
Winter 2019 - Vol. 14, No. 4
Rising Maternal Mortality:
Key Concepts and Opportunities for Intervention
Rebecca A. Sieber, MD, MSW, FACOG
Obstetrician Gynecologist
Penn Medicine Lancaster General Health Lancaster Physicians for Women
INTRODUCTION
Women in the United States are dying from pregnancy-related causes at a rate higher than any other high-resource nation, ranking 30th in the world. Each year approximately 700 American women die of complications from pregnancy and childbirth, and an additional 50,000 women experience severe morbidity.
1 It is estimated that at least half of maternal deaths in this country are preventable.
2 Even more disturbing are the stark racial disparities that exist, with African-American women being three to four times more likely to die than white women.
1
The United States was not always this far behind. As medicine made great advances in the 20th century, maternal mortality rates in the United States steadily declined to reach an all-time low in 1987. Since then, the trend has reversed and U.S maternal mortality rates have steadily risen (Fig. 1).
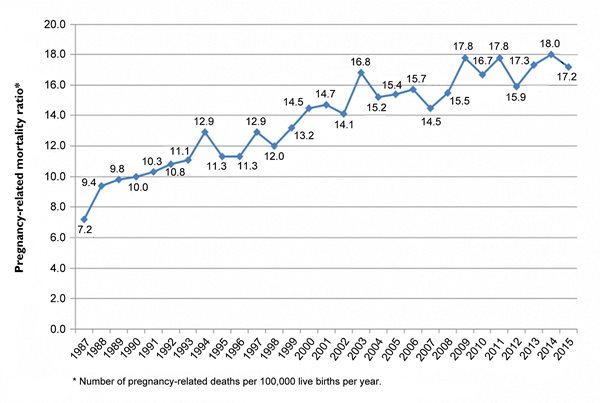
Fig. 1. Trends in Pregnancy-Related Mortality in the United States 1987-2015. Source: Centers for Disease Control and Prevention Pregnancy Mortality Surveillance System.
We see a very different picture worldwide, with maternal mortality rates continually decreasing over time, reflecting strides in both technology and access to care.
It is important to understand which deaths are considered pregnancy-related. The Centers for Disease Control and Prevention defines a pregnancy-related death as the death of a woman during or within one year of pregnancy that was caused by a pregnancy complication, a chain of events initiated by pregnancy, or the aggravation of an unrelated condition by the physiologic effects of pregnancy. The maternal mortality ratio is the number of pregnancy-related deaths per 100,000 live births.
It is tragic that we are losing mothers at such a high rate in a country with unmatched wealth, resources, and technology. Unfortunately, there is nothing simple or straightforward about the problem and solutions will need to be equally complex, involving individuals at all levels and specialties in the health care system.
COMMON CAUSES OF DEATH – A CONCERNING TREND
Historically, hemorrhage, hypertension, infection, and venous thromboembolism were the leading causes of pregnancy-related deaths in the United States; and worldwide, they still are. While these causes continue to claim lives each year, acquired cardiovascular disease has emerged as the leading cause of pregnancy-related death, with heart failure, myocardial infarction, arrhythmias, and aortic dissection topping the list.
3 Other rising causes of death include non-obstetric, non-cardiac medical conditions, such as pulmonary or renal disease (Fig. 2).
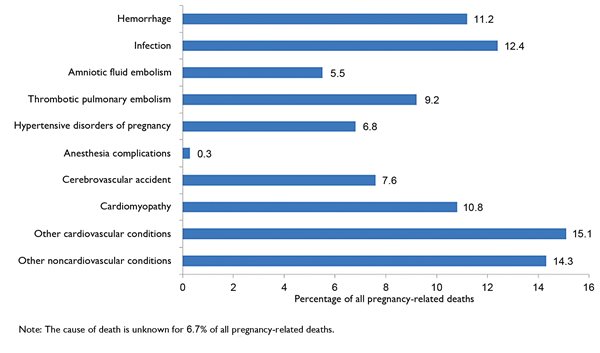
Fig. 2. Causes of Pregnancy-Related Death in the United States 2011-2015. Source: Centers for Disease Control and Prevention Pregnancy Mortality Surveillance System.
It is worth noting that the majority of maternal deaths do not occur on the labor floor. Only one third of deaths occur during childbirth or within a week of delivery; one third occur during pregnancy; and the final third occur during the period between one week and one year postpartum.
4
WHY IS THE UNITED STATES SO FAR BEHIND?
The fact that cardiovascular conditions are now the leading cause of pregnancy-related deaths in the United States highlights one of the most significant reasons we are lagging behind the rest of the developed world – we are unhealthier. We have higher (and ever increasing) rates of obesity, as well as obesity-related health conditions such as hypertension and diabetes. Furthermore, women in the United States are continuing to delay childbearing. Those women who deliver after age 40 have markedly higher rates of mortality and serious morbidity when compared with younger women.
5,6 In addition, women with significant chronic illnesses such as congenital heart disease and pulmonary disease are now surviving to childbearing age. As mentioned above, at least half of maternal deaths in the United States are preventable. The lack of standardization among hospitals and providers in treating common preventable causes of pregnancy-related deaths (such as hemorrhage and hypertension) contributes significantly to our higher death and complication rates.
It is also worth noting that nearly every other high-resource nation with lower maternal mortality rates than ours, has some form of universal health coverage that continues after delivery. It is estimated that Medicaid covers nearly half of births in the United States, and for the majority of women this coverage stops by 60 days postpartum. Since pregnancy-related deaths are counted until one year postpartum, one can infer that a significant number of deaths occur in women who lack medical insurance.
RACIAL DISPARITIES
Maternal mortality does not affect all American women equally, with black women fairing markedly worse than any other racial group (Fig. 3).

Fig. 3. Pregnancy-Related Mortality Ratios by Age, Race-Ethnicity, and Overall for 2011-2013. Source: Creanga AA, Syverson C, Seed K, Callaghan WM. Pregnancy-related mortality in the United States, 2011-2013. Obstet Gynecol 2017; 130:366-372.
Socioeconomic factors undoubtedly contribute to this disparity, but even after controlling for income and education, black women are still far more likely to die than white women. We know that African American women have higher rates of chronic diseases such as hypertension and diabetes, but why this occurs is a complex issue, with factors such as chronic stress playing an inevitable role.
Predisposing factors aside, African American women do not always receive equivalent medical care. Implicit bias within the health care system is seldom acknowledged but is a critically important reason for the striking racial disparities in women’s health. In 2017, ProPublica and National Public Radio conducted a series of interviews with over 200 African American women regarding their experiences in the U.S. health care system during their pregnancy and postpartum period. These women consistently reported feeling undervalued, not taken seriously, and not believed by medical staff and providers.
7
WHAT IS BEING DONE?
As the nation has awakened to this crisis, there have been legislative changes at both state and federal levels. In December 2018, Congress passed the “Preventing Maternal Deaths Act” which authorizes the CDC to assist states in creating or expanding their Maternal Mortality Review Committees (MMRCs), and provides additional funding for research. Pennsylvania established an MMRC just this last year, which consists of a multidisciplinary group of individuals who review each maternal death in the state, looking for trends and opportunities for change.
A new Pennsylvania Perinatal Quality Collaborative meets regularly, with the goal of identifying health care processes that need to be improved, and implementing changes across the Commonwealth. California has led the way in terms of standardizing treatment for the primary causes of preventable death. For example, California has implemented evidence-based tool kits or “bundles” to address common contributors to maternal morbidity and mortality (hemorrhage, hypertension, and now cardiovascular disease), and has implemented quality improvement programs throughout the state. As a result, they have seen a marked reduction in their maternal mortality rate over the last 15 years.
8
WHAT CAN HEALTH CARE PROVIDERS DO?
Women of childbearing age do not only see obstetrician-gynecologists; they interact with the health care system in a variety of ways and see a myriad of specialists. There are opportunities for providers in all specialties to intervene prior to, during, and after pregnancy.
Before pregnancy
• Help prevent unwanted or unplanned pregnancy! Not only should we increase women’s access to safe and affordable family planning, we need to ask the question, “Are you planning to become pregnant in the next year?” If not, prescribe or refer for contraception.
•. Optimize management of overall health and chronic diseases prior to pregnancy. Prevention of health problems such as obesity, hypertension, and diabetes starts in childhood and is a lifelong process of encouraging healthy habits.
•. Encourage patients with high-risk cardiac or other conditions to consult with a maternal fetal medicine specialist or obstetrician prior to becoming pregnant. Women deserve to know about the potential dangers of pregnancy so they can make informed decisions about their health.
During Pregnancy and Childbirth
• Provide easy and early access to quality prenatal care with referral to specialists when needed.
• Ensure patients deliver at a hospital with an appropriate level of care. For example, women with high-risk cardiac conditions should deliver at a tertiary care center with immediate access to perinatology, cardiology, and critical care physicians.
• Standardize the approach to common intrapartum conditions such as hypertension and hemorrhage. Use of tool kits or standard algorithms has been shown to greatly decrease the severe morbidity and mortality associated with these conditions.
9,10
• Maintain a high index of suspicion! Many symptoms normally attributed to the discomforts of pregnancy, such as headaches, swelling, shortness of breath, or palpitations, can also be signs of dangerous cardiovascular or pulmonary conditions.
Postpartum
Given the large proportion of maternal deaths occurring in the postpartum period, The American College of Obstetrics and Gynecology recommends that we rethink the postpartum period as one in which women receive ongoing care, rather than consisting of a single encounter six weeks after delivery.
11
• Increase access to quality postpartum care through one year after birth. Given the implications that expansion of postpartum care would have for both office flow and reimbursement, it will require creative thinking to find solutions that work for both providers and patients.
12
• Advocate for the expansion of Medicaid eligibility to one year postpartum
• Educate patients and primary care providers about worrisome symptoms that can develop in the postpartum period. Remember that the danger is not over once a healthy baby has been born.
CONCLUSION
U.S. maternal mortality rates are shocking and discouraging. Much is being done to address this complex problem, but we have far to go. Making change at a systems level is crucial, but it behooves all of us to examine whether we can personally improve the care that we provide women in our community. In order to begin to tackle the problem of racial disparities in pregnancy outcomes, we all need to identify and address our own implicit biases. This is uncomfortable work, but until we acknowledge our biases, we cannot change them. Finally, and most importantly, we need to believe women when they tell us something is wrong. Even those who do not provide maternity care can advocate for women and refer them to appropriate care before it is too late.
REFERENCES
1. Centers for Disease Control and prevention. Pregnancy mortality surveillance system.
https://www.cdc/gov/reproductive health/maternalinfanthealth/pmss.html . Updated June 4, 2019. Accessed September 30, 2019.
2. Berg CJ, Harper MA, Atkinson SM, et al. Preventability of pregnancy-related deaths: results of a state-wide review.
Obstet Gynecol 2005;106:1228-1234.
3. Hameed AB, Lawton ES, McCain C et al. Pregnancy-related cardiovascular deaths in California: beyond peripartum cardiomyopathy.
Am J Obstet Gynecol 2015; 213:e1-210.
4. Creanga AA, Syverson C, Seed K, et al. Pregnancy-related mortality in the United States 2011-2013.
Obstet Gynecol 2017; 130:366-373.
5. Creanga AA, Berg CJ, Syverson C, et al. Pregnancy-related mortality in the United States, 2006-2010.
Obstet Gynecol 2015; 125:5-12.
6. MacDorman MF, Declerq E, Thomas, ME. Trends in maternal mortality by sociodemographic characteristics and cause of death in 27 states and the District of Columbia.
Obstet Gynecol 2017: 129:811-818.
7. Propublica.org/article/nothing-protects-black-women-from-dying-in-pregnancy
8. Macdorman MF, Declerq E, Cabral H, et al. Recent increases in the U.S. maternal mortality rate: disentangling trends from measurement issues.
Obstet Gynecol 2016; 128:447-455.
9. Mann S, Hollier LM, McKay K et al. What we can do about maternal mortality – and how to do it quickly.
N Engl J Med 218; 379:1689-1691.
10. Bernstein, PS, Combs CA, Shields LE et al. The development and implementation of checklists in obstetrics. Society for Maternal-Fetal Medicine 2017; B2-B5
11. Optimizing postpartum care. Committee Opinion No 736. American College of Obstetricians and Gynecologists.
Obstet Gynecol 2018;131:e140-148.
12. Murray Horwitz ME, Molina RL, et al. Postpartum care in the United States – new policies for a new paradigm.
N Engl J Med 2018.; 379:1691-1693.