Summer 2022 - Vol. 17, No. 1
SCIENTIFIC REPORT
Emergency Contraceptives
Breaking Down the Indications for Use
Emily S. Kirchner, MD, MA
Associate Director, Family Medicine Residency Program
Penn Medicine Lancaster General Health
CLINICAL CASE
A 19-year-old nulliparous patient you saw for well child care until the patient left for college calls your office and asks for an urgent call back. The patient had sex for the first time yesterday. The condom broke, and the patient is worried about pregnancy. The patient has been taking a combined hormonal contraceptive pill since high school and has missed a few doses. The patient's last menstrual period was two weeks ago. What options does the patient have to avoid an undesired pregnancy?
INTRODUCTION
Emergency contraception (EC) reduces the risk of pregnancy after unprotected sexual intercourse. People use EC when birth control is misused or fails, when a condom breaks, or after sexual assault. Emergency contraception does not interfere with an existing pregnancy and does not cause abortion.
Some patients may feel ambivalent about formalizing their contraception plan when asked in their physician’s office, but have a clear preference to prevent pregnancy when faced with this possibility later on. Unfortunately, many sexually active people in relationships do not have full autonomy in their reproductive decision-making and are prevented from using contraception.
However, oral EC offers a way to reduce the risks for and consequences of undesired pregnancy. Emergency contraception is a critical part of sexual and reproductive health care.
Because all forms of emergency contraception must be administered soon after unprotected intercourse and because accessing EC can be time consuming, it is reasonable and recommended to provide prescriptions for oral EC in advance so patients may use emergency contraception as soon as possible when it is needed. This practice is called
advanced provision. A 2007 Cochrane Review demonstrated that advanced provision was not associated with negative sexual or reproductive health outcomes.
1
In 2019, the American Academy of Pediatrics released an updated policy statement on EC recommending that pediatricians provide emergency contraception to adolescents and young adults who have an urgent need and recommended advanced provision of emergency contraceptive pills. Furthermore, they recommended:
[All] adolescents receive counseling about EC as part of routine anticipatory guidance in the context of a discussion on sexual health and family planning regardless of current intentions for sexual behavior. In addition, it is important that information about EC be included in all contraceptive and STI counseling for adolescents wherever these visits occur, including emergency departments, clin.ics, and hospitals. Information provided should include indications for use and options for access, including over-the-counter availability and advance prescription or supply if available in the clinic. It is important that pediatricians also provide this counseling to adolescents with physical and cognitive disabilities and their parents.2
They went on to suggest that regarding policy, health care professionals “should advocate for low-cost or free, nonprescription access … for teenagers regardless of age and insurance coverage of EC without cost sharing to further reduce cost barriers.”
DEMOGRAPHICS
Use of emergency contraception is increasing. In 2015, 23% of sexually active women aged 15-44 in the United States reported they had used EC, compared to 11% in 2008. Increased use of EC is seen across demo. Graphic groups — regardless of age, race and ethnicity, income level, education, religion, marital status, and women’s number of births.
During the same period, the Affordable Care Act’s contraceptive coverage guarantee took effect, and some forms of EC became available over the counter. Of note, this data only includes oral EC and does not include intrauterine devices (IUDs) for EC.
3
METHODS AND CLINICAL CONSIDERATIONS
There are currently a number of safe and effective forms of EC: the Copper TCu380A IUD and levonorgestrel 52 mg IUDs, oral levonorgestrel, and oral ulipristal. Patients may also utilize large doses of combined hormonal contraceptives; this regimen is known as the Yuzpe method.
The most effective forms of EC are IUDs. The copper IUD (Paragard®) and the 52 mg levonorgestrel IUDs (Mirena® and Liletta®) can all be used for EC when inserted within five days of unprotected inter.course.
4 The pregnancy rate following IUD insertion for EC is less than 1%. IUDs work as EC regardless of BMI.
5 They are an excellent choice for anyone who wants ongoing highly effective contraception (for up to 12 years with the copper IUD and up to seven with a levonorgestrel-containing IUD). They are the most expensive form of EC — both for the device and required insertion.
The mechanism of action of an IUD for EC is thought to be inhibition of sperm function and inhibition of fertilization through direct effects on sperm, as well as thickening of cervical mucous and endometrial receptivity, thus creating an inhospitable environment. There is no evidence to demonstrate that IUDs have post-implantation effects.
6,7,8,9
Risks of IUD insertion include pelvic pain or abdominal cramping, vaginal bleeding, and much lower risks of infection and uterine perforation.
If pregnancy occurs despite IUD as EC, the patient should receive options counseling. The IUD will need to be removed, and the patient can initiate prenatal care or abortion care.
Two oral forms of EC are currently available. Both oral levonorgestrel and ulipristal prevent ovulation. Neither method will prevent ovulation after luteinizing hormone (LH) peaks, nor will they interfere with implantation of a fertilized egg or an established pregnancy.
10
Levonorgestrel (abbreviated LNG, brand names PlanB® or Next Choice®) is the most commonly used and most available method. It works to inhibit ovulation by blocking the luteinizing hormone surge, which subsequently prevents follicle development. LNG loses efficacy if the LH surge has started. This method will not work if fertilization has already occurred as it does not affect implantation of a fertilized egg.
11
The efficacy decreases with increasing time between unprotected intercourse and LNG administration, thus it must be taken as soon as possible within 72 hours. Because of the urgency of medication administration, advanced provision of EC, as described above, is advisable. Evidence suggests oral LNG loses efficacy for individuals with BMI >26.
12,13 Efficacy also varies depending on the timing of unprotected intercourse within an individual’s menstrual cycle; LNG is not as effective once a patient has ovulated (typically day 14 of her cycle). Another form of EC should be considered.
If a patient desires ongoing contraception at the time of LNG use, any contraceptive method can be prescribed on the same date. There is no interference between levonorgestrel EC and other birth control methods. A typical seven-day backup method or abstinence period should be recommended. Breastfeeding after use of LNG is safe.
All levonorgestrel EC products are now approved for over-the-counter sale without age or gender restrictions, but the reality of access may vary in each community. The original levonorgestrel EC was approved in 1999 as a two-dose prescription product. In 2006, LNG was approved for nonprescription sale for any.one over the age of 18. And in 2009, the limit was lowered again to age 17. The product was available to women under age 17, but required a prescription and was held behind the counter so that age restriction could be enforced prior to purchase. Plan B One-Step®, an LNG product, was approved for unrestricted sale in 2013, but the age-restricted label remained for generics until 2014.
14
Patients should be informed that LNG is available to anyone regardless of gender or age without a prescription. They may have to talk to pharmacy staff, as some stores keep the product behind the register or in locked boxes to prevent theft. If purchased over the counter (either in stores or online), the cost can be $15 to $50. If prescribed, the medication is usually covered as part of the Affordable Care Act’s contraceptive coverage guarantee. It is on Pennsylvania’s Statewide Preferred Drug List and, if prescribed, is available with no co-pay.
Ulipristal (abbreviated UPA, brand name ella®) is a selective progesterone receptor modulator that works by mimicking and blocking progesterone, which can delay ovulation before and even after the LH surge has begun. There is no evidence that UPA interferes with fertilization or disrupts an established pregnancy.
15
UPA is more effective than LNG and can work for five days after unprotected intercourse.
11,16 Patients should be counseled to take the medication as soon as possible. UPA loses efficacy in higher BMI individuals and may be ineffective for individuals with BMI >35.
13 It is important to explain the effect larger body size may have on efficacy of ulipristal EC so a patient may make an informed choice about EC. UPA requires a prescription and is usually available for $40 to $50 with a GoodRx coupon. It can be found at low cost on-line and/or from international pharmacies. Advanced provision of ulipristal EC is advisable.
The Centers for Disease Control and Prevention’s (CDC’s) Medical Eligibility Criteria do not restrict UPA while breastfeeding, but do recommend expressing and discarding breast milk for 24 hours after taking UPA based on limited evidence.
Progestin-containing contraceptive methods may interfere with UPA. Any desired ongoing contraception — that is, subsequent use of progestin-containing contraceptives (including progestin-only birth control pills, combined estrogen-progestin pills, patch or ring, depot-medroxyprogesterone acetate injection, or etonogestrel implant) — must be delayed at least five days following UPA administration.
Despite increased efficacy of UPA compared to levonorgestrel EC, it is not always available in pharmacies for same-day use. A number of studies have investigated accessibility of LNG and UPA in pharma.cies.
17,18 A 2021 survey of southwestern Pennsylvania pharmacies revealed that only 5% of pharmacies had ulipristal in stock.
19 This author called four pharmacies in Lancaster (including one LGH Convenience Pharmacy and three retail pharmacies), and none had UPA in stock for same-day use.
For both forms of oral EC, patients may experience nausea, vomiting, headache, dizziness, abdominal pain, or breast pain.
20 Individuals should be counseled to take a home pregnancy test if they have not had a period within a week of their expected cycle.
Efficacy for both oral EC methods decreases with repeated unprotected intercourse, especially during the fertile window. The CDC’s Medical Eligibility Criteria may be referenced for further questions about medication interactions, contraindications, or safety.
21
Clinicians may be asked about the Yuzpe method — named for Canadian obstetrician-gynecologist Albert Yuzpe, MD. This method requires specific combinations of combined hormonal contraceptive pills (100 mcg ethinyl estradiol and 0.5 mg levonorgestrel) taken twice, 12 hours apart. A number of common birth control brands can be arranged in the appropriate doses; lists of these combinations can be found online.
This method is the least effective of all emergency contraceptives. Side effects including nausea, vomiting, spotting, and headaches are common. It is reasonable to offer an antiemetic to help with these side effects. With the other available and effective forms of long-acting reversible contraception and EC, the Yuzpe method has fallen out of common practice. However, for patients who already have an oral contraceptive prescription at home, it is convenient, private, and does not incur additional cost.
In-person or telehealth visits, pelvic exams, or pregnancy tests are not required for EC prescriptions. Either persistent bleeding or delayed bleeding following oral EC use should prompt an evaluation for pregnancy.
22,23
If a patient suspects pregnancy, it is reasonable to test for pregnancy and offer options counseling. If pregnancy occurs despite use of emergency contraceptive pills (either LNG or UPA), there are no known adverse outcomes to the developing fetus. Patients should be offered options counseling and appropriate follow-up for prenatal or abortion care.
Repeated use of EC is not harmful, nor does it lead to infertility.
24,25 For a visual guide to choosing an emergency contraceptive method, see Fig. 1.
 OPPORTUNITIES
OPPORTUNITIES
Anyone who is having sex or plans to become sexually active should have access to EC. Access to EC includes medically accurate, evidence-based counseling, same-day availability of prescriptions and procedures, advanced provision, and insurance coverage for all methods.
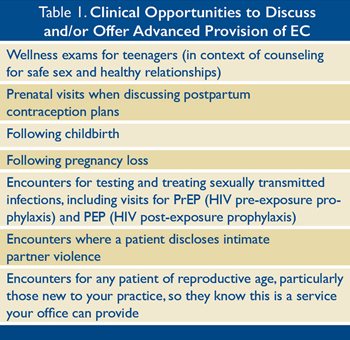
Emergency contraception is an appropriate topic for discussion in a variety of patient encounters (see Table 1).
CONCLUSION
The patient described at the beginning of this article is a candidate for LNG, UPA, or an IUD for emergency contraception (see Fig. 1). Since it is approximately day 14 of their-menstrual cycle, LNG may be ineffective. If they would like to use UPA and subsequently continue their oral contraceptive, there should be a five-day window before resuming their birth control pill. They could also be counseled on the Yuzpe method if desired.
Preventing an undesired pregnancy is an emergency. Patients deserve education about EC as part of their contraception counseling. Clinicians should be aware of the forms of EC, understand the indications for use, and be prepared to deliver patient-centered care including EC for our patients.
REFERENCES
1. Polis CB, Schaffer K, Blanchard K, Glasier A, Harper CC, Grimes DA. Advance provision of emergency contraception for pregnancy prevention (full review).
Cochrane Database Syst Rev. 2007;(2):CD005497.
2. Upadhya KK; Committee on Adolescence. Emergency contraception.
Pediatrics. 2019;144(6):e20193149.
3. Hussain R, Kavanaugh ML. Changes in use of emergency contraceptive pills in the United States from 2008 to 2015.
Contracept X. 2021;3:100065.
4. Turok DK, Gero A, Simmons RG, et al. Levonorgestrel vs. copper intrauterine devices for emergency contraception.
N Engl J Med. 2021;384(4):335-344.
5. Xu H, Wade JA, Peipert JF, Zhao Q, Madden T, Secura GM. Contraceptive failure rates of etonogestrel subdermal implants in overweight and obese women.
Obstet Gynecol. 2012;120(1):21-26.
6. Ortiz ME, Croxatto HB. Copper-T intrauterine device and levonorgestrel intrauterine system: biological bases of their mechanism of action.
Contraception. 2007;75(6 Suppl):S16-S30.
7. Dean G, Schwarz EB. Intrauterine devices. In: Trussell J, Cwiak C, Cason P, et al., eds.
Contraceptive Technology. 21st ed. Ayer Company Publishers; 2018:157.
8. Mahmood T, Saridogan E, Smutna S, Habib AM, Djahanbakhch O. The effect of ovarian steroids on epithelial ciliary beat frequency in the human Fallopian tube.
Hum Reprod. 1998;13(11):2991-2994.
9. Gemzell-Danielsson K, Berger C, Lalitkuma, PGL. Emergency contraception — mechanisms of action.
Contraception. 2013;87(3): 300-308.
10. Brache V, Cochon L, Deniaud M, Croxatto HB. Ulipristal acetate prevents ovulation more effectively than levonorgestrel: analysis of pooled data from three randomized trials of emergency contraception regimens.
Contraception. 2013;88(5):611-618.
11. Marions L, Cekan SZ, Bygdeman M, Gemzell-Danielsson K. Effect of emergency contraception with levonorgestrel or mifepristone on ovarian function.
Contraception. 2004;69(5):373-377.
12. Kapp N, Abitbol JL, Mathé H, et al. Effect of body weight and BMI on the efficacy of levonorgestrel emergency contraception.
Contraception. 2015;91(2):97-104.
13. Glasier A, Cameron ST, Blithe D, et al. Can we identify women at risk of pregnancy despite using emergency contraception? Data from randomized trials of ulipristal acetate and levonorgestrel.
Contraception. 2011;84(4):363-367.
14. Cleland K, Bass J, Doci F, Foster AM. Access to emergency contraception in the over-the-counter era.
Womens Health Issues. 2016;26(6):622-627.
15. Li HWR, Resche-Rigon M, Bagchi IC, Gemzell-Danielsson K, Glasier A. Does ulipristal acetate emergency contraception (ella®) interfere with implantation?
Contraception. 2019;100(5):386-390.
16. Richardson AR, Maltz FN. Ulipristal acetate: review of the efficacy and safety of a newly approved agent for emergency contraception.
Clin Ther. 2012;34(1):24-36.
17. Shigesato M, Elia J, Tschann M, et al. Pharmacy access to Ulipristal acetate in major cities throughout the United States.
Contraception. 2018;97(3):264-269.
18. French VA, Mattingly TL, Rangel AV, Shelton AU. Availability of ulipristal acetate: a secret shopper survey of pharmacies in a metropolitan area on emergency contraception.
J Am Pharm Assoc (2003). 2019;59(6):832-835.
19. Orr K, Chin J, Cuddeback M, et al. Pharmacy availability of emergency contraception in southwestern Pennsylvania: a simulated patient study.
Contracept X. 2021;3:100068.
20. Practice Bulletin No. 152: Emergency contraception.
Obstet Gynecol. 2015;126(3):e1-e11.
21. Curtis KM, Tepper NK, Jatlaoui TC, et al. U.S. medical eligibility criteria for contraceptive use, 2016.
MMWR Recomm Rep. 2016;65(3):1-103.
22. Webb A, Shochet T, Bigrigg A, et al. Effect of hormonal emergency contraception on bleeding patterns.
Contraception. 2004; 69(2):133-135.
23. Shen J, Che Y, Showell E, Chen K, Cheng L. Interventions for emergency contraception.
Cochrane Database Syst Rev. 2017; 8(8):CD001324.
24. Emergency Contraception. World Health Organization. Published November 9, 2021. Accessed May 12, 2022.
https://www.who.int/news-room/fact-sheets/detail/emergency-contraception
25. Trussell J, Cleland K, Schwarz EB. Emergency contraception. In: Trussell J, Cwiak C, Cason P, et al., eds.
Contraceptive Technology. 21st ed. Ayer Company Publishers; 2018:329-365.