Summer 2022 - Vol. 17, No. 1
CHOOSING WISELY XXXVII & TOP TIPS
Recommendations from the American Society of Nuclear Cardiology
and the American Urogynecologic Society
Alan S. Peterson, MD
Emeritus Director, Environmental and Community Medicine
Walter L. Aument Family Health Center
This is my 37th article on Choosing Wisely from the American Board of Internal Medicine (ABIM) Foundation. As noted in previous issues of
JLGH, each specialty group is developing “Five or More Things That Physicians and Patients Should Question.” All items are developed to encourage discussion between physicians and their patients about which tests and procedures are best in each case. Additional resources are available online at
choosingwisely.org.
I. RECOMMENDATIONS OF THE AMERICAN SOCIETY OF NUCLEAR CARDIOLOGY (ASNC)
1. Stress cardiac imaging or coronary angiography should not be performed in patients without cardiac symptoms unless high-risk markers are present. Asymptomatic, low-risk patients account for up to 45% of inappropriate stress testing. Testing should be performed only when the following findings are present: diabetes in patients older than 40 years old, peripheral arterial disease, and greater than 2% yearly coronary heart disease event rate.
1
2. Cardiac imaging should not be performed for patients who are at low risk. Chest pain patients at low risk of cardiac death and myocardial infarction (based on history, physical exam, electrocardiograms, and cardiac biomarkers) do not merit stress radionuclide myocardial perfusion imaging or stress echocardiography as an initial testing strategy if they have a normal electrocardiogram (without baseline ST-abnormalities, left ventricular hypertrophy, pre-excitation, bundle branch block, intra-ventricular conduction delay, paced rhythm, or on digoxin therapy) and are able to exercise.
3. Radionuclide imaging should not be performed as part of routine follow-up in asymptomatic patients. Performing stress radionuclide imaging in patients without symptoms on a serial or scheduled pattern (e.g., every one to two years or at heart procedure anniversary) rarely results in any meaningful change in patient management. It could lead to unnecessary invasive procedures and excess radiation exposure. An exception to this rule would be for patients more than five years after a bypass operation.
4. Cardiac imaging as a pre-operative assessment in patients should not be performed in those scheduled to undergo low- or intermediate-risk non-cardiac surgery. In those patients or in those with no cardiac symptoms or clinical risk factors, non-invasive testing is not useful. This type of testing does not change the patient’s clinical management or outcomes and may result in increased cost.
5. Whenever possible, use methods to reduce radiation exposure in cardiac imaging, including not performing such tests when limited benefits are likely. The key step to reduce or eliminate radiation exposure is appropriate selection of any test or procedure for a specific person, in keeping with medical society recommendations such as appropriate use criteria.
2
II. RECOMMENDATIONS OF THE AMERICAN UROGYNECOLOGIC SOCIETY (AUGS)
1. Fluoroquinolone antibiotics should be avoided for the first-line treatment of uncomplicated urinary tract infections (UTIs) in women. For women with uncomplicated UTIs (defined as premenopausal, non-pregnant women with no known urologic abnormalities or comorbidities), fluoroquinolone antibiotics should not be considered first-line treatment. Although fluoroquinolones are efficacious in three-day regimens, they have a higher risk of ecological adverse events, such as increasing multidrug-resistant organisms. Therefore, use these drugs only for the treatment of acute UTIs for women who should not be prescribed first-line regimens such as nitrofurantoin, trimethoprim-sulfamethoxazole, or fosfomycin.
3
2. Cystoscopy, urodynamics, or diagnostic renal and bladder ultrasound should not be performed in the initial workup of an uncomplicated overactive bladder patient. The initial evaluation of an uncomplicated patient presenting with symptoms should include history, physical examination, and urinalysis. In some cases, urine culture, post-void residual urine assessment, and bladder diaries may be helpful. More invasive testing should be reserved for complex patients, patients who have failed initial therapies (i.e., behavioral therapies and medications), or patients who have abnormal findings on their initial evaluation.
3. Pessaries should not be excluded as a treatment option for pelvic organ prolapse. Non-surgical treatment options for pelvic organ prolapse include pessaries, which are removable devices that are placed into the vagina to support the prolapsed organs (i.e., uterus, vagina, bladder, and/or rectum). A pessary trial can be offered to almost all women with pelvic organ prolapse. Exceptions include women with an active vaginal infection and those who are unable to follow through with treatment.
4. Synthetic or biologic grafts should be avoided in primary rectocele repairs. Posterior vaginal repair of rectocele is performed for women with symptoms of a posterior vaginal wall bulge or difficulty with defecation. The repair involves suturing the posterior vaginal wall and perineal tissue. The addition of synthetic or biologic grafts to this repair does not improve patient outcomes.
5. Removing ovaries at hysterectomy should be avoided in pre-menopausal women with normal cancer risk. There is evidence from observational studies that surgical menopause may negatively impact cardiovascular health and all-cause mortality. This is particularly important in patients with a personal or strong family history of cardiovascular disease or stroke. Women with an average risk of ovarian cancer are defined as women who do not have a documented germline mutation or who do not have a strong family history suspicious for a germline mutation and are undergoing a hysterectomy for benign conditions.
4
Top Tips
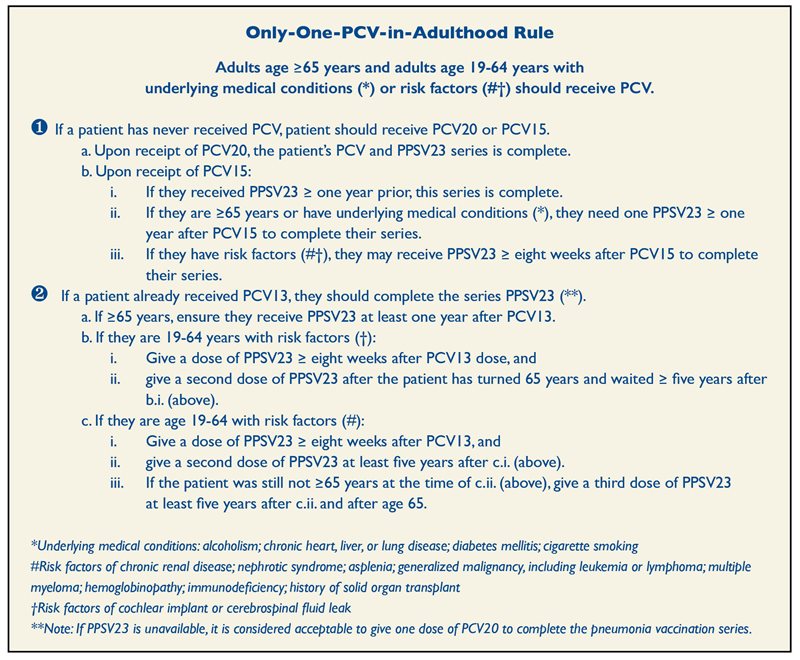
RECOMMENDATIONS SIMPLIFIED FOR PNEUMOCOCCAL VACCINATION
A new policy has simplified the pneumococcal vaccination recommendations of the Advisory Committee on Immunization Practices (ACIP) of the Centers for Disease Control and Prevention (CDC). The updated recommendations were published in the CDC’s
Morbidity and Mortality Weekly Report in January of this year.
5
Noting that the 13-valent pneumococcal conjugate vaccine (PCV13) and 23-valent pneumococcal polysaccharide vaccine (PPSV23) were recommended for use in U.S. adults, with the recommendations varying by age and risk group, Miko Kobayashi, MD, from the CDC in Atlanta, and colleagues reviewed the evidence framework to develop recommendations for use of 20-valent PCV (PCV20) and 15-valent PCV (PCV15). PCV20 and PCV15 were licensed in 2021 by the Food and Drug Administration for adults ages 18 years and older.
As a result of this review, ACIP now recommends an only-one-PCV-in-adulthood rule (below).
PPSV23 had been recommended for use in the United States since the 1980s for adults ages 65 years and older, and for younger adults with underlying conditions that increased their risk for pneumococcal disease. PCV13 was first recommended for use in children in the United States in 2010; indirect effects from its use in children reduced PCV13-type pneumococcal disease in all adult groups.
In 2012, ACIP recommended administration of PCV13 in series with PPSV23 for adults with immunocompromising conditions, cerebrospinal leaks, or cochlear implants, and in 2014, the recommendation was extended to all adults ages 65 and older.
GAS STOVES POLLUTING EVEN WHEN TURNED OFF
In an article published by the American Chemical Society, researchers noted that natural gas (methane) stoves in over 40 million U.S. residences release methane — a potent greenhouse gas — through post-meter leaks and incomplete combustion.
6 Almost three-quarters of the methane found was emitted from the stoves when they were not turned on.
The researchers quantified methane released in 53 homes during all phases of stove use: steady-state off (appliance not in use), steady-state on (during combustion), and transitory periods of ignition and extinguishment. They found:
Using a 20-year timeframe for methane, annual methane emissions from all gas stones in U.S. homes have a climate impact comparable to the annual carbon dioxide emissions of 500,000 cars. In addition to methane emissions, co-emitted health-damaging air pollutants such as nitrogen oxides (NOx) are released into home air and can trigger respiratory diseases.
6
Other pollutants associated with gas stoves include formaldehyde, particulate matter (such as PM2.5), and carbon monoxide. A significant amount of nitrogen oxides entering the homes of people with asthma and to heat pans. But this transition to electric-powered other health conditions is obviously not a good finding.
In 32 homes, the researchers measured NO and will be difficult. NO
2 emissions and found them to be linearly related Why is this important to our patients? Researchers to the amount of natural gas burned. Their data suggest that “families that don’t use their range hoods that exposure to ambient air pollution contributed to or who have poor ventilation can surpass the [one-hour] national standard of NO
2 (100 ppb) within a few minutes of stove usage, particularly in smaller kitchens.” And even when U.S. gas stoves are not running, they are emitting 2.6 million tons of methane into the air each year.
We don’t need to fix every gas stove to eliminate this source of emissions, as there is already a better solution: replace these with stoves that run on electricity. The best contender to replace the gas stove is the induction stove, which uses a magnetic field to heat pans. But this transition to electric-powered cooking without city, state, and even federal policy will be difficult.
Why is this important to our patients? Researchers in a toxicology article published in 2020 concluded that exposure to ambient air pollution contributed to autism spectrum disorders and that oxytocin receptor protein may serve as part of the mechanism linking them.
7
It has even been suggested that airborne particulate matter may act like a trojan horse, representing an effective delivery system for diverse environmental toxicants to reach the brain. Previous studies reported that simultaneous exposure to particulate matter and gaseous pollutants during pregnancy have been associated with autism spectrum disorder.
8,9
AMERICAN COLLEGE OF PHYSICIANS (ACP) RELEASES NEW CLINICAL GUIDELINES ON DIVERTICULITIS10,11
Acute diverticulitis is usually uncomplicated, causing only localized inflammation. However, in about 12% of cases, there can be complications.
Complicated diverticulitis is an inflammation association with an abscess, a phlegmon, a fistula, an obstruction, bleeding, or perforation. The chance of recurrence is approximately 22%.
Approximately 95% of patients with diverticula have sigmoid diverticula, and 5% to 10% of those with diverticulosis may develop acute diverticulitis, increasing with age.
Due to recent theory that diverticulitis may be more inflammatory than infections, the ACP in early 2022 released new guidelines as follows:
- Use abdominal CT imaging when there is diagnostic uncertainty with suspected acute diverticulitis (conditional recommendation: low-certainty evidence).
- Manage most patients with acute uncomplicated diverticulitis in an outpatient setting (conditional; low-certainty).
- Characterize uncomplicated diverticulitis by absence of frank perforation, obstruction, fistula, or abscess on CT.
- Initially manage select patients with acute diverticulitis without antibiotics (conditional; low-certainty).
For adults with recent episodes of acute left-sided colonic diverticulitis:
- Refer for a colonoscopy after an initial episode of complicated diverticulitis for those who have not had recent colonoscopy (conditional; low-certainty).
- Do not use mesalamine to prevent recurrent diverticulitis (strong; high-certainty).
- Discuss elective surgery to prevent recurrence after initial treatment in those who have either uncomplicated diverticulitis that is persistent or recurs frequently, or complicated diverticulitis (conditional; low-certainty).
- Personalize the decision on whether to treat with surgery based on a discussion of potential benefits, harms, costs, and patient preferences.
If antibiotics are indicated in the ambulatory setting, amoxicillin-clavulanate (Augmentin
®) alone should be favored over a combination of fluoroquinolones and metronidazole due to Food and Drug Administration advisement regarding reserving fluoroquinolones for conditions with no alternative treatment options.
REFERENCES
1. Hendel RC, Abbott BG, Bateman TM, et al. Roll of radionuclide myocardial perfusion imaging for asymptomatic individuals.
J Nucl Cardiol. 2011;18(1):3-15.
2. Cerqueira MD, Allman KC, Ficaro EP, et al. Recommendations for reducing radiation exposure in myocardial perfusion imaging.
J Nucl Cardiol. 2010;17(4):709-718.
3. Hooton, TM. Clinical practice. Uncomplicated urinary tract infection.
N Engl J Med. 2012;366(11):1028-1037.
4. Berek JS, Chalas E, Edelson M, et al. Prophylactic and risk-reducing bilateral salpingo-oophorectomy: recommendations based on risk of ovarian cancer.
Obstet Gynecol. 2010116(3):733-743.
5. Kobayashi M, Farrar JL, Gierke R, et al. Use of 15-Valent Pneumococcal Conjugate Vaccine and 20-Valent Pneumococcal Conjugate Vaccine among U.S. adults: updated recommendations of the Advisory Committee on Immunization Practices — United States, 2022.
MMWR Morb Moral Wkly Rep. 2022;71(4):109-117.
6. Leibel ED, Finnigan CJ, Ouyang Z, et al. Methane and NOx emissions from natural gas stoves, cooktops, and ovens in residential homes.
Environ Sci Technol. 2022;56(4):2529-2539.
7. Emam B, Shahsavni A, Khodagholi F, et al, Effects of PM2.5 and gasses exposure during prenatal and early-life on autism-like phenotypes in male rat offspring.
Part Fibre Toxicol. 2020;17(1):8.
8. Raz R, Roberts AL, Lyall K, et al. Autism spectrum disorder and particulate matter air pollution before, during, and after pregnancy: a nested case-control analysis with the Nurses’ Health Study II Cohort.
Environ Health Perspect. 2015;123(3):264-270.
9. Talbott EO, Arena VC, Rager JR, et al. Fine particulate matter and the risk of autism spectrum disorder.
Environ Res. 2015;140:414-420.
10. Quaseem A, Etxeandia-Ikobaltzeta I, Lin JS, et al. Diagnosis and management of acute left-sided colonic diverticulitis: a clinical guideline from the American College of Physicians.
Ann Intern Med. 2022;175(3):399-415.
11. Quaseem A, Etxeandia-Ikobaltzeta I, Lin JS, et al. Colonoscopy for diagnostic evaluation and interventions to prevent recurrence after acute left-sided colonic diverticulitis: a clinical guideline from the American College of Physicians.
Ann Intern Med. 2022;175(3):416-431.