
Fall 2021 - Vol. 16, No. 3
BEST OF THE JOURNAL
Zombie Infections and Other Infectious Disease Complications of Global Warming1
Joseph M. Kontra, M.D.
Chief, Infectious Diseases
Penn Medicine Lancaster General Health
Editor’s Note: When this article first appeared in Spring 2017, it was not yet universally recognized that global warming is the central issue of our time. I consider this to be perhaps the most significant article that we have published in all my years as Editor. For this issue I have slightly updated it to remove statements that are no longer needed. It is now an accepted fact that global temperatures are rising as a result of human activity.
INTRODUCTION
In far northern Siberia lies a massive subdivision called the Yamalo-Nenets, a permafrost region that extends well north of the Arctic Circle. The Nenets (which means “man” in the native language) are the nomadic inhabitants of the region, and “Yamal,” loosely translated, means the “end of the world.” The Nenets are sustained by the local reindeer population, estimated to be the largest herd in the world, and reindeer are sacred to the people of the region. From reindeer the people derive food, clothing, and tools, and they use the thick hides to form shelters. Nenet herders travel up to 1,000 km with the reindeer herds annually along ancient migration routes.
The climate in Yamalo-Nenets is brutal. Historically, winter temperatures reached –50°C, and summertime temperatures in the southern regions only briefly reached 15°C (59°F). However, Russia is warming at 2.5 times the rate of the world average. In July 2016 the Yamalo-Nenets region experienced a heat wave unprecedented in magnitude and duration. Temperatures reached a peak of 95°F, and they persisted above 80°F for many weeks. The result was a rapid thawing of many thousands of square miles of frozen tundra.
2
As decades-old reindeer carcasses thawed, microbes that had been frozen were released, and a disease that had not been seen in the region since 1941 was resurrected. What followed was a massive outbreak of reindeer anthrax, which killed an estimated 2,300 reindeer in only a few weeks, as affected animals died within only two to three days. The spore form of anthrax can survive indefinitely in frozen soil, and Bacillus anthracis was easily cultivated from newly thawed carcasses as well as the newly sickened animals.
A regional alarm was sounded when a 12-year-old Nenet boy died of anthrax, at least 90 more deer herders were sickened, and more than 20 were hospitalized. A state of emergency was declared, and the specter of Russian public health officials in yellow Hazmat garb and quarantine tents appeared in international news feeds. Hundreds of Nenets were evacuated. Veterinary teams restarted a massive anthrax immunization program for the regional herd, which had been halted over a decade earlier due to lack of reported disease. By late 2016, Russian officials considered culling 250,000 reindeer to try to halt the epidemic.
In the even further northern reaches of the Siberian tundra lies the town of Zashiversk, still under permafrost. There, 150 years ago, a massive outbreak of smallpox killed 40 percent of the region’s population. Could the frozen corpses in shallow wooden graves serve as a source for the future reappearance of smallpox, a disease officially declared eradicated in 1977?
3
To investigate this possibility, samples from frozen corpses in wooden graves from the 1840s were unearthed and examined. While fragments of the smallpox virus genome were recovered, to date no transmissible smallpox virus has been identified in frozen human remains.
4
These rare reports of so-called “zombie Infections,” admittedly hyperbolic, nonetheless highlight a stark reality: changing climate and infectious diseases have always been linked.
GLOBAL WARMING AND CLIMATE CHANGE
The knowledge that climatic conditions affect human illness is ancient. The Roman aristocracy took their summers at higher, cooler elevations in part to avoid seasonal outbreaks of malaria (“bad air”). The food processes of salting, smoking, and currying of meats began in temperate climates due to an understanding of the association between food spoilage and diarrheal disease.
The predicted changes in ambient temperature can affect both the geographic range of pathogens as well as the incidence and seasonal prevalence of disease. This holds true not only for the microbes themselves, but for the insect and animal vectors in the chain of transmission of zoonotic infections.
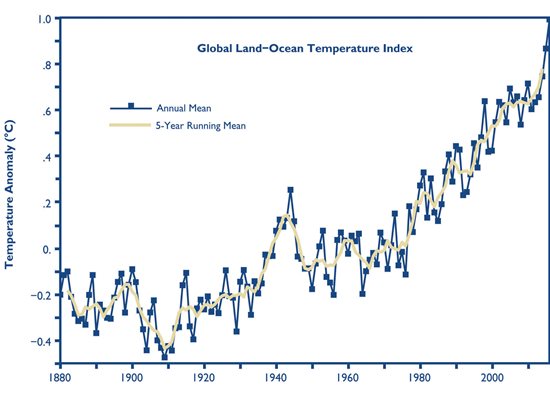
Fig. 1. Line plot of global mean land-ocean surface temperature index, 1880 to present, with the base period 1951-1980. The dark blue line is the annual mean and the gold line is the five-year running mean. [This is an update of Fig. 1A in Hansen et al. (2006).] The graph shows an overall longterm warming trend. (NASA Goddard Institute for Space Studies — http://data.giss.nasa.gov/gistemp/graphs/)
EXTREME WEATHER EVENTS: ENSO
One of the most significantly disruptive climate events caused by global warming is the perturbation in the El Niño Southern Oscillation (ENSO), which results in extreme weather events over a wide area. Climatic cycles of El Niño (sea surface temperatures in the eastern Pacific Ocean that are above average) and La Niña (below average sea surface temperatures in the central and eastern Pacific Ocean), strongly affect regional temperatures and rainfall. Variations in the amplitude, duration, and distribution of ENSO events can lead to major, sometimes massive and disruptive, heat wave-drought-flood cycles. More extreme variations in weather conditions, including severe storms as well as more frequent and non-seasonal hurricanes and typhoons, are consequences of global warming as well. The resulting effects on health and disease, especially in impoverished regions with poor water, sanitation, and health care infrastructure can be devastating.
5
INFECTIONS ASSOCIATED WITH EXTREME WEATHER EVENTS
Tropical storms and hurricanes in Central America and across the southern United States have increased substantially over the last 20 years, with attendant increases in weather-related deaths and massive socio-economic disruption. Increased rates of fecal-oral gastrointestinal infections, vector-borne illnesses, skin and soft tissue infections, and respiratory infections have all been associated with such disasters. Flood-related outbreaks of bacterial diseases that have been identified include typhoid fever, cholera, shigellosis, enteropathogenic E. coli, non-typhoidal salmonella, and leptospirosis. The risk of fecal-oral viral infections such as hepatitis A and E is also increased in association with rainy season floods. Parasitic diseases such as Giardia and Cryptosporidium are also consequences of the flooding that results from these extreme weather perturbations.
Further, displaced and crowded populations are also at risk for outbreaks of measles, meningococcal meningitis, influenza, and MRSA infection.
6 A detailed study in Peru compared health care data after a severe El Niño season with baseline data. For each 1°C increase in temperature, hospital admissions increased by 8 percent. Diarrheal disease admissions predominated, and increased by over 6,200 cases post-El Niño.
7
Even drought conditions can be associated with an increase in infectious diseases. Under arid conditions where water sources are scarce, mosquitoes and birds can be brought into proximity, facilitating transmission of West Nile virus to birds, and then to humans. In addition, the poor sanitation that can accompany drought conditions can facilitate transmission of enteric infections, as was demonstrated by a drought-related epidemic of cholera in Kenya in 2009.
8
CLIMATE CHANGE AND ZOONOTIC DISEASES
Changes in precipitation and ambient temperatures can directly affect the incidence and prevalence of vector-borne infections, through host-pathogen interactions as well as ecosystem changes. Rising temperatures can allow for the survival of pathogens in previously hostile environments. Ambient warming can also result in a shortened pathogen incubation period, and an increase in microbe density within the vector.
9 Increasing temperatures, humidity, rainfall, and flooding also favor vector breeding, while shortening their life cycle and expanding their habitat range.
Arthropod-borne burgeoning epidemics have been particularly facilitated by the unrelenting expansion of the range of
Aedes aegypti, the mosquito vector for multiple viral pathogens. In only the last few years its range has expanded from the Mexican border up to San Francisco on the west coast and Pennsylvania on the east coast.
10
Dengue and
chikungunya are arboviruses that produce acute febrile illnesses associated with severe musculoskeletal pain (Dengue is known by locals in endemic areas as “break bone fever”). About one third of the world’s population lives in dengue endemic areas, with over 400 million infections estimated to occur annually. The intercontinental spread of these diseases has in part been attributed to increased ambient temperatures and more prolonged and persistent rainy seasons.
Chikungunya virus, which had been endemic in Asia and Africa for decades, spread suddenly and dramatically from India to the Americas in late 2013, causing an explosive epidemic. It is now estimated to be responsible for 1.7 million cases in 45 countries. Though less lethal than dengue, its debilitating post-infectious musculoskeletal pain can last for months.
The alarming spread of
zika virus from South America into the United States, with devastating obstetrical and neonatal consequences, has also been associated with prolongation of the mosquito season.
About half of the world’s population lives in regions at risk for
malaria. The World Health Organization (WHO) estimated that 212 million cases of malaria with 429,000 deaths occurred in 2015. As ambient temperatures rise, the Plasmodium parasite replicates faster. This accelerated life cycle results in a higher infection burden in the vector mosquitoes, rendering their bite more infectious. Furthermore, the warmer temperatures also stimulate the infected mosquitoes to take blood meals more frequently. Global warming is expected to exacerbate the hyper-endemic nature of malaria in parts of the world.
11
The outbreak of hantavirus in the in the early 1990s in the four corners region of the Southwestern United States is another example of climate disruption leading to emergence of an infectious disease.
12 Heavy El Niño rains after years of drought resulted in an explosion of plant growth and a dramatic rise in the population of deer mice that carry the virus. Subsequent exposure of humans to mouse droppings resulted in the explosive 1993 outbreak of Hantavirus Pulmonary Syndrome. Hantavirus infections have now been reported in more than 30 states.
In 1999, after a similar sequence of heat wave, drought, and flood, the mosquito-borne African West Nile virus first arrived in North America. Beginning in New York City, where it killed nine people and infected hundreds, it spread rapidly in the immunologically naive U.S. population. The spectrum of illness ranged from asymptomatic infection, through self-limited aseptic meningitis, to devastating polio-like meningoencephalitis. More than 2,000 people have died of West Nile Virus infection, which remains endemic in the United States.
13
Mosquitoes are not the only insect vector impacted by climate change. Epidemics of tick-borne illnesses such as
Lyme disease have been facilitated by the milder winters of global warming. The ecology and epidemiology of human infection with
Borrelia burgdorferii is complex, and is related to the geographic range and density of Ixodes ticks, their host mammals, as well as their infection burden with Lyme spirochetes. Climate change has resulted in more favorable overwintering conditions and a resultant increase in survival of both the pathogen within infected ticks, as well as the white-tailed deer and deer mouse hosts involved in the life cycle.
14
The web of events leading to the 2014 Ebola outbreak in western Africa is a bit more complex, but here, too, climate change has played a role. Certainly, the progressive deforestation of the region over decades has caused displacement of many animal species from their preferred habitats and therefore an increased likelihood of contact with humans. The precipitous rise in human Ebola infections in 2014, however, followed a heat-drought-rain cycle that lead to an abundance of food such as fruit, bringing bat vectors in close proximity with primates. Infected primate “bush meat,” considered a food staple by local populations, served to transmit the deadly disease to humans.
15
CONCLUSIONS
Global warming has resulted in an unrelenting rise in the earth’s mean temperature, and is accelerating at an alarming rate. Warming of the earth has caused a disruption of normal global weather patterns resulting in a variety of extreme weather conditions. These phenomena have both direct and indirect effects on human infectious diseases.
While the problems outlined in this paper are indeed pervasive, the devastating consequences of global warming and extreme weather events go far beyond just infectious diseases. Famine, political uprisings, mass migrations, and socio-economic upheaval can also be consequences of climate change. It will be left to governments and nations to try and address, and hopefully begin to reverse, the coming global catastrophe.
In December 2015, the United States joined representatives of more than 190 countries in drafting the Paris Climate Agreement, which has been ratified by 125 parties as of this writing. The Agreement took effect on Nov. 4, 2016,
16 and called for mitigation of greenhouse gases to begin in 2020. Let us hope that we do not have to face the consequences of its failure. (Note: President Trump withdrew from the agreement, but President Biden rejoined it.)
REFERENCES
1. Kontra JM. Zombie infections and other infectious disease complications of global warming.
J Lanc Gen Hosp. 2017; 12 (1): 12-16.
2. Bearak M. Anthrax spreads from reindeer to humans in an outbreak at the end of the world.
The Washington Post. August 2, 2016.
3. Biagini P, Thèves C, Balaresque P, et al. Variola Virus in a 300-year-old Siberian Mummy.
N Engl J Med 2012; 367:2057-2059.
4. http://siberiantimes.com/science/opinion/features/f0179-how-great-is-the-threat-of-an-explosion-of-smallpox-from-the-thawing-permafrost-in-siberia/">http://siberiantimes.com/science/opinion/features/f0179-how-great-is-the-threat-of-an-explosion-of-smallpox-from-the-thawing-permafrost-in-siberia/
5. Hales S. et al WHO Climate change and human health. Chapter 5. Impacts on health of climate extremes. Pp. 79-102
6. Watson JT, Gayer M, Connolly MA. Epidemics after natural disasters.
Emerg Infect Dis. 2007;13(1):1.
https://dx.doi.org/10.3201/eid1301.060779
7. Checkley W el at. Effect of En Nino and ambient temperature on hospital admissions for diarrhoeal diseases in Peruvian children.
Lancet. 2000; 355(9202): 442-450
8. Shuman EK. Global climate change and infectious diseases.
N Engl J. Med. 2010. 362(12): 1061-1063
9. Mills JN, Gage KL, Kahn AS. Potential influence of climate change on vector-borne and zoonotic diseases.
Environ Health Perspect. 2010; Nov;118(11): 1507–1514. doi: 10.1289/ehp.0901389
10.//https://www.cdc.gov/zika/vector/range.html"> https://www.cdc.gov/zika/vector/range.html
11. Gagnon, AS, Smoyer-Tomic KE, Bush ABG. et al. El Nino southern oscillation and malaria epidemics in South America.
Int J Biometeorol. 2002; 46(2): 81-89. doi: 10.1007/s00484-001-0119-6.
12. Update: Hantavirus Pulmonary Syndrome.
MMWR 1999; 48(24): 521-525
13. West Nile Virus and other nationally notifiable arboviral diseases – United States, 2014.
MMWR 2015:64(34); 929-934
14. Brownstein JS, Holford TR, Fish D. Effect of climate change on Lyme Disease risk in North America.
EcoHealth. 2005: 2(1); 38-46.
15. Origins of the 2014 Ebola Epidemic. World Health Organization International.
http://who.int/csr/disease/ebola/one-year-report/virus-origin/en/
16. United Nations. Framework Convention on Climate Change
http://unfccc.int/paris_agreement/items/9485.php