
FALL 2018 - Vol. 13, No. 3
The Challenge of Durability in Hip Replacement
Gregory A. Tocks, D.O.
Orthopedic Associates of Lancaster Ltd.
INTRODUCTION
Hip replacement is a very common operation, and the number of long-term postoperative survivors is growing continuously. According to the CDC, in 2010 there were 310,800 total hip replacements in the United States,
1 and by 2030 an annual total of 572,000 is projected.
2 In 2017, 739 total hip replacements were performed at Lancaster General Hospital.
Since long-term survivors are at risk of needing a revision procedure, the durability of their prostheses, particularly at the bearing surfaces, is a major concern. Because of the stresses at the hip joint, the ideal component should minimize wear, maintain stability, and preserve longevity. This article provides an outline of the common prosthetic bearing surfaces for total hip replacement, their comparative wear characteristics, advantages, and disadvantages.
The techniques of hip surgery are not the focus of this article, but for the interested reader, the common surgical approaches and methods of hip arthroplasty are illustrated on the websites of one of the prosthesis manufacturers.
3
PROBLEM OF WEAR IN POLYETHYLENE ACETABULAR LINERS
Currently, total hip arthroplasties consist of a femoral stem prosthesis, a modular femoral head, a modular acetabular liner, and an implanted acetabular cup (Figs. 1, 2).

Fig. 1 Illustration of pink ceramic femoral head, white polyethylene liner, and metal acetabular cup. The femoral stem prosthesis is not shown. (From Depuy Pinnacle Polyethylene technique guide.
3).

Fig. 2
A: Acetabular cup with cobalt-chromium femoral head and highly crossed-linked polyethylene liner;
B: Acetabular cup with ceramic femoral head and highly crossed-linked polyethylene liner;
C: Acetabular cup with ceramic femoral head and ceramic liner.
The acetabular liner is a polyethylene implant that is generally impacted into the acetabular cup. During the life of a total hip arthroplasty, wear primarily affects the polyethylene acetabular liner.
The Consequences of Wear
The wearing process in polyethylene liners produces small particles of polyethylene debris. The immune system responds by releasing macrophages and associated cytokines (e.g. TNF-α), which activate osteoclasts that produce osteolysis around the hip joint (Fig. 3).
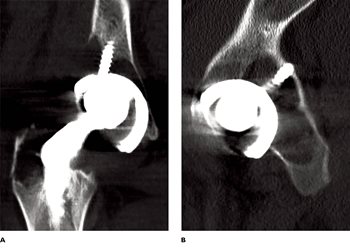
Fig. 3. CT scan coronal (A) and axial (B) images showing significant osteolysis behind
the previously implanted acetabular cup.
The loss of bone causes micromotion of the hip implants, and further potentiates osteolysis. As a result of the osteolysis and wear, patients are at increased risk of several consequences, including periprosthetic fractures from simple falls or minor trauma, aseptic loosening of the prosthesis, or dislocation of the prosthesis.
Conventional Polyethylene and Highly Crossed-Linked Polyethylene
The polyethylene component has gone through two generations, termed “conventional polyethylene,” (CP) and “highly crossed-linked polyethylene” (XPE). In CP, radiation is used to form the hydrocarbon bonds, and the irradiation produces free radicals. If oxygen binds at the site of free radical formation, the resulting oxidation degrades the material’s properties. CP is irradiated with doses of 25-40 kGy,
* and XPE is irradiated with doses of 50-100 kGy. The higher dose increases the cross-linking potential between free radicals, but radiation doses greater than 100 kGy compromise the mechanical properties of the material.
Another step in the process to reduce free radicals and oxidation is thermal stabilization, or heating. In the production of polyethylenes, various commercial companies use different types of radiation, radiation doses, and methods of stabilization, machining, and terminal sterilization.
Wear is termed linear wear (femoral head penetration into the liner), and volumetric wear (amount of material lost). Linear wear is assessed in clinical studies, and volumetric wear in laboratory studies. Osteolysis has a higher propensity to occur with linear wear greater than 0.10 mm/yr and volumetric wear greater than 80 mm
3/yr.
4 Laboratory simulator studies done prior to commercial release demonstrated less wear for XPE compared with CP.
5-11 Those in-vitro wear studies also demonstrated that with XPE, the degree of wear that occurs is not related to the size of the prosthetic femoral head selected, nor to the initial thickness of the polyethylene liner. (The importance of this characteristic will become clear in a discussion below.)
XPE was introduced into clinical practice in 1999 with the expectation that lower wear rates in-vitro would translate to lower wear rates in vivo. Two randomized clinical studies followed patients for five years after total hip arthroplasties with XPE or CP.
12 Both studies concluded that, compared with CP, XPE had significantly fewer penetrations of the liner by the femoral head. The wear rate for XPE decreased by more 95% compared with the wear rates for CP, and tended to plateau after one year.
Another study found that five years after total hip arthroplasty there was significantly less osteolysis on CT scan with XPE compared with CP (28% versus 80%).
13 Multiple other studies have since confirmed a reduction in wear rates for XPE compared with CP, which has translated into less osteolysis and aseptic loosening in total hip arthroplasties with XPE.
FEMORAL HEAD AND ACETABULAR LINER BEARINGS
Cobalt-Chromium & Crossed Linked Polyethylene (XPE)
The most common femoral head composition used in total hip arthroplasty is made of a cobalt-chromium (CoCr) metal alloy. As a result, the most widely used combinations in the U.S. are metal-on-polyethylene bearings (Fig.3), and most studies that compared CP to XPE wear used CoCr femoral heads. In 2013, the Swedish registry detected a trend toward fewer cup/liner revisions with the use of XPE, compared with an increase in the previous years when CP was used.
14 In 2014, the Australian arthroplasty registry also noted that, as time progressed, there was a lower revision rate with XPE compared with CP.
15
In high risk patients, larger femoral heads are used sometimes to decrease the risk of impingement of the femoral head or neck of the femoral prosthesis on the edge of the acetabulum or polyethylene liner. These contacts may produce a lever arm that causes a dislocation. To accommodate the larger femoral head, a thinner polyethylene liner would be needed, but as noted earlier, multiple studies have demonstrated that for XPE, thickness of the polyethylene liner does not affect the wear rate. A thinner XPE cup might also raise concern about fracture, but this also has not been an issue except in those acetabular cups placed more vertically, anteverted, or with a rim thickness at the locking mechanism < 4 mm.
Since most non-cemented femoral prostheses are constructed of titanium, there has been concern recently about the bearing coupling between the CoCr femoral head and the titanium femoral prosthesis. This mixed metal construct may increase the risk of fretting
** and corrosion at the modular junction, a process termed trunnionosis (Fig. 4). (The trunnion is the tapered portion of the femoral stem prosthesis where the femoral head is impacted during implantation.)

Fig. 4 Example of trunnionosis of a cobalt chromium femoral
head and the tapered portion of the femoral prosthesis.
With CoCr femoral heads, there have been reports of corrosion at the trunnion, metal wear at the trunnion, and adverse local tissue reactions from the metal debris. As a result, it has been proposed that ceramic femoral heads be used to avoid these reactions. However, registries have not reflected a statistically significant difference in revision rates between ceramic or CoCr femoral heads with XPE liners. Also, ceramic femoral heads typically are significantly more expensive than CoCr femoral heads and may not be cost effective.
Studies have also revealed that XPE liners are more tolerant of acetabular component malposition. Together with the low wear characteristics of XPE, the cheaper cost of CoCr femoral heads, and the ability of metal-on-XPE bearings to withstand minor malposition, CoCr-XPE bearings should be the predominant couple in current total hip arthroplasties.
Ceramic Bearings
Ceramic bearings were first used in clinical practice in the 1970s. The ceramic components are fabricated from pure alumina, zirconia, and alumina matrix composite powder. In total joint replacement, ceramic constructs are available for both the femoral head and the acetabular liner. Ceramic constructs have stronger mechanical properties and lower wear rates.
16,17 Their hard structures and smoothly polished surfaces provide higher resistance to wear, and minimize frictional forces because of their hydrophilic properties.
18
Not only do ceramic-on-ceramic constructs have the lowest wear rate amongst all bearings, but they also cause less soft tissue reactions when compared to metal-on-polyethylene and metal-on-metal bearings.
19 Because a ceramic component is not a metal alloy, there is less trunnionosis with the combination of a ceramic femoral head and a titanium femoral prosthesis, and less chance for metal debris and damage to the titanium trunnion. Also, the lack of metal debris makes ceramic femoral heads beneficial in patients with metal hypersensitivity.
In-vivo studies have demonstrated excellent wear rates over a 10-year period for both ceramic-on-polyethylene,
20-24 and ceramic-on-ceramic bearings,
21-22,
25-29 with no statistically significant difference in osteolysis, wear rates, or implant failure.
22-24
Nonetheless, first-generation ceramic components had higher rates of component fracture than XPE liners with CoCr femoral heads. Fracture is catastrophic because it results in multiple fragments that may lead to third body wear and damage of the femoral prosthesis. Fortunately, the newest generation of mixed oxide ceramic materials has greatly reduced the risk of fracture to roughly 0.003% and 0.03% for Delta ceramic heads and liners, respectively.
30
The various factors that influence the risk of ceramic femoral head fractures include the cleanliness of the trunnion prior to head impaction, the amount of force used to impact the head on the trunnion, and the size and length of the femoral head. (Smaller heads and shorter necks have a higher risk of fracture.)
Ceramic-on-ceramic hip constructs are also associated with increased squeaking. The Australian National Joint Registry noted a 4.2% rate of squeaking with this construct.
31 Squeaking can occur with every step, or with deep flexion, and is likely caused by malposition of the acetabular component with excessive inclination and anteversion. Squeaking may also occur with the loss of the fluid film lubricating the joint. Component malposition is also a factor, as it may result in increased loading against the edge of the cup. Care must be taken to avoid this complication because it may produce embarrassment and anxiety for the patient, and litigation against the surgeon. There is no clear evidence that squeaking increases the wear rate of the implant, though there are suggestions that it may. In addition, ceramic heads have traditionally been significantly more expensive than CoCr, and their cost effectiveness is debatable.
Ceramicized Femoral Heads
Zirconium is a hard metal with properties like titanium. It is not found naturally as a metal, but can be refined, through a complex process, from zirconium silicate (ZrSiO4). However, Zirconium oxide (ZrO2) is not a metal but a ceramic. It was first used clinically in total hip arthroplasties in approximately 2003 as a zirconium oxide, ceramic, outer surface of approximately 5 μm on a zirconium metal femoral head (Fig. 5).

Fig. 5 Acetabular cup with highly crossed-linked polyethylene liner and ceramicized femoral head.
This ceramic outer surface has similar mechanical properties to a fully ceramic bearing, including a smooth surface, increased scratch resistance, and increased hardness when compared to CoCr. In vitro studies confirm that ceramicized zirconium femoral heads share the improved resistance to wear of fully ceramic heads with polyethylene, especially with XPE.
32 The Australian Joint Registry reported a low revision rate of 3.3% at 11 years with this bearing couple.
33 However, in-vivo studies vary when comparing XPE with CoCr or ceramicized heads. Some studies show statistically significant differences in wear rate, and others demonstrate no difference.
34-36
Because of its zirconium alloy core, this composite will not fracture like fully ceramic heads. However, the oxide surface may be damaged if it contacts other metal surfaces, such as the rim of the acetabular metal shell during joint reductions and dislocations. Ceramicized femoral heads also have a higher resistance to fretting and corrosion of the trunnion compared to CoCr, so they may be a suitable option if there is concern about trunnionosis. Like ceramic heads, ceramicized heads are also a viable option in patients with metal hypersensitivity since they avoid metal debris and trunnionosis at the bearing junction.
Like the all-ceramic heads, however, ceramicized heads are significantly more expensive than CoCr femoral heads. Also, only one company currently manufactures this product, and it should therefore only be used with this company’s compatible femoral prosthesis.
In sum, ceramicized heads are a good option because of their improved wear characteristics and good in-vivo results, but their increased cost, and production by only one manufacturer, limits their widespread use.
METAL-ON-METAL FEMORAL HEAD AND LINER
As discussed throughout this article, a primary concern in total hip replacements is the wear rates of bearing materials. A metal-on-metal (MoM) bearing includes a CoCr metal head and a metal acetabular liner. (Fig. 6)

Fig. 6. Metal-on-metal hip prosthesis with femoral stem, cobalt chromium femoral head,
metal liner, and metal acetabular cup.
Traditional stemmed MoM hip replacements (and later resurfacings) were first introduced in the 1990s because they offered lower wear rates. For younger patients who need total hip replacement for osteoarthritis, longevity of the implant is a particularly important characteristic. It is estimated that since 1996, more than 1 million MoM implants have been inserted worldwide. MoM bearings can result from traditional hip replacement with a stemmed femoral prosthesis (Fig. 7B), or resurfacing of the femoral head with a metal cap (Fig. 7A), in which case more bone is preserved.

Fig. 7. Radiographs of metal-on-metal prosthesis.
A: Hip resurfacing prosthesis;
B: Stemmed metal-on-metal total hip replacement.
The benefits of MoM bearings compared with metal-on-polyethylene include not only lower volumetric wear rates, but also greater stability of the implant; because metal inserts are thinner than polyethylene liners, larger femoral head sizes can be used.
However, the use of MoM bearings in stemmed hip replacements is not recommended in the U.S. because there are reports in the literature of poor outcomes. When MoM bearings are inserted in patients who are more than 55 years old, have larger femoral heads, or have acetabular cups placed in excessive inclination, they have a higher risk of revision than polyethylene and ceramic bearings.
36-38
Soft tissue reactions from the metal ions of the MoM bearings are the key issues in failure of the implants and associated complications. The metal ions cause adverse local tissue reactions (ALTRs), osteolysis, enlarged bursae, effusions, creation of pseudotumors, destruction of the abductor muscles, and necrosis. (Fig. 8)
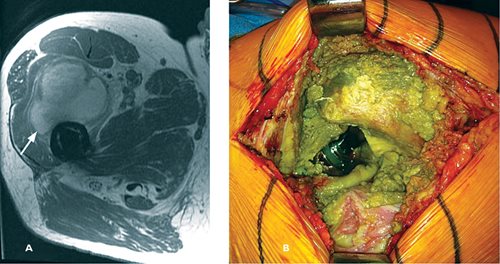
Fig. 8.
A: MARS MRI axial image with pseudotumor (arrow) anterior to the femur and metal-on-metal prosthesis;
B: Intraoperative image of previous metal-on-metal prosthesis causing extensive metallosis and soft tissue destruction.
A lymphocyte dominated immunologic response occurs in the tissue, known as aseptic lymphocyte-dominant vasculitis-associated lesions (ALVAL).
Unfortunately, it is not possible to predict which patients will have these reactions to metal ions. Some patients have symptoms, others have none, but it is generally recommended that even asymptomatic patients should be evaluated yearly with radiographs to assess osteolysis and blood levels of cobalt and chromium ions. Metal ion levels > 7 ppb (parts per billion) are considered elevated, and should instigate advanced imaging. Metal artifact reduction sequence (MARS) MRI helps assess for presence of pseudotumors and integrity of the abductor and gluteal muscles.
Optimum treatment of asymptomatic patients is debated. Treatment of symptomatic patients is multi-factorial but commonly involves a revision total hip replacement. Placement of metal-on-polyethylene or ceramic-on-polyethylene bearing constructs are generally recommended for stable acetabular and femoral prostheses.
Many companies have recalled their MoM stemmed hip replacements because of these unfavorable outcomes. Therefore, hip resurfacing is the only recommended MoM bearing, and should be reserved for younger patients with preserved femoral head bone stock. However, this operation is not typically performed by most orthopedic surgeons.
CONCLUSION
Substantial progress has been made in the bearing components of total hip replacements in the past 30 years. Newer highly crossed-link polyethylene liners have significantly decreased wear rates when compared with conventional polyethylene. Cobalt chromium femoral heads and highly crossed linked polyethylene liners are the dominant bearing couple used in the United States, due to excellent follow-up studies. Ceramic and ceramicized femoral heads have lower wear rates, but they are more costly. They may be viable options in younger patients, and those with metal hypersensitivities. Stemmed metal-on-metal hip replacements have largely been removed from the U.S. market due to post-operative complications, and the need for revision surgery. The ultimate goal will be to create a bearing couple with minimal complications and increased durability.
* Gy = Gray, the International Unit of absorbed ionizing radiation. It is derived from the applied energy (in Joules) and the mass of the affected matter (in Kg). kGy = thousands of units.
** Fretting: A special wear process that occurs at the contact area between two materials under load that are subjected to relative motion by vibration or some other force.
REFERENCES
1. Wolford M, Palso K, Bercovitz A: Hospitalization for total hip replacement among inpatients aged 45 and over: United States, 2000-2010. Centers for Disease Control and Prevention
https://www.cdc.gov/nchs/data/databriefs/db186.htm
2. Kurtz S, Ong K, Lau E, et al: Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 2007;89(4):780-785.
3. Depuy Pinnacle Polethylene technique guide:
http://synthes.vo.llnwd.net/o16/LLNWMB8/US%20Mobile/Synthes%20North%20America/Product%20Support%20Materials/Technique%20Guides/DSUSJRC04140026(2)%20Pinnacle%20ST.pdf
4. Hammerberg EM, Wan Z, Dastane M, et al: Wear and range of motion of different femoral head sizes. J Arthroplasty 2010;25(6):839-843.
5. Estok DM II, Burrough BR, Muratoglu OK, et al: Comparison of hip simulator wear of 2 different highly crossed-linked ultra high molecular weight polyethylene acetabular components using both 32- and 38-mm femoral heads. J Arthroplasty 2007;22(4):581-589.
6. Muratoglu OK, Rubash HE, Bragdon CR, et al: Simulated normal gait wear testing of a highly crossed-linked polyethylene tibial insert. J Arthroplasty 2007;22(3):435-444.
7. Laurent MP, Johnson TS, Crowninshielf RD, et al: Characterization of a highly crossed-linked ultrahigh molecular-weight polyethylene in clinical use in total hip arthroplasty. J Arthroplasty 2008;23(5):751-761.
8. Ito H, Maloney CM, Crowninshield RD, et al. In vivo femoral head damage and its effect on polyethylene wear. J Arthroplasty 2010; 25(2): 302-308.
9. Shen FW, Lu Z, McKellop HA: Wear versus thickness and other features of 5 MRAD crosslinked UHMWPE acetabular liners. Clin Orthop Relat Res 2011; 469(2): 395-404.
10. McKellop H, Shen FW, DiMaio W, et al. Wear of gamma-crosslinked polyethylene acetabular cups against roughened femoral balls. Clin Orthop Relat Res 1999; 3369:73-82.
11. McKellop HA, Shen FW, Lu B, et al. Effect of sterilization method and other modifications of the wear resistance of acetabular cups made of ultra-high molecular weight polyethylene: A hip simulator study. J Bone Joint Surg Am 2007;89 (10):2212-2217.
12. Digas G, Karrholm J, Thanner J, et al. 5-year experience of highly crossed-linked polyethylene in cemented and uncemented sockets: Two randomized studies using radiostereometric analysis. Acta Orthop 2007;78(6):746-754.
13. Leung SB, Egawa H, Stepniewski A, et al. Incidence and volume of pelvic osteolysis at early follow-up with highly crossed-linked and noncross-linked polyethylene. J Arthroplasty 2007;22(6, Suppl 2):134-139
14. Swedish Hip Arthroplasty Register: Annual Report 2013.
https://registercentrum.blob.core.windows.net/shpr/r/Annual-report-2013-HJnnK8Tie.pdf
15. Australian Orthopaedic Association: National joint replacement registry annual report 2014.
https://aoanjrr.sahmri.com/en/annual-reports-2014 Accessed on 6/25/18
16. Campbell P, Shen FW, McKellop H: Biologic and tribologic considerations of alternative bearing surfaces. Clin Orthop Relat Res 2004;418:98-111.
17. Macdonald N, Bankes M: Ceramic on ceramic hip prostheses: A review of past and modern materials. Arch Orthop Trauma Surg 2014;134(9):1325-1333.
18. Di Puccio F, Mattei L: Biotribology of artificial hip joints. World J Orthop 2015;6 (1):77-94.
19. Esposito C, Maclean F, Campbell P, et al. Periprosthetic tissues from third generation alumina-on-alumina total hip arthroplasties. J Arthroplasty 2013;28(5):860-866.
20. So K, Goto K, Kuroda Y, et al. Minimum 10-year wear analysis of highly cross-linked polyethylene in cementless total hip arthroplasty. J Arthroplasty 2015; 30(12):2224-2226.
21. Epinette JA, Manley MT: No differences found in bearing related hip survivorship at 10-12 years follow-up between patients with ceramic on highly cross- linked polyethylene bearings compared to patients with ceramic on ceramic bearings. J Arthroplasty 2014;29(7): 1369-1372.
22. Kim YH, Park JW, Kulkarni SS, et al. A randomised prospective evaluation of ceramic-on-ceramic and ceramic-on-highly cross-linked polyethylene bearings in the same patients with primary cementless total hip arthroplasty. Int Orthop 2013;37(11): 2131-2137.
23. Nakashima Y, Sato T, Yamamoto T, et al. Results at a minimum of 10 years of follow- up for AMS and PerFix HA-coated cementless total hip arthroplasty: Impact of cross-linked polyethylene on implant longevity. J Orthop Sci 2013;18(6): 962-968.
24. Fukui K, Kaneuji A, Sugimori T, et al. Wear comparison between conventional and highly cross-linked polyethylene against a zirconia head: A concise follow-up, at an average 10 years, of a previous report. J Arthroplasty 2013; 28(9):1654-1658.
25. Chana R, Facek M, Tilley S, et al. Ceramic-on-ceramic bearings in young patients: Outcomes and activity levels at minimum ten-year follow-up. Bone Joint J 2013;95-B(12): 1603-1609.
26. Synder M, Drobniewski M, Sibinski M: Long-term results of cementless hip arthroplasty with ceramic-on-ceramic articulation. Int Orthop 2012;36(11): 2225-2229.
27. Streit MR, Schröder K, Körber M, et al. High survival in young patients using a second generation uncemented total hip replacement. Int Orthop 2012;36(6): 1129-1136.
28. Solarino G, Piazzolla A, Notarnicola A, et al.Long-term results of 32-mm alumina- on-alumina THA for avascular necrosis of the femoral head. J Orthop Traumatol 2012;13(1):21-27.
29. Sugano N, Takao M, Sakai T, et al. Eleven- to 14-year follow-up results of cementless total hip arthroplasty using a third-generation alumina ceramic-on-ceramic bearing. J Arthroplasty 2012;27(5):736-741.
30. Massin P, Lopes R, Masson B, et al. French Hip & Knee Society (SFHG): Does Biolox Delta ceramic reduce the rate of component fractures in total hip replacement? Orthop Traumatol Surg Res 2014;100(6 suppl):S317-S321.
31. Own Dh, Russell NC, Smith PN, et al, An estimation of the incidence of squeaking and revision surgery for squeaking in ceramic-on-ceramic total hip replacement: A meta-analysis and report from the Australian Orthopaedic Association National Joint Registry. Bone Joint J 2014;96-B(2):181-187.
32. Good V, Ries M, Barrack RL, et al. Reduced wear with oxidized zirconium femoral heads. J Bone Joint Surg Am 2003;85-A(suppl 4):105-110.
33. Australian Orthopaedic Association: National joint registry annual report 2015.
https://aoanjrr.sahmri.com/en/annual-reports-2015 Accessed 6/27/18
34. Morison ZA, Patil S, Khan HA, et al. A randomized controlled trial comparing Oxinium and cobalt-chrome on standard and cross-linked polyethylene. J Arthroplasty 2014;29(9suppl):164-168.
35. Jassim SS, Patel S, Wardle N: Five-year comparison of wear using oxidized zirconium and cobalt-chrome femoral heads in total hip arthroplasty: A multicenter randomized controlled trial. Bone Joint J 2015;97-B(7):883-889.
36. Karidakis GK, Karachalios T: Oxidized zirconium head on crosslinked polyethylene liner in total hip arthroplasty: A 7- to 12-year in vivo comparative wear study. Clin Orthop Relat Res 2015;473(12):3836-3845.
37. Australian Orthopaedic Association: National joint registry annual report 2010.
https://aoanjrr.sahmri.com/en/annual-reports-2010
38. National Joint Registry for England and Wales: Seventh Annual Report. 2010.
http://www.njrcentre.org.uk/NjrCentre/Portals/0/NJR%207th%20Annual%20Report%202010.pdf