Spring 2020 - Vol. 15, No. 1
Coleman Ton-That
Treatment for Fibromyalgia
Christa Coleman, PsyD, BCB
Clinical Psychologist
Penn Medicine Lancaster General Health Physicians Neuropsychology
Tony Ton-That, M.D.
Medical Director Spine/Low Back Pain
Lancaster General Health Physicians Pain Management
Second of two parts
INTRODUCTION
Fibromyalgia can have a substantial impact on both a patient’s mental and physical health. Common adverse consequences in the affected population are low rates of work, high rates of financial dependency, and poor quality of life. The treatment of fibromyalgia aims to modulate central pain pathways to reduce sensitivity, which can be achieved with a range of treatment modalities.
Effective treatment requires multimodal pharmacological treatment combined with non-pharmacological therapy. The most effective evidence-based treatment strategies include education about the nature of the condition, graded exercise programs, and psychology-based interventions. These include cognitive-based stress management therapy with a pain management psychologist, yoga, tai chi, or simple meditation. These non-pharmacological interventions are recommended by recently published guidelines: 1) The 2016 European League Against Rheumatism (EULAR) Fibromyalgia Management Guidelines; and 2) the 2012 Canadian Fibromyalgia Diagnosis and Management Guidelines.
This article provides information on the best practices and current services available for patients with fibromyalgia. These complex patients require a team approach for optimal care.
The Fibromyalgia Clinic at Penn Medicine Lancaster General Health provides state-of-the-art care by an interdisciplinary team that includes a physician who specializes in pain and rehabilitation, a clinical psychologist, an occupational therapist, a physical therapist, a case manager, and a dietitian.
PHARMACOLOGY
Below are descriptions of the multimodal pharmacological treatments currently available and approved by the FDA and international organizations to control the complex and differing symptoms reported by patients (Table 1).

Table 1. * In Europe, Milnacipran is available in France, Portugal, Finland, Estonia, Austria, Luxembourg, Poland, Turkey, Bulgaria, and Russia.
I. Serotonin and noradrenergic reuptake inhibitors (SNRIs)
Serotonin and noradrenaline are neurotransmitters involved in pain-processing pathways via their action on descending inhibitory pathways in the brain and spinal cord, with the net effect of reducing sensory input from the periphery. Both neurotransmitters have an array of other functions including roles in regulation of mood and emotion, with noradrenaline also involved in regulation of attention and memory.
Duloxetine is an SNRI originally used for the treatment of depression, but several studies have since evaluated its benefit in fibromyalgia.1 Doses can range from 30-120 mg daily, though many patients cannot tolerate doses above 60 mg. Common side effects include headache, palpitations, nausea, and flushing. Some patients find that duloxetine causes drowsiness, and they should take it before bed, while a smaller number of patients find it stimulating, and thus benefit more from taking it in early in the day.
Milnacipran is another recommended SNRI. Trial data indicated that milnacipran improved the quality of life and reduced patient-reported pain in 15% more participants than a placebo. 2 The usual dose of milnacipran is 50mg twice daily, but many patients only tolerate much smaller doses, such as 25mg once or twice daily. Patients should be initiated on a dose of 25mg daily and then titrated upwards by 25mg daily at a minimum of every few days. Milnacipran has a similar side effect profile to duloxetine, but has stronger noradrenergic qualities than duloxetine and for this reason may be more stimulating.
II. Gabapentinoids
Pregabalin was used as an antiepileptic drug but is now commonly used for pain management. It mediates its effects by binding to voltage gated calcium channels and reducing calcium influx at sensitized spinal cord neurons, thereby reducing the release of neuroactive molecules – including glutamate, substance P, and noradrenaline – into the synapse. Patients with fibromyalgia have increased levels of glutamate in their insula, an area of the brain involved in pain processing, and pregabalin can reduce these levels, leading to a decreased perception of pain. 3
Pregabalin can be initiated at a dose of 25–75mg daily, with the addition of 25–75mg every 1-2 weeks as tolerated. Common side effects include dizziness, somnolence, and weight gain. If somnolence is prominent, patients may benefit from taking pregabalin only at night to enhance sleep and minimize daytime drowsiness. Drug interactions are uncommon and pregabalin can be safely added to SNRIs, tricyclic antidepressants (TCAs), and most analgesics. It may be best for patients with prominent pain and sleep disturbance, and is less effective for fatigue.
III. Tricyclic antidepressants (TCAs)
Like SNRIs, TCAs mediate their effects via modulation of noradrenaline and serotonin, and were originally developed for the treatment of depression.
Amitriptyline is a TCA commonly prescribed for the management of fibromyalgia, and short-term studies have shown clinical improvement in 15-20% more patients taking amitriptyline compared with placebo. 4 Nortriptyline is an alternative option, but it has been evaluated in fewer studies.
Side effects from amitriptyline are common, including dry mouth, constipation, daytime drowsiness, and mental clouding. Like pregabalin, patients may benefit from taking this medication in the evening to promote sleep and minimize daytime side effects. Smaller doses are used in fibromyalgia than in depression, with between 10mg and 25mg usually prescribed as an early evening dose; doses above 50mg are seldom used for this indication. It can be co-prescribed with pregabalin, simple analgesics, and cautiously with SNRI medications. It may be helpful in patients with insomnia as a prominent clinical feature.
Cyclobenzaprine has a tricyclic structure similar to that of amitriptyline, and its common side effects are similar to those of amitriptyline, but it is not known to have antidepressant effects. Doses of 1–4 mg at night have been shown to improve sleep. Both amitriptyline and cyclobenzaprine are recommended in the EULAR and Canadian guidelines.
Tramadol is a weak opioid with mild serotonin-noradrenaline reuptake inhibition. A small study showed benefit of tramadol in combination with paracetamol in patients with fibromyalgia compared with placebo. Tramadol is recommended in the EULAR fibromyalgia guidelines, however, in the Canadian guidelines, it is suggested that tramadol be reserved for patients with significant symptoms not responding to the above-mentioned drug classes.
IV. Injection Therapies
Injection therapies can combine with manual therapies to diminish afferent drive and facilitate rehab processes. Trigger point injections using lidocaine and/or corticosteroid, Botox, dry needling, and acupuncture treatments can reduce pain, anxiety, and fatigue so patients can participate in therapy successfully. 5
V. Medications that are not recommended in fibromyalgia
A. Anti-inflammatory medications: Non-steroidal anti-inflammatory drugs (NSAIDs) and glucocorticoids act peripherally to reduce inflammation at the site of tissue damage. Given that the pain experienced by patients with fibromyalgia is not nociceptive, it is not surprising that these medications are not beneficial.
B. Opioids: Despite their common use, there is no evidence to suggest opioid medication is beneficial in fibromyalgia. To the contrary, in terms of pain, function and quality of life, these medications may be associated with significant harm and worse outcomes than in patients not taking opioids. 6,7
CASE MANAGEMENT
The RN case manager (CM) provides initial phone contact with individuals, fostering early engagement and interest in learning more about the program. The CM coordinates attendance to the FM class which provides fundamental neuroscience education and the details of the biopsychosocial treatment program. Family members are encouraged to participate from the onset of the program. There is good evidence that early and ongoing education in the neuroscience of pain enhances individuals’ participation in FM programs. 8,9
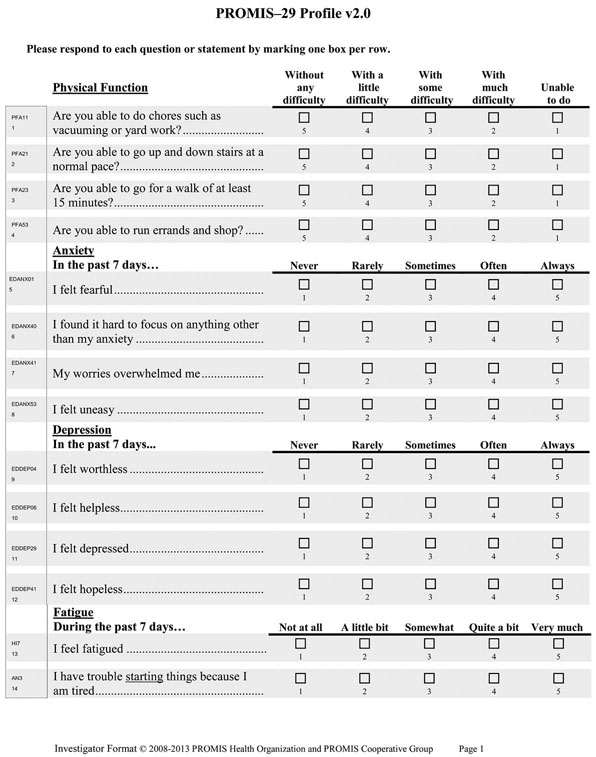
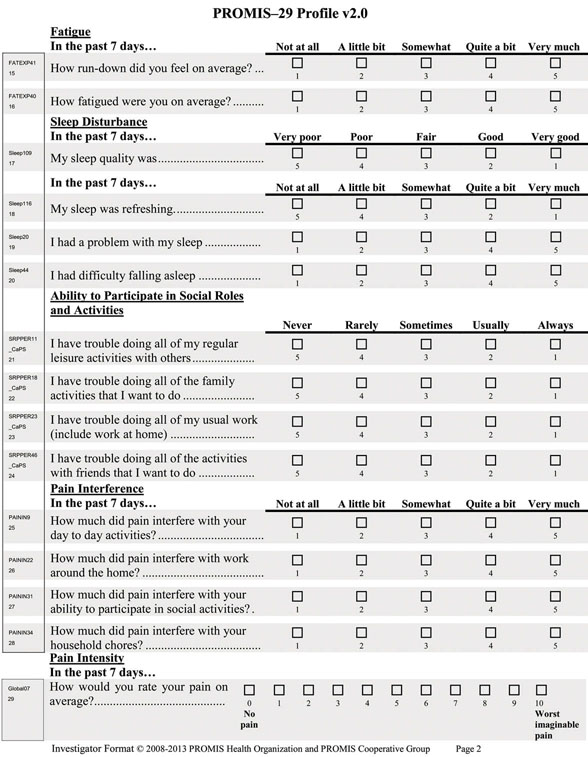
Attendance at the FM introductory class is required, prior to the initial FM intake evaluation with the three providers (OT, PT, and the pain psychologist). After completion of the class, information on individual needs are assessed with preliminary questionnaires (PROMIS-29 intake form [Patient-Reported Outcomes Measurement Information System], General Anxiety Disorder-7 [GAD-7], and the Pain Catastrophizing Scale (PCS). Upon completion, individuals are scheduled for their evaluations, at which time they meet one on one with OT, PT, and the pain psychologist. At the conclusion of these evaluations, individuals receive their comprehensive interdisciplinary recommended treatment program.
With the addition of the introductory class, we have found that the 25% “no-show” rate to the initial intake evaluation is reduced to under 10 percent. We have also found that time lapse between class attendance and the initial intake evaluation affects the no-show rate: a lapse of six weeks increased the no-show rate whereas three to four weeks maintains the no-show rate below 10 percent.
In addition to the class, the CM provides ongoing individual support to patients who require health counseling for symptoms related to fibromyalgia, communicates with the PCPs where indicated, and facilitates community resources for individuals who need support. The CM offers a once monthly support group with an educational focus that provides experience with evidence-based approaches to managing chronic pain and fatigue. The support group centers upon a guest speaker or instructor, and includes tai chi, yoga, Reiki, stress management, and music therapy. The group meets on the first Wednesday of each month from 5-6 p.m., is free of charge, and does not require pre-registration. Individuals and families are encouraged to attend when possible.
PSYCHOLOGY
Fibromyalgia is a multifaceted disorder with many co-occurring diagnoses. Psychological treatments can be offered individually or as part of a multidisciplinary or interdisciplinary program. Empirically supported psychological treatments for fibromyalgia include education about behavioral management of symptoms, various cognitive behavioral therapy (CBT) approaches, and multidisciplinary care.10 In addition, preliminary studies indicate there may be benefit to mindfulness-based interventions, emotional awareness and expression therapy, meditation, and EMG biofeedback/neurofeedback.11,12
Regarding the treatment modality, both group and individual therapy as well as telehealth/distance CBT can all be effective for this population. Although there is support for each of the identified treatments and approaches, it is essential to recognize the heterogeneity of those diagnosed with fibromyalgia and to tailor the treatment approach to the individual’s needs and circumstances; there is no one-size-fits-all approach in treating individuals with fibromyalgia. For some the greatest need might be education about their diagnosis and self-management; for others, interdisciplinary care including psychology might be needed; and yet others may benefit most from positive peer support. Overall, individualized treatment is the best care.
The role of psychology in the treatment of fibromyalgia involves identifying patients who have significant psychosocial needs, developing an individualized treatment plan, educating patients about how thoughts, emotions, and behaviors can impact pain, and working with patients on behavioral modification to better manage their unique pain experience. This may involve education and various cognitive therapy approaches to address problematic thoughts such as catastrophizing and kinesiophobia. Relaxation training or mindfulness-based interventions can help those struggling with emotional distress and pain behaviors such as muscle bracing and guarding. Activity-rest pacing is important in managing pain and fatigue. Time management and stress management are useful with strategically planning events and coping with unexpected challenges. Sleep education and CBT for insomnia can assist those struggling with insomnia and poor sleep hygiene. Yet, there may also be a need to address assertiveness and communication skills, anger management, acceptance of the diagnosis, or a number of other areas through psychological interventions.
Currently, the Fibromyalgia Clinic provides patients with psychological evaluations to identify needs, education, and resources to assist with carrying out the treatment plan, and individual and group therapy for chronic pain. Patients identified as having pain-related psychological symptoms may be referred for brief psychotherapy with a counselor through the clinic, or referred out to primary care-embedded counselors or community providers based on their preferences. They may also be referred for a brief two-session CBT chronic pain (CBT-CP) program and/or a longer eight-week CBT-CP program as deemed appropriate during their evaluation. Each individualized treatment plan is established by considering several screening measures (i.e., PCS, PHQ9, PROMIS29, GAD7), in combination with a comprehensive evaluation and patient preferences. Post-treatment assessment measures are contingent upon presenting symptoms and treatment modality.
ROLE OF OCCUPATIONAL THERAPY
Occupational therapy (OT) assists patients to define their specific areas of frustration and functional limitation with activities of daily living, and to establish a plan to address these concerns. Occupational therapy can address a multitude of limitations including the capacity of the patient to manage self-care, home management, or participation in a work or caregiver role. The adverse impact of fibromyalgia can be far reaching, including - but not limited to – restrictions in upper extremity range of motion, strength, endurance, and cognitive performance (i.e., memory, concentration); non-restorative sleep that impacts capacity for activities of daily living; and poor tolerance of stress and pain. Education and home programming help the patient to better understand how fibromyalgia affects daily life, and better positions them to independently manage the condition through exercise, adaptive approaches, and coping strategies. Occupational therapy through the fibromyalgia clinic strives to ensure the greatest level of comfort and independence for each participant, with emphasis on quality of life and establishing good lifelong management strategies.
The patient’s progress in skilled occupational therapy services is measured with the Patient Specific Functional Scale (PSFS). At the initial evaluation, the patient specifies 3-5 tasks that the patient describes as “unable” or “difficult” to complete. Examples include meal preparation, cleaning the shower, or the ability to concentrate during bill paying/financial management. Difficulty of the tasks is rated on a scale of 0-10, ranging from inability to perform it to normal and comfortable engagement in the task. An overall score is then calculated that reflects the patient’s self-reported ability to complete identified tasks. The PSFS is re-administered at each occupational therapy visit and at discharge, with the goal of improving the score as the patient progresses toward greater independence.
ROLE OF PHYSICAL THERAPY
Physical therapy (PT) evaluates specific areas of weakness, ROM limitations, muscle restrictions, and functional limitations that affect daily living. Once deficits are identified, a plan of care is developed to address them. Physical therapy can include home management techniques, education about pain, body mechanics, a comprehensive home exercise program, endurance training, manual therapy, and aquatic therapy. Postural respiration is also included as needed to address breathing and muscle deficits. Physical therapy’s role in the fibromyalgia program is to provide the patient with the tools necessary to independently manage their condition on a daily basis. The patient is educated on the body’s way of processing chronic pain, and is trained to identify his/her pain triggers in an effort to start self-management techniques prior to symptoms becoming out of control. Patients are typically seen 1-2 times per week for 4-12 weeks depending on the extent of care indicated at the initial evaluation.
Progress in skilled physical therapy services is measured using the Revised Fibromyalgia Impact Questionnaire (FIQR). At the completion of the initial evaluation, at each PT visit, and at discharge, the patient completes a form that assesses function and overall fibromyalgia symptoms. Patients rate their status on a scale from 0 to 10 based on their experience in the last seven days. The goal from intake to discharge is a reduced score of at least 14%, reflecting a statistically significant reduction in patient symptoms and improvement in activity tolerance.
DIETITIAN
We are very excited about the addition of a clinical dietitian to our team. The dietitian offers a twice-monthly class to provide nutritional support and education for people with chronic pain conditions. The focus is an anti-inflammatory diet, and guidance is provided for grocery shopping and label reading, mindful eating, and weight management to reduce chronic pain and fatigue. This class is offered every other Thursday from 11 a.m. to noon, is also free of charge, and does not require pre-registration.
OTHER SERVICES
The overarching goal is to provide a continuous supportive community through comprehensive programs that are free and accessible to individuals and their families. Future plans include the addition of once monthly physical conditioning programs, such as gentle yoga or tai chi, to emphasize the importance of a lifestyle of physical activity to increase function and to combat chronic pain and fatigue.
Future changes may also include CM triage to assess which individuals require a la carte services with CM, physician, pain psychology, OT, and/or PT. Additional ongoing care conferences and formalized inter-team communication will assist in identifying individuals who require additional support and services or a change in their treatment program. Finally, improved tracking of patient progress throughout the program with PROMIS 29 scores at regular intervals and at discharge from the program, will provide helpful insight into areas for further improvement and areas of need.
ACKNOWLEDGEMENTS
Also contributing to this article, were:
Jessica C. Thomas OTR/L, occupational therapist;
Holly Leonard, DPT, physical therapist
Sue Hopkins, RN, case manager.
REFERENCES
1. Russell IJ, Mease PJ, Smith TR et al. Efficacy and safety of duloxetine for treatment of fibromyalgia in patients with or without major depressive disorder: results from a 6-month, randomized, double-blind, placebo-controlled, fixed-dose trial. Pain 2008;136(3):432–444.
2. Mease PJ, Clauw DJ, Gendreau RM et al. The efficacy and safety of milnacipran for treatment of fibromyalgia. a randomized, double-blind, placebo-controlled trial. J Rheumatol. 2009;36(2): 398–340
3. Harris RE, Napadow V, Huggins JP et al. Pregabalin rectifies aberrant brain chemistry, connectivity, and functional response in chronic pain patients. Anesthesiol. 2013;119(6):1453–1464.
4. Carette S, Bell MJ, Reynolds WJ et al. Comparison of amitriptyline, cyclobenzaprine, and placebo in the treatment of fibromyalgia. A randomized, double-blind clinical trial. Arthritis Rheum 1994;37(1):32–40.
5. Martin DP, Sletten CD, Williams BA, et al. Improvement in fibromyalgia symptoms with acupuncture: results of a randomized controlled trial. Mayo Clin Proc. 2006;81(6):749-57.
6. Goldenberg DL, Clauw DJ, Palmer RE et al. Opioid use in fibromyalgia: A cautionary tale. Mayo Clin Proc. 2016;91(5):640–648
7. Peng X, Robinson RL, Mease P et al. Long-term evaluation of opioid treatment in fibromyalgia. Clin J Pain 2015;31(1):7–13
8. Arnold LM, Clauw DJ, Dunegan LJ, et al. Fibromyalgia management: A framework for fibromyalgia management for primary care physicians, FibroCollaborative. Pifzer. 2010
9. Clauw D. J., Lesley, M., Arnold, & McCarberg,B.H. (2011)The science of fibromyalgia, Mayo Clin Proc. 2011; 86(9): 488-496.
10. Castelnuovo G, Giusti EM, Manzoni GM et al. Psychological treatments and psychotherapies in the neurorehabilitation of pain: Evidences and recommendations from the Italian consensus conference on pain in neurorehabilitation. Front Psychol. 19 February 2016. https://doi.org/10.3389/fpsyg.2016.00115
11. Van Gordon W, Shonin E, Dunn TJ, et al. Meditation awareness training for the treatment of fibromyalgia syndrome: A randomized controlled trial. Brit J Health Psychol. 2017;22(1):186-206. doi:10.1111/bjhp.12224.
12. Theadom A, Cropley M, Smith HE, et al. Mind and body therapy for fibromyalgia. Cochrane Database of Systematic Reviews. 2015;(4): doi:10.1002/14651858.CD001980.pub