
Spring 2020 - Vol. 15, No. 1
Progress in Thoracic Surgery:
Its Effect on Clinical Pracice and Residency Training
David J. Cziperle, MD, FACS
Clinical Associate in Surgery
University of Pennsylvania School of Medicine
Managing Physician, Thoracic Surgery
Penn Medicine LG Health Physicians Thoracic Surgery
INTRODUCTION
Thoracic surgery has a documented history of advances made by many brave surgeons who were not afraid of failure. They were risk takers who utilized the basics of anatomy and physiology to solve the problems of their particular era. The modern thoracic surgeon stands on the shoulders of these predecessors and recognizes that their successes and failures are the basis of our future. The purpose of this manuscript is to recount some of the great moments in thoracic surgery, to highlight recent advances, and to prophesize – as much as possible – what still needs to be accomplished.
According to Genesis (2:21-22), the first thoracic surgical procedure was performed by God…a rib resection. “And the Lord God caused a deep sleep to fall upon Adam, and he slept: and he took one of his ribs, and closed up the flesh instead thereof: And the rib, the Lord God had taken from man, made he a woman, and brought her unto the man.”
Subsequently, the Greeks recognized the mortality associated with chest trauma, particularly penetrating wounds. During the battle of Mantinea in 362 B.C., Epaminodas was pierced in the chest by Anticrates’ javelin. He wisely did not remove the javelin until after victory was attained so that he could die after seeing his work accomplished. Epaminodas died of a pneumothorax and is often credited as being the “Savior of Greece.” 1
TUBERCULOSIS
Notwithstanding the Biblical and Greek references cited above, thoracic surgery was not practiced as a scientific discipline until the early 19th century when tuberculosis became prevalent, reaching epidemic proportions in the early 20th century. During an approximately 50-year interval, the treatment of tuberculosis transitioned through three stages.
The first stage involved sequestration of tuberculosis patients in sanatoriums away from urban populations. It is notable that early in this sanatorium era, surgical treatment of tuberculosis was initiated by medical doctors who performed minor procedures in an attempt to improve the disease process. Forlanini in Italy introduced pneumothorax; Jacobaeus in Stockholm developed pleuroscopy and adhesiolyis; and De Cerenville of Switzerland performed the first rib resection to initiate collapse therapy for tuberculosis. All of these pioneers were professors of internal medicine, not surgeons.
The second phase of tuberculosis treatment began with itinerant traveling surgeons who visited the sanatoriums to perform procedures, since tuberculosis patients were still not welcomed at urban hospitals. During this phase, without modern anesthesia, the field of thoracic surgery still managed to develop the use of thoracoplasty – to collapse diseased lung tissue – and drainage of empyema. Most of these procedures were accomplished under local anesthesia so that the awake patient could cough and expectorate secretions, thus avoiding contamination of the contralateral good lung. 2
In the next era, with general anesthesia, Richard Overholt, who received his training at the University of Pennsylvania prior to becoming a world renowned thoracic surgeon and establishing a thoracic clinic in Boston, pioneered the face down or prone position for pulmonary resection to prevent contamination of the contralateral lung. Later, that approach was superseded by the development of endotracheal intubation with selective bronchial cannulation and ventilation.2
The third stage of tuberculosis treatment was the introduction of drug therapy, which began with Streptomycin in 1944. In the next 50 years, a strong bond developed between pulmonologists and thoracic surgeons to combine medical and surgical treatment in the management of what had become an epidemic problem.
THORACIC SURGERY AFTER THE TUBERCULOSIS ERA
As tuberculosis came under control, thoracic surgeons performed less surgery for tuberculosis, but the techniques they had learned became steppingstones to surgical techniques for other intrathoracic procedures.
An example is progress in lung resection. During the surgical tuberculosis era, pulmonary resection had occasionally been performed in an attempt to effect a cure. In 1891, the French surgeon Théodore Tuffier performed the first successful resection of the apex of the lung for tuberculosis.3 Most other attempts at performing surgical resection of the lung were disastrous, as they were done with mass ligation of the pulmonary hilum. In 1933, Evarts Graham performed the first successful pneumonectomy with individual ligation of the major pulmonary vessels and the bronchus, but then reportedly lost the next 19 patients before again achieving a successful outcome.2
During the latter part of the 20th century, anesthetic techniques improved, and single lung ventilation allowed surgeons to operate on an uninflated lung in an anaesthetized and sedated patient. Thoracic surgical procedures were now accomplished through large, painful incisions, often accompanied by additional rib resections. Intraoperative techniques remained crude by modern day standards, as there were no stapling devices, and everything was hand sewn and ligated. For many procedures, intraoperative mortality was high, and postoperative complications were abundant, often including excessive bleeding, prolonged air leaks, and dehiscence of the bronchial closure with subsequent empyema. Additional complications included postoperative pneumonia and pulmonary embolism, as early ambulation and prophylaxis of deep vein thrombosis were not practiced.
Simultaneously, the field of cardiac surgery was born. In 1953, after 20 years of research, Dr. John Gibbon performed the first operation with cardiopulmonary bypass, closure of an atrial septal defect, at Jefferson Medical College in Philadelphia.
CHANGES IN TRAINING REFLECT CHANGES IN PRACTICE
Thoracic surgeons adopted the new surgical discipline of cardiac surgery as their natural purview. On January 1, 1971, the Board of Thoracic Surgery became a primary specialty board distinct from general surgery, changed its name to the American Board of Thoracic Surgery (ABTS), and became a member of the American Board of Medical Specialties.4 During the ensuing decades, training in thoracic surgery residencies encompassed all intrathoracic procedures. To be eligible for examination by the ABTS, candidates had to perform a minimum number of specific cardiovascular, pulmonary, and esophageal operations.
Meanwhile, as techniques and technology advanced across all specialties, a plethora of new procedures was introduced, such as transcatheter aortic valve replacement (TAVR), long-term ventricular assist, robotic lobectomy, and minimally invasive esophagectomy. Thoracic surgeons could not all be expected to master every one of these techniques and utilize them on a regular basis, and there was an inevitable tendency for CT surgeons to focus their practices on one or two areas of interest. Unsurprisingly, specialization improved outcomes.
As the practice of CT surgery became more complex and diverse, questions were raised about the adequacy of the traditional CT training plan, which consisted of five years in a U.S. or Canadian general surgery residency, followed by two years in a CT surgery residency. It became increasingly clear that to master the entire clinical specialty, more than two years of CT training might be needed. Moreover, to provide research experience during training for budding academic surgeons, the seven-year minimum often became even longer. As a result, many leading thoracic surgery residencies effectively lasted three to five years after general surgery training, a duration that discouraged entry into the field.
To shorten the total length of training, while hopefully enhancing education in CT surgery by increasing the time devoted to that discipline, from 1971-77 the ABTS approved several experimental programs that eliminated the year of chief residency in general surgery and combined training in general and thoracic surgery. Though these “special programs” were eventually eliminated, they were harbingers of what was to come.5 In 2003 the ABTS permanently eliminated the requirement for ABTS candidates to have previously received certification by the American Board of Surgery (which requires a year spent as chief resident in general surgery). That action allowed restructured residencies to combine general and thoracic surgery training into a total of six or seven years that resulted in certification solely by the ABTS.
The seven-year programs simply shorten general surgery from five years to four years, and add that year to CT surgery. In the six-year residency programs, general and CT surgery training are “integrated.” To fulfill the required 24 months of residency training in thoracic and cardiovascular surgery, the programs generally contain intermittent periods of general and CT surgery, with progressively increasing responsibility distributed through the six-year residency. Regardless of the particulars, the ABTS requires that the program must culminate in “continuous [CT surgery] senior-level responsibility in the last year of training.” 6
Two Pathways
Having addressed the need to make CT surgery training more efficient, the ABTS dealt with the increasing tendency of CT surgeons to specialize in cardiovascular (CV) or general thoracic surgery. Some training programs began to allow residents to maximize their exposure to one or the other. Ultimately, the ABTS approved two pathways to certification, one in CV surgery and one in general thoracic surgery.
Although both certifications require applicants to perform a minimum number of “major cardiothoracic cases,” (an average of 125/year), the case distribution differs substantially, and emphasizes either thoracic or CV surgery. The ABTS emphasizes that its most important goal is “to maintain adequate educational and operative experience in both general thoracic and cardiovascular surgery, irrespective of the field of thoracic surgery in which a candidate may choose to practice.” 6
It is important to recognize that this reorientation of training places burdens not only on the trainee, who must choose which pathway to pursue, but also on the training program that must commit resources and administer two different pathways of training.
CHANGES IN PRACTICE REFLECT CHANGES IN TRAINING
Similar to the changes in the approved CT Surgery training pathways, our clinical practice of thoracic surgery has also evolved, and we have become more specialty focused in either general thoracic surgery or cardiovascular surgery.
In 2015, the thoracic and cardiovascular surgeons at Lancaster General Hospital divided into separate entities to allow for more defined and specialty-specific delivery of care. Cardiothoracic Surgeons of Lancaster (CTSL) continues to provide expertise in all aspects of cardiovascular surgery as they have done exclusively since the first open-heart operation at Lancaster General Hospital in September 1983. Thoracic surgeons at Penn Medicine Lancaster General Health perform non-cardiac thoracic surgery procedures and have achieved a wealth of experience and expertise in minimally invasive thoracoscopic and robotic surgery techniques.
The field of minimally invasive major thoracic procedures has evolved tremendously during the past decade. The learning curve has been steep, but certainly not as steep as the development and perfection of lung resection since the first pneumonectomy performed by Evarts Graham and others cited earlier. The benefits of minimally invasive thoracic surgery include better patient satisfaction, shorter lengths of stay, fewer complications and readmissions, and shorter recovery times.
Initially, minimally invasive thoracic surgery procedures were performed with video-assisted thoracoscopy (VATs), but the addition of robotic-assisted thoracoscopy (RAT) has further advanced the capabilities of minimally invasive thoracic surgery.
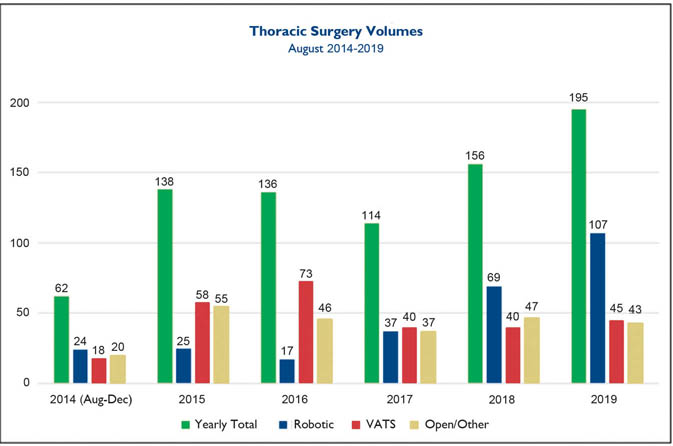
Fig. 1. Thoracic surgical volume over the past five years at Lancaster General Hospital subdivided into open technique, video-assisted thoracoscopic technique (VATS), and robotic-assisted thoracoscopic technique.
The thoracic surgery team at Penn Medicine Lancaster General Hospital now performs the majority of our thoracic procedures utilizing robotic-assisted thoracoscopic techniques. During the past five years, 801 thoracic surgery procedures have been performed at Lancaster General Hospital. Fig. 1 displays our commitment to the minimally invasive robotic-assisted thoracoscopic approach, which has become our preferred approach in the past one to two years.
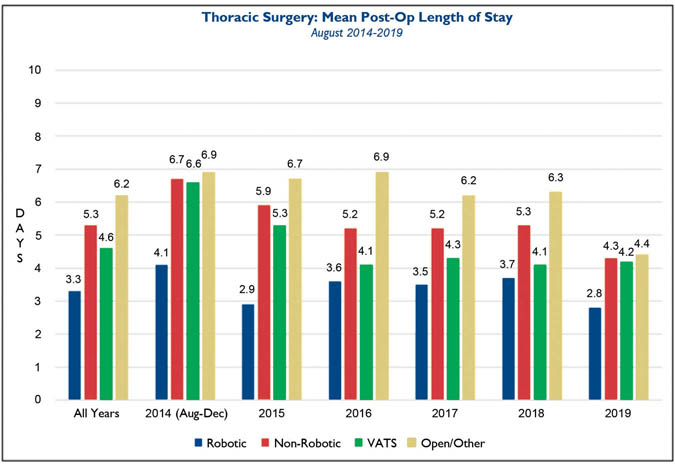
Fig. 2. Average length of stay for patients operated on by robotic-assisted thoracoscopic technique compared to the averages for the non-robotic techniques (open or video-assisted), displayed combined and individually.
Fig. 2 demonstrates the LGH length of stay (LOS) for open, robotic-assisted thoracoscopic, and VATs procedures during the past five years. LOS for robotic-assisted thoracoscopic procedures is an average of 1.3 days shorter when compared to the VATs group of patients, and 2.9 days shorter than the open procedure group.
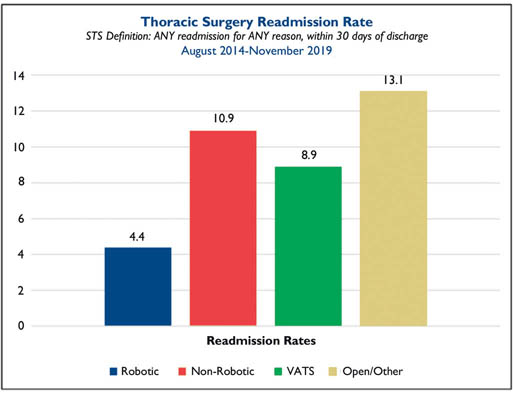
Fig. 3. Readmission rates during a five-year time period for patients operated on by robotic-assisted thoracoscopic technique compared to the non-robotic techniques (open or video-assisted), displayed as combined and individually.
The readmission rates, as seen in Fig. 3, are also superior for the robotic-assisted thoracoscopic group. Over the five-year time period, the readmission rate for the robotic assisted thoracoscopic group was half that of the VATs group, and one third that of the open technique group.
The Lancaster General Health Physicians Thoracic Surgery group continues to refine our surgical techniques and protocols so that we can offer patients a customized state-of-the-art plan for surgical intervention. We have recently implemented an aggressive enhanced recovery after surgery (ERAS) protocol, and over the past six months only 22.7% of 97 patients managed with this protocol were discharged with a prescription for opioids. Moreover, in that group of 97 patients, 10% were already on chronic opioids prior to thoracic surgical intervention. Our multi-modal pain management strategy has resulted in a significant reduction in opioid prescribing for procedures that previously were associated with substantial and often long-term disability due to pain management issues.
We are committed to learning, evolving, developing, and implementing change as leaders in thoracic surgery for the 21st century. Our goal is to provide patients with opioid-free thoracic surgery and an expedited recovery to normal activity.
REFERENCES
1. Dodds S. Hellenic News of America. Nov. 30, 2015.
2. Naef AP. The Story of Thoracic Surgery. Hogrefe & Huber, Cambridge, MA. 1990
3. Ochsner A. The history of thoracic surgery. Surg Cl N Am. 46( 6): 1357-1358.
4. American Board of Throacic Surgery Information about initial certification: https://www.abts.org/ABTS/CertificationWebPages/Initial_Certification_Page.aspx
5. Bonchek LI. Special training programs in thoracic surgery; past or prologue? Ann Thor Surg. 1977; 23(3): 199-201.
6. American Board of Throacic Surgery residency requirements: https://www.abts.org/ABTS/Initial_Certification/Residency_Requirements.aspx