Spring 2023 - Vol. 18, No. 1
SCIENTIFIC REPORT
Implementing CDC’s STEADI Fall Risk Screening
in an Outpatient Neurology Practice


Wu-Chen Vance
Wen Y. Helena Wu-Chen, MD
Neurologist, Neuro-Oncologist
Neuroscience Institute
Penn Medicine Lancaster General Health
Joan M. Vance, DPT, MBA
Administrative Director, Neuroscience
Neuroscience Institute
Penn Medicine Lancaster General Health
INTRODUCTION
Falls are a serious threat to the health and well-being of our aging population. More than 10,000 people in the United States turn 65 every day, and one out of four of these seniors falls each year.
1 The Centers for Disease Control and Prevention (CDC) reported approximately 36 million falls among this age group in 2018. Out of these, 8.4 million falls resulted in an injury that required medical visits or limited regular activities for one day.
2
Neurological disorders often result in functional and cognitive impairments that contribute to an even higher risk for falls in this population. When not fatal, falls often result in brain injury, hip fracture, and loss of independence, all of which may cause a substantial economic burden. Each year approximately $50 billion in medical expenses are incurred as a result of fatal and non-fatal falls.
3
The CDC’s response to this growing public health problem is an initiative called STEADI: Stopping Elderly Accidents, Deaths & Injuries. This initiative offers a robust set of tools and resources for clinicians, patients, caregivers, and pharmacists. These resources are available for review or download from the CDC at
cdc.gov/steadi/index.html.
The foundation of STEADI is an algorithm that integrates the 2010 clinical practice guidelines from both the American and British Geriatric Societies.
4 The algorithm
5 outlines the three core elements of:
- Screening.
- Assessments of modifiable risk factors.
- Interventions targeted at those risk factors.
Along with provider training and education, the CDC worked with early adopters to develop guidance on how to implement and evaluate a STEADI-based fall prevention program. Several health systems have successfully implemented the STEADI initiative into their outpatient practices, achieving high screening rates, reducing fall-related hospitalizations, and lowering associated health care expenditures.
6-8
Further, studies have proven that falls are preventable by assessing modifiable risk factors (e.g., gait abnormalities, environmental factors, medication adverse effects) and promoting evidence-based interventions like exercise, medication review, behavioral therapy, and vitamin D supplementation, among others (see Table 1).
9-11

The Centers for Medicare and Medicaid Services has included falls screening as one of 10 individual measures in the Medicare Shared Savings Program, targeting high-cost chronic conditions, preventive care, and patient safety.
Traditionally, falls screening at Penn Medicine Lancaster General Health Physicians outpatient services clinics has been performed without a standardized workflow/Epic tool; instead, each department chose which screening tools and interventions to use.
Primary care practices have often used the Timed Up and Go test during Annual Wellness screenings. Although validated in geriatric populations
12 when there is lack of standardization, it is challenging to demonstrate compliance for the Medicare Shared Savings Program.
The objective of this study, which is ongoing, is to facilitate a standardized electronic medical record (EMR) approach to falls screening using the STEADI algorithm and to put in place individual and multifactorial interventions that reduce fall risk. This is a quality and safety improvement initiative.
LGHP Neurology initiated a pilot to facilitate the use of the STEADI guidelines by hardwiring the process into the EMR. The result is an opportunity to assess the individual contributors to risk and modifiable risk factors, as well as implement effective strategies targeted at the identified risk factors.
Our team identified the critical success factor for this pilot as the ability to hardwire screening tools into the EMR. As a result, two tools were built into Epic to help facilitate the process. The Neurology Department rolled out its pilot on January 1, 2022, and began collecting data for new patients who are 65 years of age and older. This phase of the pilot was completed on December 31, 2022.
METHODS
This study was conducted at the neurology outpatient services practice of the LGHP Neuroscience Institute. All neurology providers participated in the study. Data from patients who met the age requirements were included. The first tool is a 12-question self-assessment with built-in clinical calculators (see Fig. 1). It is launched as a MyChart questionnaire that patients can complete prior to an upcoming appointment. Screening is considered abnormal or at risk when a patient scores 4 or higher.
The second tool is the short-screening three-question assessment (see Fig. 2) used during the rooming process, which is performed by the nurse. This is used only if the patient did not complete the first tool. A patient is considered at risk if the score is 1 or higher.

For any abnormal results, a Best Practice Alert (BPA) indicates the clinician needs to evaluate for risk factors and discuss an intervention plan. In addition to triggering this evaluation, the BPA helps facilitate and document the plan of care via a Smartset. Options within the Smartset include:
- Educational handouts.
- Option to refer to LGHP Physical Therapy, PMR, or external physical therapy.
- Documentation that a current fall prevention plan may already be in place.
- Documentation that the patient declines intervention.
Patients who screen positive are automatically eligible for educational handouts, which are auto-assigned to the after-visit summary. Orders 2-4 are assigned at the discretion of the clinician.
Data from the first quarter of 2022 showed that compliance with completion of the full self-assessment was low and the nursing Best Practice Alert was frequently firing. As part of a rapid cycle improvement process, in May 2022 the team converted to completing a short screening tool as standard rooming process for all new patients.
RESULTS
To measure the success of the project, the system tracks several key components of the study, including the number of patients and age distribution of patients screened through self-assessment or by nursing staff, and compliance of providers in using the BPA as a tool to evaluate and document an intervention for those patients determined to be at risk.
Currently, we have data collected from January 4 through October 30, 2022. A total of 357 patients were screened; 238 patients (67%) were at risk of fall. Ages ranged from 65 to 91 years (see Fig. 3), and female-to-male ratio was 1.2:1.
 Fig. 3. Percent of each age cohort in study considered at risk for fall as of October 2022.
Fig. 3. Percent of each age cohort in study considered at risk for fall as of October 2022.
Figs. 4 and 5 show our screening and BPA compliance by month. Fig. 4 further shows that the conversion to completing a short screening tool as standard rooming process for all new patients significantly increased compliance.
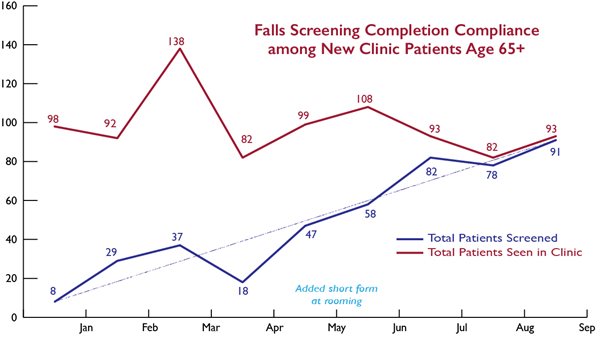 Fig. 4. This graph represents falls screening compliance by new patients or nursing staff. The most desirable outcome is to have Total Patients Screened = Total Patients Seen in Clinic.
Fig. 4. This graph represents falls screening compliance by new patients or nursing staff. The most desirable outcome is to have Total Patients Screened = Total Patients Seen in Clinic.
 Fig. 5. This graph demonstrates provider compliance with the BPA tool for patients who screen positive for fall risk. The most desirable outcome is to have Total BPA Interventions = Total Patients Identified at Risk.
DISCUSSION
Fig. 5. This graph demonstrates provider compliance with the BPA tool for patients who screen positive for fall risk. The most desirable outcome is to have Total BPA Interventions = Total Patients Identified at Risk.
DISCUSSION
Several Penn Medicine Lancaster General Health departments actively contributed to the first stage of this project. Collaboration with Information Services was crucial in the development of the two screening tools in our Epic system. Active participation by the nursing staff allowed us to capture and screen the designated patients.
In addition, we initiated chart reviews on at-risk patients who did not show activity on the Best Practice Alert report. It was noted that on occasion, providers were documenting an action plan to address risk outside of the Best Practice Alert. This represents an opportunity for further process improvement.
Information Services continues to work with the neurology team to create new solutions to better enhance our intervention plan documentation. More data will be coming in the year ahead. We also expect to follow-up with patients who have not been screened or who had a positive STEADI fall risk screen in the last 11 months, to see if any part of the action plan was beneficial in reducing falls. Future studies will also target the effectiveness of delivering intervention resources to the community.
Preliminary data validated the easy access of the CDC’s STEADI screeners, as demonstrated in our high compliance rate. By identifying our high-risk patients and providing them with resources, we hope to reduce fall-related injuries and eventually reduce associated health care costs.
Based upon the results, the success of this tool may be applicable to primary care, geriatrics, and other interested departments.
REFERENCES
1. STEADI — Older Adult Fall Prevention. Centers for Disease Control and Prevention. Updated July 26, 2021. Accessed December 19, 2022.
https://www.cdc.gov/steadi/
2. Moreland B, Kakara R, Henry A. Trends in nonfatal falls and fall-related injuries among adults aged ≥65 years — United States, 2012– 2018.
MMWR Morb Mortal Wkly Rep. 2020;69:875-881.
3. Florence CS, Bergen G, Atherly A, Burns ER, Stevens JA, Drake C. Medical costs of fatal and nonfatal falls in older adults.
J Am Geriatr Soc. 2018;66:693-698.
4. Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons.
J Am Geriatr Soc. 2011;59(1):148-157.
5. Algorithm for Fall Risk Screening, Assessment, and Intervention. Centers for Disease Control and Prevention. 2019. Accessed January 30, 2023.
https://www.cdc.gov/steadi/pdf/STEADI-Algorithm-508.pdf
6. Eckstrom E, Parker EM, Lambert GH, Winkler G, Dowler D, Casey CM. Implementing STEADI in academic primary care to address older adult fall risk.
Innov Aging. 2017;1(2):igx028.
7. Casey CM, Parker EM, Winkler G, Liu X, Lambert GH, Eckstrom, E. Lessons learned from implementing CDC’s STEADI falls prevention algorithm in primary care.
Gerontologist. 2017;57(4):787-796.
8. Johnston YA, Bergen G, Bauer M, et al. Implementation of the Stopping Elderly Accidents, Deaths, and Injuries Initiative (STEADI) in primary care: an outcome evaluation.
Gerontologist. 2019;59(6):1182-1191.
9. Bergen G, Stevens MR, Kakara R, Burns ER. Understanding modifiable and unmodifiable older adult fall risk factors to create effective prevention strategies.
Am J Lifestyle Med. 2019;15(6):580-589.
10. Guirguis-Blake JM, Michael YL, Perdue LA, Coppola EL, Beil TL, Thompson JH.
Interventions to Prevent Falls in Community-Dwelling Older Adults: A Systematic Review for the U.S. Preventive Services Task Force. Rockville (MD): Agency for Healthcare Research and Quality (US); April 2018.
11. Ang GC, Low SL, How CH. Approach to falls among the elderly in the community.
Singapore Med J. 2020;61(3):116-121.
12. Christopher A, Kraft E, Olenick H, Kiesling R, Doty A. The reliability and validity of the Timed Up and Go as a clinical tool in individuals with and without disabilities across a lifespan: a systematic review.
Disabil Rehabil. 2021;43(13):1799-1813.
13. Rubenstein LZ, Vivrette R, Harker JO, et al. Validating an evidence-based, self-rated fall risk questionnaire (FRQ) for older adults.
J Safety Res. 2011;42(6):493-499.