Summer 2019 - Vol. 14, No. 2

PHOTO QUIZ FROM NEUROSURGERY
Does a 25-Year-Old Woman
Need Glasses or Brain Surgery?
Kristine Dziurzynski, M.D.
Penn Medicine Lancaster General Health Physicians
NeuroScience & Spine Associates
CASE HISTORY
A healthy appearing 25-year-old woman with no past medical history presented with blurry vision which had worsened recently during the latter months of her recent pregnancy, and delivery of her second child. She believed she needed corrective glasses.
She had headaches which, at worst, she considered mild. She denied diplopia, visual loss, nausea or vomiting. On examination she was pleasant, calm, and in no distress. Evaluation of her fundus revealed marked papilledema, prompting an MRI. (Fig. 1)
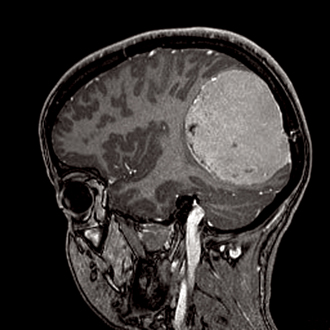
Fig. 1. MRI taken prior to surgery.
1. Do these findings likely represent a benign or a malignant process?
It is clear this is a neoplasm. Its round symmetric appearance, and location arising from the dura, suggest a meningioma, which is the most common reported tumor in the United Srates.
1 Approximately two thirds are benign, and one third are malignant. Although this tumor appears to be most likely benign, adverse sequelae have occurred as a result of the mass effect, resulting in papilledema and compromised vision.
2. Is it significant that her symptoms occurred after pregnancy?
Yes. Meningiomas are known to express both estrogen and progesterone receptors. During pregnancy, levels of both hormones rise, with an increase in progesterone from the placenta during the second trimester. Most likely, this patient’s tumor was present at the onset of gestation, followed by a pattern of linear growth that correlated with the pregnancy. As the brain is primarily composed of fat, it is soft, compressible, and has the capacity to accommodate a mass this size except when exponential growth occurs.
3. Does this patient require transfer to the Emergency Department?
No, provided there have been no further changes in her exam, no worsening of her headaches, and no nausea or vomiting. However, considering the striking findings, immediate consultation with a neurosurgeon is warranted, who will assume care and determine disposition.
After consultation with neurosurgery about the MRI results, the patient was seen by neurosurgery in clinic a few days later, and surgery was scheduled for the following week. The operation was successful in removing all the tumor.
(Fig. 2)
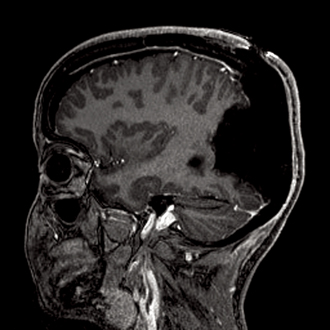
Fig. 2. MRI taken following surgery.
Ideally, to prevent recurrence of a meningioma, the tumor and a 1 cm margin of its dural attachment should be removed,
2 but this is not always possible. Fortunately for this patient, it was possible to obtain this margin.
Tumor pathology identified a grade I meningioma, which is benign. Staining for estrogen and progesterone receptors revealed the presence of progesterone receptors, but not estrogen receptors. Clinically, the patient did very well post operatively. No new deficits were incurred, and a few days later she was discharged home. Her vision returned to her normal baseline.
4. Since the tumor was completely removed, with clean margins, is there still chance of recurrence?
Yes. It has been shown that up to 20% of meningiomas that have grossly been totally resected can recur within 20 years.
3 Thus, these patients should be followed by the patient’s neurosurgeon with interval MRIs to monitor for recurrence. The MRIs are obtained yearly at first, with gradual increases in the intervals between studies.
5. If such a patient presents to their primary care doctor in the months or even years after surgery complaining of headaches, should an MRI always be obtained?
Yes, if the headache is persistent, especially if worsening in severity. An MRI is also warranted for new onset seizures or a neurological deficit. Usually these patients are monitored closely enough with MRIs that recurrence is detected prior to the development of symptoms, so regular follow up with neurosurgery to maintain this surveillance is important. In addition, this long-term relationship enables questions of uncertainty to be referred to the neurosurgeon who is familiar with the patient.
6. Are exogenous hormones safe for women with meningiomas?
Meningiomas have a higher incidence in women.
4 Published data are unclear regarding a specific risk, as there aren’t enough data sets with large enough numbers of patients who are taking exogenous hormones at the time, or around the time, of diagnosis. The question is complicated further, since pathological analysis of ex-vivo tumor tissue does not routinely include testing for hormone receptors unless it is specifically requested.
However, in addition to the higher incidence of meningiomas in women, there are data that suggest a potential association with use of exogenous hormones. Meningiomas also have a higher incidence in women with a history of uterine fibroids,
5,6 endometriosis,
6 and possibly breast cancer,
6 as well as a variation in tumor size during the luteal phase of the menstrual cycle and – as in the present case – pregnancy.
7
Since all these phenomena have a hormonal relationship, it can be inferred that it may be safer to avoid exogenous hormones if a diagnosis of meningioma has been established.
REFERENCES
1. Louis DN et al. Working Group for The WHO Classification of Tumors of the Central Nervous System 2016; Revised 4th Edition: 232
2. Gallaher MJ, Jenkinson MD, Brodbelt AR, et al. WHO grade 1 meningioma recurrence: Are location and Simpson grade still relevant?
Clin Neurol Neurosurg. 2016; 141: 117-21
3. Jaaskelainen J. Seemingly complete removal of histologically benign intracranial meningioma: late recurrence rate and factors predicting recurrence in 657 patients. A multivariate analysis.
Surg Neurol. 1986; 26: 461-9
4. Ostrom QT, Gittleman H, Truitt G, et al. CBTRUS Statistical Report: Primary Brain and Central Nervous System Tumors Diagnosed in the United States in 2011–2015.
Neuro Oncol 2018; 20 (suppl 4):
5. Claus EB, Calvocoressi L, Bondy ML, et al. Family and personal medical history and risk of meningioma.
J Neurosurg. 2011; 115: 1072-1077
6. Johnson DR, Olson JE, Vierkant RA, et al. Risk factors for meningioma in post-menopausal women: results from the Iowa Women’s Health Study.
Neuro Oncol. 2011; 13: 1011-1019.
7. Wiemels JL, Wrensch M, Claus EB: Epidemiology and etiology of meningioma.
J Neurooncol 2010; 99:3017-314