
Spring 2021 - Vol. 16, No. 1
History of Diabetes Diagnosis and Treatment
in Lancaster County
Jocelyn M. Dialectos
The Lancaster Medical Heritage Museum
The incidence of diabetes in the United States has been trending upward for some time, and Lancaster is no exception. This paper traces the transformation of diagnostic approaches and treatment of diabetes in Lancaster County since the first settlement of this area, and tracks local advances against the general progress in our understanding and management of the disease.
THE HISTORY OF RESEARCH ON DIABETES
Though the history of diabetes in the 20th century is well known, beginning with the isolation of insulin by Canadians Frederick Banting and Charles Best in 1921, earlier studies, though less familiar, are no less interesting.
The ancient Greeks carried out some of the first diabetes experiments after noticing that frequent urination was a common complaint among afflicted patients. Early Greek doctors suggested horseback riding to reduce urinary urgency by causing friction on the bladder, and also studied diets of wine, potatoes, and oatmeal. Overfeeding was commonly used to compensate for the rapid weight loss seen in diabetic patients, though some doctors preferred starvation diets.
1
The sweet taste of diabetic urine was not explained until around 1775, when Matthew Dobson demonstrated sugar in diabetic urine by boiling a sample until the liquid evaporated, leaving a sweet crystalline precipitate with both the appearance and taste of sugar.
2,3 His treatment plan consisted of purgatives (rhubarb and senna), opium (Dover’s powder), and urinary irritants (cantharides from the Spanish fly, a beetle). Though Dobson also prescribed the consumption of water from the Buxton Spa at Derbyshire, England, none of his patients followed his suggestion.
4
During the early 19th century, the pancreas was suspected of playing a role in diabetes because pancreatic tissue from diabetic cadavers was often atrophied and filled with stones. Nonetheless, the pancreas was already known to be an exocrine organ, so the atrophied tissue was considered a chance finding.
 In the early 1800s French physiologist
In the early 1800s French physiologist
Claude Bernard studied glucose
metabolism and tried to determine
which organ causes diabetes.
In this climate of confusion, famed French physiologist Claude Bernard studied glucose metabolism to determine which organ causes diabetes. He first suspected the lungs, so he studied the pulmonary circulation by simultaneously injecting grape sugar into the jugular vein and extracting blood from the carotid artery. After demonstrating that glucose was not metabolized in the lungs, Bernard began studying liver function in dogs.
He fed one group of dogs a diet rich in carbohydrates, and fed others a meat diet. The dogs were sacrificed after eating their meals, and their livers were examined for the presence of sugar. Bernard found that both groups had greater amounts of glucose in their livers than in other organs, and he realized that the liver stores glucose in a different form, which he called
“la matière glycogène,” or “sugar-forming substance.” Because it could be converted back to sugar and released into the blood, Bernard mistakenly concluded that diabetes resulted from the over-production of glucose by these glycogen stores.
Though we now know that the brain has a complex role in regulating glucose metabolism through specialized neurons in the hypothalamus that sense insulin, leptin, glucose, and fatty acids, Bernard was the first to discover a link between the brain and diabetes. He punctured the fourth ventricle of rabbit brains with a needle, and induced temporary symptoms of diabetes.
2



Joseph von Mering Oskar Minkowski Frederick Banting Charles Best
In 1886, Joseph von Mering found that phlorizin, a naturally occurring phenol glycoside first isolated from the bark of an apple tree, induced glycosuria. This discovery led him to partner with Oscar Minkowski three years later at the University of Strasbourg to perform pancreatectomies on 4 dogs, all of whom developed severe polyuria and glycosuria. Based on these findings, Minkowski injected samples of the pancreas back into the dogs subcutaneously, and observed that the glycosuria was temporarily reversed until the implanted pancreas was removed or degraded. These experiments revealed the role of the pancreas in controlling glucose levels, suggesting this organ was part of the endocrine system and diabetes is a disease of the pancreas.
2
As is well known, Banting and Best first isolated insulin in 1921 at the University of Toronto under the supervision of John Macleod. To determine the relationship between the pancre-as and glucose homeostasis, they surgically removed the pancreas from a dog, crushed the pan-creatic tissue and mixed it with salt, then injected the mixture back into the dog, resulting in a significant reduction in the dog’s blood sugar. Hoping to isolate the extract responsible for this finding, James Collip joined the team to assist in the purification process. The resultant substance originally was termed “insletin,” though Macleod later changed the name to “insulin.” Macleod and Banting won the Nobel Prize for their discovery in 1923, and they decided to share their monetary compensation with Best and Collip.
2
The first person in the world to receive insulin therapy in 1922 was Leonard Thompson, a 14-year old diabetic undergoing Frederick Allen’s starvation diet, in which he was fed minimally and brought to emaciation. Thompson initially was given a 15 mL insulin shot in his buttock, but this procedure worsened his condition by triggering abscess formation around the injection site. Six weeks later he was given an updated form of insulin, with a substantial reduction in his dia-betic symptoms, a drop in his blood sugar from 520 mg/dl to 120 mg/dl, and the elimination of ketones from his urine. He lived for 13 more years after starting insulin therapy, a feat that was not possible with previous treatments.
2
Having tried the starvation diet with little success, Elizabeth Hughes Gossett also started insulin injections in 1922. Gossett had been diagnosed with diabetes when she was 11 years old, and insulin dramatically prolonged her life. She attended college and raised a family before her death in 1981.
2
DIABETES IN LANCASTER COUNTY
DIAGNOSIS
In the 17th century, according to folklore tradition, walking across
Agrostis stolonifera, the hungry grass, was a cause of diabetes. A diagnosis could be made if symptoms appeared after a person came in contact with the grass.
5 Though this diagnostic tactic was short-lived, many early methods of diagnosing diabetes used similar approaches based on the recognition of characteristic symptoms.
In the late 18th Century, the Atlee family, recognized for their prominence in the Lancas-ter community, mentioned in their correspondence the “preternatural flow of urine,” or frequent urination, as a primary means of diagnosing diabetes.
6
TREATMENT
The 17th Century
Up until the 1700s, treatment of diabetes locally focused mainly on Indian folk medicine and natural home remedies.
7 Throughout the 17th century, standard treatments included consumption of powdered mice, peanuts, chickweed, comfrey, wormwood, and boiled nettles. Some doctors also treated patients by infusing them with herb-Robert, dandelion, queen of the meadow, devil’s shoestring, sagebrush, yarrow blossom, horsetail grass, Spanish moss, or bugleweed extracts. Additionally, patients were instructed to drink goat’s milk, buttermilk, sauerkraut juice, vinegar, honey, and tea made from alfalfa or mullein leaves. Mixtures of sulphur and molasses and of salt and soda were prescribed, as well, and some patients were told to drink their own urine.
5 Common folk remedies also included Helmbold’s buchu,
8 French lilac,
9 huckleberry, sumac leaves, and devil’s club root. Substituting white sugar with brown sugar was widely believed to both treat and prevent diabetes. Letting a poisonous snake bite the patient was a less common recommendation.
5
The 18th Century
In this era, treatment of diabetes was still almost completely ineffective. The Atlee family’s letters from 1794 describe diabetic ulcers being treated by infusing the wounds with nicotine and tobacco solutions.
16 In 1799, John Rollo’s book,
An Account of Two Cases of the Diabetes Mellitus, began circulating in Philadelphia and provided novel suggestions on the diagnosis and treatment of diabetes that became popular.
10 He hypothesized that sugar was created in the stomach from vegetables, and his treatment stressed eliminating green vegetables from the diet. Animal foods were encouraged, and a typical diet could include lime water, milk, bread, blood pudding, and meat. Daily drinks of kali sulphuricum (potassium sulphate, which is still marketed today as a homeopathic treatment for colds) also were recommended.
Unlike previous diets, which solely reflected the humoral theory of medicine, Rollo’s treatment focused on preventing the body’s production of sugar. He pioneered the use of a low-carbohydrate, high-fat, high-protein diet, inspiring the use of meat diets throughout the next century. Rollo promoted strict adherence to this diet, but he noted that most patients opted for medicinal treatments over lifestyle restrictions, even when the medications caused side effects and tasted unpleasant.
4
Aside from the diet, 20 drops of antimonial wine (an emetic) and 25 drops of opium could be taken before bed. These doses were gradually increased as the treatment continued, and tobacco and foxglove could be added. To further manage symptoms, patients were instructed to apply hog’s lard to their skin and cover their bodies with flannel.
Rollo’s lack of scientific understanding of diabetes is revealed by his promotion of the ingestion of aloe, soap, rhubarb, colocynth, senna, castor oil, croton oil, and magnesium sulfate, all of which were meant to clear the bowels. Surgical interventions could be performed for severe cases, in which a large incision was made above each kidney to relieve congestion in the area and decrease bodily inflammation. Additionally, Rollo believed exercise exacerbated diabetes, and he endorsed only light activity, though rest was preferred. Uniquely, however, Rollo did not believe bloodletting was effective, and his book was one of the first treatment plans with no chapter on this practice.
4
The 19th Century
In 1800, Dr. John Howard introduced Chinese herbs and roots to Lancaster, bringing them directly from China, and creating the medicines himself. Like Rollo, Howard did not practice bloodletting.
11
With the turn of the century came a novel blend of medical and spiritual treatments. Pow-wow, a practice of folk healing rituals, became popular, and diabetes was approached with a mixture of amulets, spirituality, the Bible, magic, and herbs.
12
B. Ehrmen introduced homeopathy in the 1840s,
12 and Dr. Edwin Augustus Atlee used lithiated hydrangea. Certain diets were stressed, and some practitioners used a rigid milk diet.
13
The
Lancaster Examiner and Herald newspaper advertised diverse diabetes treatments, all of which claimed to be the only known remedy for the disease. One advertisement from 1864 recommended constitution water for diabetes and any other malady. A single bottle was required, taken as one teaspoon daily until the bottle was empty. Testimonials from satisfied customers claimed that this remedy began working within days to decrease urinary frequency. The ad asserted that constitution water was approved by the best doctors in Lancaster County, was “not merely mineral water,“ and should
not be met with skepticism.”
14
Other newspaper advertisements advocated avoiding starchy diets, which suggests that though the cause of diabetes was still unknown, doctors were aware the underlying problem involved the starch-sugar conversion process.
14 A related suggestion was to limit food consumption in general, since overeating was thought to cause diabetes and constipation was believed to induce diabetic comas.
15
Warner’s Safe Liver and Kidney Cure, a vegetable preparation, was promoted as a cure that had support from local doctors, as was a more specific diabetes treatment, Warner’s Safe Diabetes Cure. Both drugs could be found at any pharmacy. The Warner company was so convinced of this treatment’s effectiveness that a $1,000 reward was offered to any unsatisfied customer.
16
Because of the hyperglycemic polyuria seen in diabetics, an association between diabetes and the kidney was presumed, and there were both external and internal approaches based on this misunderstanding. Day’s Kidney Pads could be worn externally and cost $2 each. Though useless, they did no harm except to the pocketbook.
17 The internal approach involved the ingestion of kidney wort, a dried plant solution that was swallowed in conjunction with other medications. Its marketers believed diabetes developed when the blood became contaminated with humors that should have been excreted, and kidney wort aimed to restore the natural flow of bodily processes.
18
A variety of other substances were used with differing objectives, from reducing inflammation to cleansing the gastrointestinal tract.
15 Aside from opium and morphine, the list of non-narcotic medications that became standards of care in the late 19th century included antipyrine, ergot (for mild cases only), bromide of arsenic, iodoform, jambul (Syzygium jambolanum seed), oxygen inhalation, and alkali compounds (including sodium phosphate, nitrate of uranium, salicylic acid, picric acid, Calabar bean, potassium iodide, iodine tincture, lactic acid, cod liver oil, belladonna, valerian, and phosphorus).
Many other treatments from this time period centered on resolving individual symptoms, rather than curing the disease in its entirety. Ulcers were treated by tying the root of the ironweed plant around a patient’s neck,
19 and applying homemade pastes to the afflicted area. Creams could be made of either silver nitrate, which came in wax-covered sticks to prevent oxidation, or potassium permanganate crystals, which were dissolved in water to form a spreadable solution.
20 Similar remedies existed to combat the symptom of frequent urination. To encourage a healthier bathroom schedule, the bladder of a pig was burned to a powder and subsequently ingested.
19
The 20th Century
After the discovery of insulin, diabetes treatment shifted towards enhancing insulin formulas and developing potentially curative therapies. The following timeline depicts the introduc-tion of these major innovations in insulin therapy:
• 1930s: protamine zinc insulin, a long-lasting and stable formula is developed;
• 1940s: neutral protamine Hagedorn (NPH) insulin is one of the first intermediate-acting insulins;
• 1950s: Lente insulin is another intermediate-acting insulin;
• 1955: the chemical structure of insulin is determined by Fred Sanger;
• 1967: proinsulin is discovered by Donald Steiner, who creates a C-peptide radioimmunoassay to measure insulin production in the body;
• 1967: the first pancreatic transplant surgery is performed by William Kelly and Richard Lillehei;
• 1972: U100 insulin enables more accurate dosing;
• 1982: recombinant insulin becomes commercially available;
• 1990s: insulin pens gain popularity;
• 1996: short-acting insulin analogs are developed;
• 2001: long-acting insulin analogs are introduced.
Evidence-based diabetes diets began to emerge throughout the 20th century. In 1987, the
Lancaster Farming newspaper carried an advertisement that detailed different recipes and diets for diabetics created and approved by the Lancaster chapter of the American Diabetes Association.
21
Chelation therapy gained some popularity in the late 1900s. The same
Lancaster Farming newspaper included an advertisement for chelation in 1993, which detailed the various formulas that were available and presented testimonials from both doctors and patients. Formula 1, the first suggested chelating agent, was believed to cure diabetic foot ulcers and prevent the threat of amputation without inducing side effects.
22
Amish Remedies
Lancaster’s Amish population has their own folk remedies for diabetes. Many different teas are thought to cure diabetes symptoms, including those made with leaves from the plants of avocados, eucalyptus, walnuts, peaches, blueberries, and strawberries.
23 Additional teas are made with
pau d’arco bark, tansy, chia seeds,
23 clover blossoms, and dandelions.
24 According to Amish testimonials, some diabetics no longer required insulin while drinking these teas. Herbs such as cedar berries, uva ursi, licorice root, mullein, cayenne, and golden seal root are also common remedies. Dried calamus root is chewed to alleviate dry mouth,
23and leg ulcers are cared for by applying a mixture of powdered sugar, lanolin, and benzoin solution to the affected area. This paste is applied in an upward motion to encourage proper circulation. Many Amish treatments also recommend the intake of chromium picolinate, carnitine, vitamin B-6, vitamin E, zinc, inositol, ginseng, and fenugreek supplements. Artichokes, kelp, oatmeal, dried beans, yellow dock, burdock, black snake root, sassafras, and wine are encouraged as well.
Prominent Lancastrians in the History of Diabetes
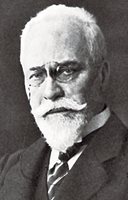
Dr. David Hayes Agnew was a 19th century Lancaster physician who was diabetic. He specialized in abdominal, gynecological, orthopedic, and brain operations, and he lectured students in those areas. In addition to his role in founding the state medical licensing board, Agnew also helped to organize the Lancaster City and County Medical Society in 1844.
12
 Charles Demuth
Charles Demuth
Charles Demuth, the famous local artist, became one of the first Americans to receive in-sulin — in 1923. Prior to that, he had been diagnosed with diabetes in 1920 after several years of ill health. He reportedly started developing carbuncles and craving sweet foods, but he continued to paint and take trips to Philadelphia and New York, and the protracted course of his disease suggests that he produced some residual intrinsic insulin for many years. Eventually, his attacks became so severe that he was put on Dr. Frederick Allen’s starvation diet, was fed only coffee, and was forced to rest all day. His friend Blanche Steinman worried that this treatment was bringing him close to death.
At an emaciated 90 pounds, he was depressed, and despite his worsening condition,
25 in the fall of 1921 he decided to vacation in Paris. He was admitted to the American Hospital of Paris in Neuilly-sure-Seine for a week, though this hospitalization did not improve him. He mentioned in one of his letters that his fatigue prevented him from accepting an invitation from his friend Arnold Rönnebeck to visit Germany. At one point during his stay in Paris, Demuth tired so easily that he was not able to carry bread back to his hotel room. When he returned from Paris in 1922, he was seen by Dr. William Carlos Williams, who then referred Demuth to Allen’s Physiatric Sanitorium in Morristown, N.J. Again, he was put on a minimal-calorie diet, causing him to “fade to mere bones.”
The Morristown Institute was the first facility in the United States to administer insulin therapy, and Demuth was the second person in this institution to receive those insulin treatments. Upon beginning his insulin injections in 1923,
25 Demuth instantly started gaining weight and becoming healthier, but the imperfections of this novel treatment caused new problems as Demuth had trouble adjusting to his altered diet and remembering his injection routine. Finding the correct insulin balance was challenging, and he still suffered hypoglycemic episodes. When he collapsed, his friends had to force feed him sugar cubes, as he never wanted to consume them voluntarily.
Demuth continued his diet and insulin therapy until his death in 1935.
25 He had planned to return to Paris around this time, but his health already had begun to deteriorate. While his doctors were unsure exactly why his condition worsened, Williams believed Demuth’s carelessness about his insulin injections was the underlying cause. After the death of his mother, who cleaned his syringes and ensured he complied with his treatment, Demuth stopped caring about his injections, sometimes even refusing to take them. He most likely entered a diabetic coma due to extreme hypoglycemia or hyperglycemia.
25
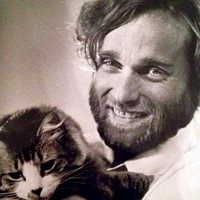 David Brumbach
David Brumbach
David Brumbach is a more recent local artist who achieved considerable recognition and also suffered from diabetes. He created most of his artwork in the 1970s and 1980s, when he became famous for his photorealism technique primarily in watercolor. Brumbach struggled with his diagnosis throughout his life, though he died of a brain tumor in 1992.
26
CONCLUSIONS
Lancaster has a history of diabetes management based on folk and natural remedies that had a particular character because of this community’s specific ethnic roots. The progression to state-of-the-art medications and technologies parallels general scientific progress in the field.
The rising rates of type 2 diabetes in Lancaster County are doubtless related to the problem of obesity, which has become a national problem that has not spared our community.
A particularly interesting aspect of diabetes in Lancaster is it affliction of the two most prominent artists our community has produced. Charles Demuth and David Brumbach each managed to produce a significant body of work despite severe diabetes. In Demuth’s case it is even more remarkable because he achieved international recognition despite having initially de-veloped diabetes before insulin had become available. Sadly, both he and Brumbach were haphazard in managing their diabetes and eventually died with advanced complications of their disease, though Brumbach’s death was hastened by cancer.
ACKNOWLEDGMENTS
The author wishes to thank Drs. Charles Rost and Nikitas Zervanos, as well Hannah Lerew, executive director of the Lancaster Medical Heritage Museum, for their assistance in the preparation of this manuscript.
REFERENCES
1. Das AK, Shah S. History of diabetes: from ants to analogs.
J Assoc Phys India. 2011; 59(Suppl): 6-7.
2. Karamanou M, Protogerou A, Tsoucalas G, et al. Milestones in the history of diabetes mellitus: The main contributors.
World Journal of Diabetes.2016; 7(1):1.
3. Dobson M. Experiments and observation on the urine in diabetes.
Med. Obs. Inq.1776; 5: 298-316.
4. Tattersall R.
Diabetes: the biography. Oxford University Press. 2009.
5. Hatfield, G. (2004).
Encyclopedia of folk medicine: old world and new world traditions. ABC-CLIO.
6. Champneys, B. (1794, January 21). [Medical Notes on Various Diseases]. Atlee Family Collection (MG-22, Box 2, Folder 17). LancasterHistory.org, Lancaster, PA.
7. Lancaster Medicine (Vol. 52). (1976). Lancaster, PA: Lancaster City & County Medical Society.
8. Helmbold’s Preparation. [Advertisement]. (1870, October 8).
The Daily Evening Telegraph.
9. Hurley, D. (2010).
Diabetes Rising: How a Rare Disease Became a Modern Pandemic, and What to Do About It. New York, NY: Kaplan Publishing.
10. Joseph and James Crukshank. (1799, March 25). [Advertisement for John Rollo’s book].
Gazette of the United States, & Philadelphia daily advertiser.
11. Chinese Doctor, Dr. John Howard. [Advertisement]. (1800, June 28).
The Lancaster Journal.
12. Lancaster Medicine (Vol. 52). (1976). Lancaster, PA: Lancaster City & County Medical Society.
13. Renal Derangements: Treatment of Diabetes Mellitus. (1899). St. Louis, MO: Lambert Pharmacal Co.
14. [Advertisement for Mineral Water]. (1864, February 10).
Lancaster Examiner and Herald.
15. Purdy, C. W. (1890).
Diabetes: Its Causes, Symptoms, and Treatment. Philadelphia, PA: F. A. Davis.
16. [Advertisement for Warner’s Safe Liver and Kidney Cure]. (1880, March 26).
Lancaster Daily Intelligencer.
17. [Advertisement for Day’s Kidney Pads]. (1880, March 26).
Lancaster Daily Intelligencer.
18. [Advertisement for Kidney Wort]. (1880, March 26).
Lancaster Daily Intelligencer.
19. Hohman, J. G. (1877).
The Long Lost Friend, Containing Mysterious and Invaluable Arts and Remedies for Man As Well As Animals, With Many Proofs of Their Virtue and Efficacy in Healing Diseases, &c. Lancaster, PA: Printed for the Purchaser.
20. Lahr, J. W., MD. (2017).
Hale Columbia: Columbia, Pa., Medical Record, 1893-1905: A True & Complete Study of Infectious Disease & Medicine In a small Pennsylvania Town At the Turn of the Century. Hummelstown, PA: Joseph Lahr.
21. Recipes for Diabetes [Advertisement]. (1987, March 7).
Lancaster Farming.
22. Chelation Therapy [Advertisement]. (1993, February 6).
Lancaster Farming.
23. McGrath, W. R. (1985).
Amish Folk Remedies for Plain and Fancy Ailments. Freeport, OH: William McGrath.
24. Quillin, P. (1995).
Amish Folk Medicine. North Canton, OH: The Leader Co.
25. Farnham, E. (1960).
Charles Demuth: His Life, Psychology and Works (Doctoral dissertation, The Ohio State University).
26. h
ttps://lancasteronline.com/news/friends-family-recall-late-artist/article_04477418-8959-569c-80e1-2e6a579e411a.html#:~:text=A%20Lititz%20native%2C%20David%20Brumbach,less%20than%20a%20week%20before.