kassam-Adams N, Schneider S, Zelikovsky N, Alderfer MA, Rourk M. An integrated model of pediatric medical traumatic stress. J Pediatr Psychol. 2006;31(4):343-355.
2. Agoston AM, Basu RK, Nelson S. A universal, trauma-informed approach to pediatric hospital medicine. Hosp Pediatrics. 2020;10(11): 1017-1019.
3. Forkey H, Szilagyi M, Kelly E, Duffee J. Trauma-informed care. Pediatrics. 2021;148(22):e2021052580.
4. Stirling J, Amaya-Jackson L. Understanding the behavioral and emotional consequences of child abuse. Pediatrics. 2012:129(1):e232-e246.
5. Crozier J, Voorhees E, Hooper S, de Bellis M. Effects of abuse and neglect on brain development. Child Abuse and Neglect. Saunders; 2011:516-525.
6. Arsten AF. Stress signaling pathways that impair prefrontal cortex structure and function. Nat Rev Neurosci. 2009;10(6):410-422.
7. Howell BR, Sanchez MM. Understanding behavioral effects of early life stress using the reactive scope and allostatic load models. Dev Psychopathol. 2011:23(4):1001-1016.
8. Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many leading causes of death in adults. The Adverse Childhood Experience (ACE) Study. Am J Prev Med. 1998;14(4):245-258.
9. Merrick MT, Ford DC, Ports KA, et al. Vital signs: estimated proportion of adult health problems attributable to adverse childhood experiences and implications for prevention — 25 states, 2015-2017. MMWR Morb Mortal Wkly Rep. 2019;68(44):999-1005.
10. Bethel C, Davis MB, Gombojav N, Stumbo S, Powers K. A National and Across State Profile on Adverse Childhood Experiences Among Children and Possibilities to Heal and Thrive: Issue Brief October 2017. Johns Hopkins Bloomberg School of Public Health; 2017.
11. Amaya-Jackson L, Absher LE, Gerrity ET, Layne CM, Halladay Goldman J. Beyond the ACE Score: Perspectives from the NCTSN on Child Trauma and Adversity Screening and Impact. National Center for Child Traumatic Stress; 2021. Accessed December 19, 2022. https://www.nctsn.org/resources/beyond-the-ace-score-perspectives-from-the-nctsn-on-child-trauma-and-adversity-screening-and-impact
12. Steen M, Raynor J, Baldwin CD, Jee SH. Child adversity and trauma-informed care teaching interventions: a systemic review. Pediatrics. 2021;149(3):32-47.
13. Nurius PS, Green S, Logan-Greene P, Borja S. Life course pathways of adverse childhood experiences toward adult psychological well-being: a stress process analysis. Child Abuse Negl. 2015;45:143-153.
14. Holley AL, Wilson AC, Noel M, Palermo TM. Post-traumatic stress symptoms in children and adolescents with chronic pain: a topical review of the literature and a proposed framework for future research. Eur J Pain. 2016;20(9):1371-1383.
15. Nelson SM, Cunningham NR, Kashikar-Zuck S. A conceptual framework for understanding the role of adverse childhood experiences in pediatric chronic pain. Clin J Pain. 2017;33(3):264-270.
16. Zatzick DF, Jurkovich GJ, Fan MY, et al. Association between post-traumatic stress and depressive symptoms and functional outcomes in adolescents followed up longitudinally after injury hospitalization. Arch Pediatr Adolesc Med. 2008;162(7):642-648.
17. Duffee J, Szilagyi M, Forkey H, Kelly E. Trauma informed care in child health systems. Pediatrics. 2021;148(2):e2021052579.
18. Christian-Brandt A, Santacrose H, Farnsworth H, MacDougall K. When treatment is traumatic: an empirical review of interventions for pediatric medical traumatic stress. Am J Community Psychol. 2019;64(3-4):389-404.
19. Taddio A, Katz J, Ilersich AL, Koren G. Effect of neonatal circumcision on pain response during subsequent routine vaccination. Lancet. 1997;349(9052):599-603.
20. Racine N, Killam T, Madigan S. Trauma-informed care as a universal precaution: beyond the adverse childhood experiences questionnaire. JAMA Pediatr. 2020;174(1):5-6.
21. Shonkoff JP, Garner AS; Committee on Psychological Aspects of Child and Family Health; Committee on Early Childhood, Adoption, and Dependent Care; Section on Developmental and Behavioral Pediatrics. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129(1):e232-e246.
22. Coughlin ME. Trauma-Informed Care in the NICU: Evidence-Based Practice Guidelines for Neonatal Clinicians. Springer; 2017.
23. Butler SC, Huyler K, Kaza A, Rachwal C. Filling a significant gap in the cardiac ICU: implementation of individualized developmental care. Cardiol Young. 2017;27(9):1797-1806.
24. Saxe GN, Miller A, Bartholomew D, et al. Incidence of and risk factors for acute stress disorder in children with injuries. J Trauma. 2005;59(4):946-953.
25. Davidson F, Snow S, Hayden JA, Chorney J. Psychological interventions in managing postoperative pain in children: a systematic review. Pain. 2016;157(9):1872-1886.
26. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, Division of Violence Prevention. Essentials for Childhood: Creating Safe, Stable, Nurturing Relationships and Environments for All Children. Accessed December 22, 2022. https://www.cdc.gov/violenceprevention/pdf/essentials-for-childhood-framework508.pdf
27. Brosbe MS, Hoefling K, Faust J. Predicting posttraumatic stress following pediatric injury: systemic review. J Pediatric Psychol. 2011;37(7):579-584.
28. Marsac MI, Kassam-Adams N, Delahanty DL, Widaman KF, Barakat LP. Posttraumatic stress following acute medical trauma in children: a proposed model of bio-psychol-social processes during the peri-trauma period. Clin Child Fam Psychol Rev. 2014;17(4):399-411.
29. Olff M, Frijling JL, Kubzansky LD, et al. The role of oxycontin in social bonding, stress regulation and mental health: an update on the moderating effects of context and interindividual differences. Psychoneuroendocrinology. 2013;38(9):1883-1894.
30. Hughes DA, Baylin J. The Neurobiology of Attachment-Focused Therapy: Enhancing Connection and Trust in the Treatment of Children and Adolescents. W.W. Norton and Co; 2016.
31. Schulman M, Menschner C. Laying the groundwork for trauma informed care. Center for Health Care Strategies. January 2018. Accessed December 26, 2022. https://www.chcs.org/resorce/laying-groundwork.trauma-informed-care/
32. Romito B, Jewel J, Jackson M; AAP Committee on Hospital Care; Association of Child Life Professionals. Child Life services. Pediatrics. 2021;147(1):e2020040261.