Summer 2019 - Vol. 14, No. 2
Urgent Care Part 2: Meeting a Growing Demand

 DiCamillo Harris
DiCamillo Harris
Vito J. DiCamillo, M.D.
Medical Director Urgent Care
Penn Medicine Lancaster General Health Physicians
Stacey Lee Harris
Director of Operations - Medical Specialty
Urgent Care & Women's and Pediatrics
Penn Medicine Lancaster General Health
Editor’s note: This timely article is the second of a two-part series. The first article, published in the last issue of JLGH, focused on the consumer demand that has fueled the dramatic growth of urgent care in Lancaster County.1 The current article examines clinical aspects of the model used by Penn Medicine Lancaster General Health to deliver urgent care.
INTRODUCTION
The primary factors influencing the increase in utilization of Urgent Care (UC) nationally and locally are convenience and accessibility. Customers want care at a time and place that is convenient for
them as opposed to the
provider.2 The leadership of Penn Medicine Lancaster General Health had the foresight a decade ago to realize this trend, and strategically planned and grew their on-demand presence.
A 21.7% increase in visits from 88,423 in FY 2017 to 107,652 visits in FY 2019 is further evidence that customers want on-demand care. Almost 10% of all outpatient visits this year will be to one of our six UCs, which underscores the importance of meeting patients on their own terms at a time a place that fits their busy schedules. In further response to consumer demand, LG Health will open a seventh UC in Elizabethtown in November, to be known as Norlanco Urgent Care.
The third most important reason for increased utilization is affordability. Patients are becoming responsible for a greater share of the cost of their health care. A UC visit is one fifth the cost of an emergency department (ED) visit, thus offering an affordable alternative for people with immediate health care needs.
3
The last factor in the equation is the quality of health care the customer receives. Patients not only expect convenient, affordable care, but they want it to be in a clean, modern environment, practiced in an evidence-based manner, by highly qualified providers. As we move from a fee-for-service model to one based on case-rates, and finally to a payment model driven by quality, UC will need to keep a close eye on quality metrics. Fortunately, as part of a top tier community hospital system, quality has been top-of-mind since our UC’s inception. Unlike some of our competitors who are trying to play catch-up, quality is part of the fabric that makes LG Health a standout among its peers.
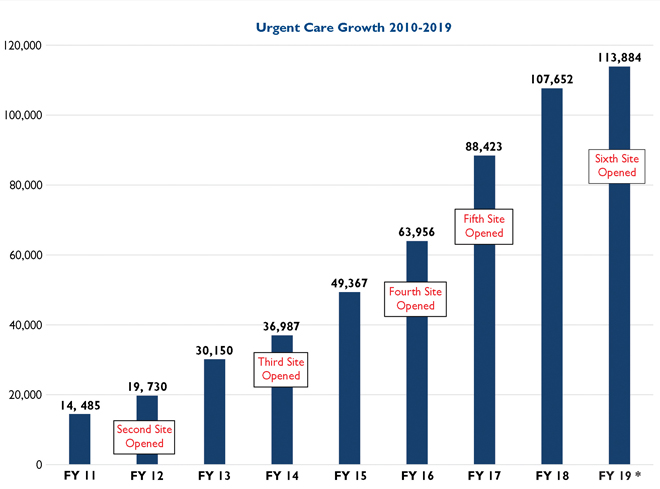
Fig. 1. LG Health Urgent Care Growth over the last decade. *Fiscal Year 2019 has been annualized.
CLINICAL SPECTRUM OF UC CARE
Ideally, the UC will see patients for their acute health care needs, and occasionally for follow up on a serious illness or to remove sutures. But the most common reason for a patient to return is that they did not receive antibiotics on the first visit. Unfortunately, there is a misconception among the general public that antibiotics are necessary for all illnesses.
4 When OTC (over-the-counter) treatments do not immediately cure them, it is not uncommon for patients to return. As good antibiotic stewards, we accept this level of unplanned follow up as part of the process of giving excellent, quality driven, evidence-based care.
The national average of patients requiring ED referral from UC is 3%. In FY 2018, the rate of referral to the ED from LG Health UC was 1%, which is markedly lower than the national benchmark.
5 Caring for the majority of the patients in the UC instead of triaging them to the ED undoubtedly has helped mitigate the ED overcrowding that is a national problem, but in the best interest of patient quality and safety, patients who present with a problem that is out of the scope of UC practice are immediately referred or transported to the ED after a process of triaging by a provider.
Typical reasons for ED referral include chest pain, dizziness, and stroke-like symptoms. Many other medical issues can be evaluated and treated in a UC with close follow up by the appropriate consultant or PCP within a few days. A typical example is a non-displaced, non-surgical fracture. In the UC, the patient is usually managed with imaging, splinting, and pain management; an ambulatory referral is placed, or the patient is directly scheduled with orthopedics or sports medicine. Definitive care and fracture management, which may include casting and physical therapy, are provided as an outpatient.
Some of the most common indications for immediate outpatient consultation are acute ocular or ENT emergencies, such as acute angle closure glaucoma or a peritonsillar abscess. Our typical workflow would be to send these patients to their specialist of choice. If they do not have a consultant on record, we attempt to schedule them in a timely manner with a provider who is part of LG Health or our Clinically Integrated Network (CIN), taking geography and patient preferences into consideration. The hospital’s unassigned monthly call list is shared and utilized as a means of fairly distributing new patients.
THE UC MODELS OF CARE
By continually evaluating our data, we perceived an opportunity to expand our services and help decrease unnecessary ED visits and health care costs. In August 2018 we opened a new model of UC in Lititz, consisting of additional treatment rooms that are used for services such as hydration, cardiac monitoring, and head injury workups including close monitoring for up to three hours.
Staffing Models
Presently, we operate with two staffing models. Our primary model is that of an Advanced Practice Clinician (APC) working alongside a physician. Our second model uses only APCs.
Each location functions with at least two providers on each shift, but there are three at our busiest locations. APCs and physicians alternate seeing patients in sequence as the patients reach the examining area. Patients are not preferentially seen by one type of provider, and at the end of most shifts, the two providers will have seen the same number of patients. Occasionally a patient will ask to see a physician instead of an APC, or will request a male or female provider. We do our best accommodate the patient’s requests, while at the same time utilizing the opportunity as a teachable moment.
In the typical staffing model, each provider (APC or physician) is supported by one staff member (nurse or Certified Medical Assistant), and one front desk person (CMA or Certified Surgical Assistant). All locations function with at least two providers. Rohrerstown UC and Parkesburg UC regularly schedule three providers on a shift. At a few of our locations, a radiology technician takes images and brings patients to exam rooms.
These providers are supported by a front desk supervisor, a nursing supervisor, and a program manager, who rotate among three sites, so there is usually a manager at each site. Overseeing all six UCs are a director of operations, an associate medical director, and a medical director. The medical director and the associate medical director work clinical shifts at all six locations, and the director of operations visits all six.
Our ratio of two APCs for each doctor is in line with national trends. There are several reasons for the uptick in APC utilization in the UC world. First, the type of patients seen in the UC fits nicely into the scope of practice for an APC. Second, there continues to be a shortage of physicians as a whole.
6 Third, we at LG Health UC believe that our APCs can provide care with as high quality as our physicians. We expect them to practice to the full extent of their license. They practice independently, but have the back up of seven physicians at a given time. We would expect to see a continued movement towards a 1:4 ratio of physicians to APCs, in keeping with Pennsylvania State Board of Medicine rules and regulations.
Staff Recruitment and Retention
Fortunately, UC has finally reached a steady state from a recruitment and retention standpoint. UC management has worked diligently to create a high performing, quality driven practice, with a focus on provider wellness. For FY 2019 we have had a provider retention rate of 96.3%, against a system goal of 88%.
Several factors account for this experience. First, to create this culture we focused on personal and group accountability. We then looked at pay parity. We shifted from provider pay that was based on Work Relative Value Units (wRVUs), to pay based on quality and experience. APCs and physicians participate in the same Quality Improvement Plan (QIP). We prioritized APC education, committee involvement, and informal mentorship. Taking into consideration family life and the glide path to retirement, we created many half-time positions. EPIC optimization is mandated for all new employees, as EPIC efficiency goes hand in hand with provider wellness. A 36-hour clinical work week was instituted in July 2018. Weekend responsibilities were changed from every other weekend to every third. Lastly, administrative time has been factored in as standard work. Many changes were made in response to the competitive environment, but the primary focus has been provider wellness. These implementations have had tremendous impact on employee recruitment and retention.
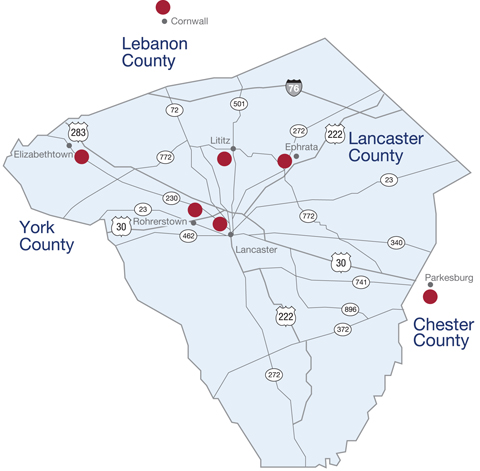
Fig. 2. LG Health Urgent Care locations by the end of 2019
Serving the Needs of the Public
Our primary and secondary markets do not consist of one homogeneous population. Within a given county, patient characteristics even differ from township to township. A cookie cutter, one-size fits all approach to urgent care medicine would not adequately fulfill the needs of the patients in our communities. As a result, our outpatient facilities and the UCs within them are tailored to the individual populations we serve.
We have had to take a micro-market approach to development and staffing. For example, some of our facilities open early or have extended visit hours. Another practice with a large geriatric population can evaluate adult patients with head injuries. Several of our facilities cater to a large population of plain folk and Amish. Two are easily accessible for the underserved inner city population. While we look at each location individually, we have not lost focus on our primary mission of giving high quality, low cost, replicable health care that our patients have come to know and expect.
Since 2010 we have seen double-digit growth in our UC visits. In FY 2019 there has been some leveling off, the causes of which appears to be two-fold. First, our primary care practices have being doing an excellent job of increasing access for their patients. Whether through expanded hours, weekend visits, or walk in availability, we have seen a trend in our LG Health practices toward immediate or same-day availability. As a result, our UCs are being appropriately utilized less by the patients that have better access to their own medical homes. Second, there appears to be some degree of market saturation. A population of 500,000 would be adequately served by 10 facilities seeing at least 60 patients a day.
5 At the time of publication, there are 12 facilities (including our six) in our primary and secondary services areas.
THE FUTURE
Moving forward, it is our belief that we should be focusing on “doing UC well” by giving the patients of Lancaster, southern Lebanon, and western Chester counties the best high-quality, affordable, on-demand healthcare we can give. Growth, though important, is secondary to doing our best in our various locations for the populations we already serve. Continued collaboration with our primary care network and CIN participants, especially around closing quality metric gaps, will be of utmost importance.
Because of our market share, commitment to population health, tight knit medical community, and our robust Electronic Health Records (EHR), we are well positioned to succeed at this monumental task into the future. Additional brick and mortar UC facilities in certain underserved micro-markets are under consideration; however, large scale growth would be impractical and fiscally unsound. More likely, innovative platforms like telemedicine will continue to drive health care costs down, while improving quality and accessibility.
7 These technological advancements have the ability to replace or augment the on-demand medicine we see today. Our UC facilities are telemedicine ready. We are prepared to see our patients by any means necessary, whether in person, by phone, or through video monitoring.
REFERENCES
1. Wynne SP, Harris SL, DiCamillo VJ. Urgent Care: meeting a growing demand.
J Lanc Gen Hosp. 2019(1);14:15-19.
2. Castaneda R. Three reasons behind the meteoric rise of urgent care clinics.
US News and World Report. Dec 10, 2018.
https://health.usnews.com/health-care/patient-advice/articles/2018-12-10/should-i-go-to-urgent-care
3. Poon SJ, Schuur JD, Mehrotra A. Trends in visit to acute care venues for treatment of low-acuity conditions in the United States from 2008 to 2015.
JAMA Internal Medicine. 2018;178 (10): 1342-1349
4. Sweeney, P. Improving appropriate antibiotic use for common clinical conditions in urgent care.
J Urgent Care Med online:
https://www.jucm.com/improving-appropriate-antibiotic-use-common-clinical-conditions-urgent-care/
5. 2017 benchmarking report - Urgent Care Association of America.
https://www.ucaoa.org/Resources/Industry-Reports/Benchmarking
6. Addressing the nation’s primary care shortage: advance practice clinician and innovative care delivery models. Available at: https://www.unitedhealthgroup.com/content/dam/UHG/PDF/2018/UHG-Primary-Care-Report-2018.pdf. Accessed April 4, 2019.
7. Strongwater, S, Kimura, J. The evolution of primary care: embracing innovation while protecting the core value. NEJM Catalyst. November 15, 2018.
https://catalyst.nejm.org/primary-care-value-disruptive-innovation/