
Winter 2017 - Vol. 12, No. 4
PERSPECTIVES
Firearm Violence
A Local, State and National Scourge
Chet A. Morrison, M.D., FACS, FCCM
Medical Director, Trauma/Neuro Critical Care
Lancaster General Health/Penn Medicine
Adjunct Associate Professor of Surgery, University of Pennsylvania
INTRODUCTION
Firearm violence (injury and death related to firearms) has become a major American scourge that causes tremendous suffering, but although mass shootings are increasingly frequent
1 and command the public’s attention, these highly visible atrocities account for only a small percentage of the total burden of injuries or deaths related to guns.
In 2015, the last full year for which U.S. data are available, gunfire violence accounted for 35,476 deaths in a population of 321,418,820, for a crude death rate of 11.04/100,000, and an age adjusted rate of 10.77/100,000.
2 The death rate for firearm violence has surpassed that for motor vehicle collisions, largely because driving a car has become markedly safer in recent years, while owning a firearm has not. (Fig. 1)
Fig. 1.
Yearly Death Rates for Firearm Injuries and Motor Vehicle Accidents
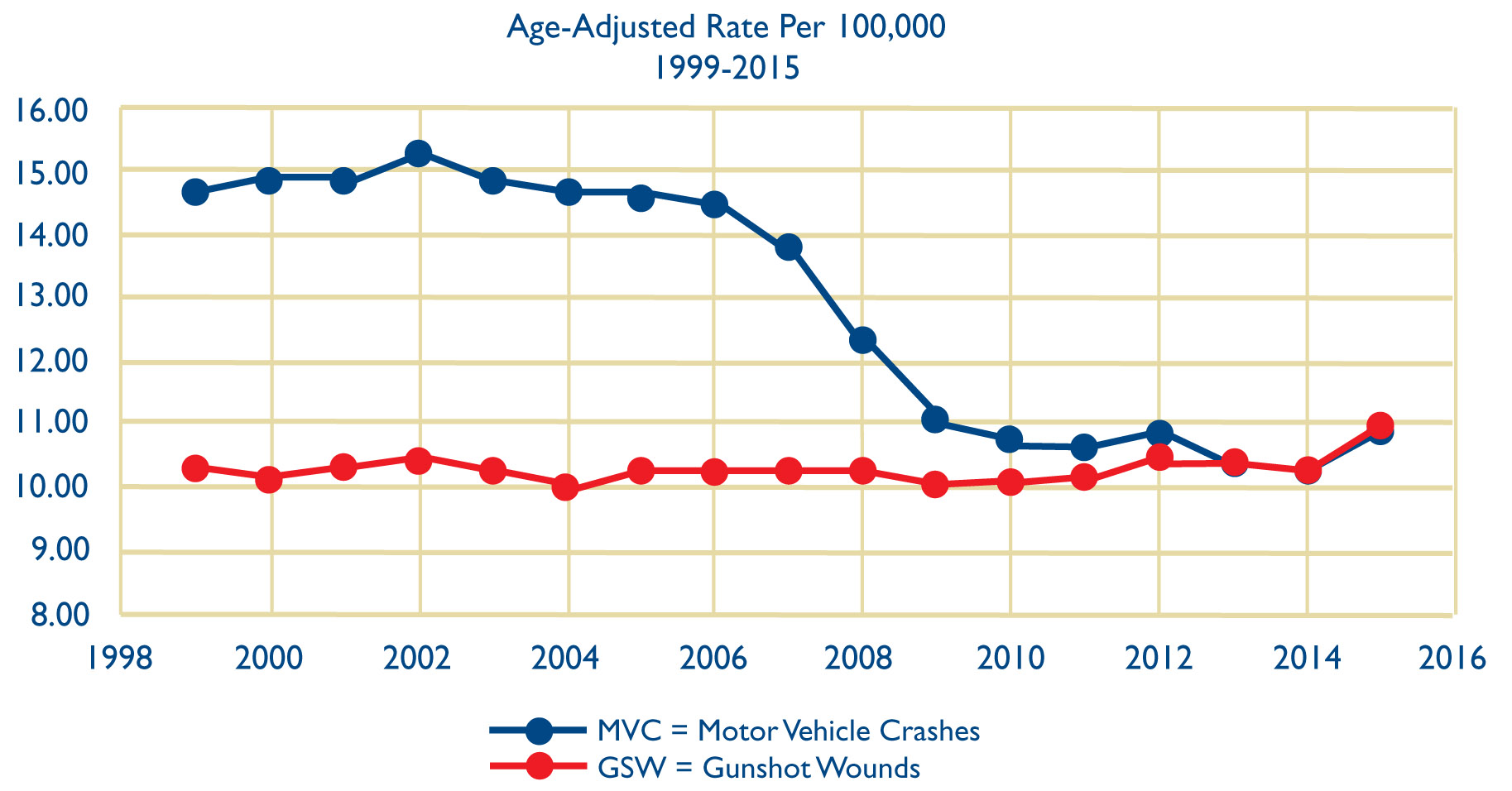 Source: CDC National Center for Health Statistics, 1999-2015
Source: CDC National Center for Health Statistics, 1999-2015
It should also be kept in mind that close to two thirds of all gunfire deaths are suicides – 22,018 of the total of 35,476 deaths in 2015.
2 Despite this set of grim statistics, and widespread public awareness, firearm policy remains stagnant; as of this writing our elected leaders have not introduced any gun control initiatives to curb this epidemic.
The trauma community has long been focused on these policy issues, because we must treat these unfortunate patients and their families. Indeed, one of the major efforts of the trauma community is to teach first responders and the general public the simple methods that are effective in controlling hemorrhage at the scene of a shooting. We do so because we presume these horrific events will continue, just as we teach basic life support because we assume that people will continue to have acute coronary events.
3 Lancaster General Health actively participates in this effort as the county trauma center, and as a Level 2 center accredited by the Pennsylvania Trauma System Foundation. We educate members of the public, our law enforcement officers, our EMTs and paramedics, and other first responders, about simple techniques to control bleeding, and other actions that are potentially lifesaving.
Surprisingly, for a public health issue of this magnitude there is a lack of reliable data, and little funding for research that would clarify the real scope of the problem and suggest ways to improve it. This is likely due, at least in part, to the Dickey amendment, named after the congressman who proposed it in 1996, which
specifically directs the Centers for Disease Control not to do research advocating or promoting gun control; it was extended to other government health care agencies in 2011 by the new Republican Congress.
4 But, as mass shootings have increased, the trauma centers that care for such patients have prompted renewed interest in this topic. Unfortunately, the data are not reassuring; several centers report no decline, or even significantly increased mortality over the past decade, which is thought to be due to increased lethality of the injuries they see, and possibly increased frequency of multiply wounded patients.
5,6
GUNFIRE VIOLENCE IN LANCASTER
Lancaster County, despite its semi-rural status and below average crime incidence, is not immune to gunfire violence and injury. Recent work by our group in the LGH Trauma Department showed that Lancaster General Health, the county trauma center where presumably the vast majority of gunshot victims are brought for care, averages 30 to 40 patients per year for the entire population, with a mortality rate of 15% (71 deaths per 478 GSW victims).
7 There was no change in these statistics over the study period from January 2000 to December 2013 (21% in 2000 to 21% in 2013; p=0.973). (Fig. 2)
Fig. 2.
Mortality Rate for Gunshot Wounds Brought to Lancaster General Hospital (Including Pronounced Dead on Arrival)
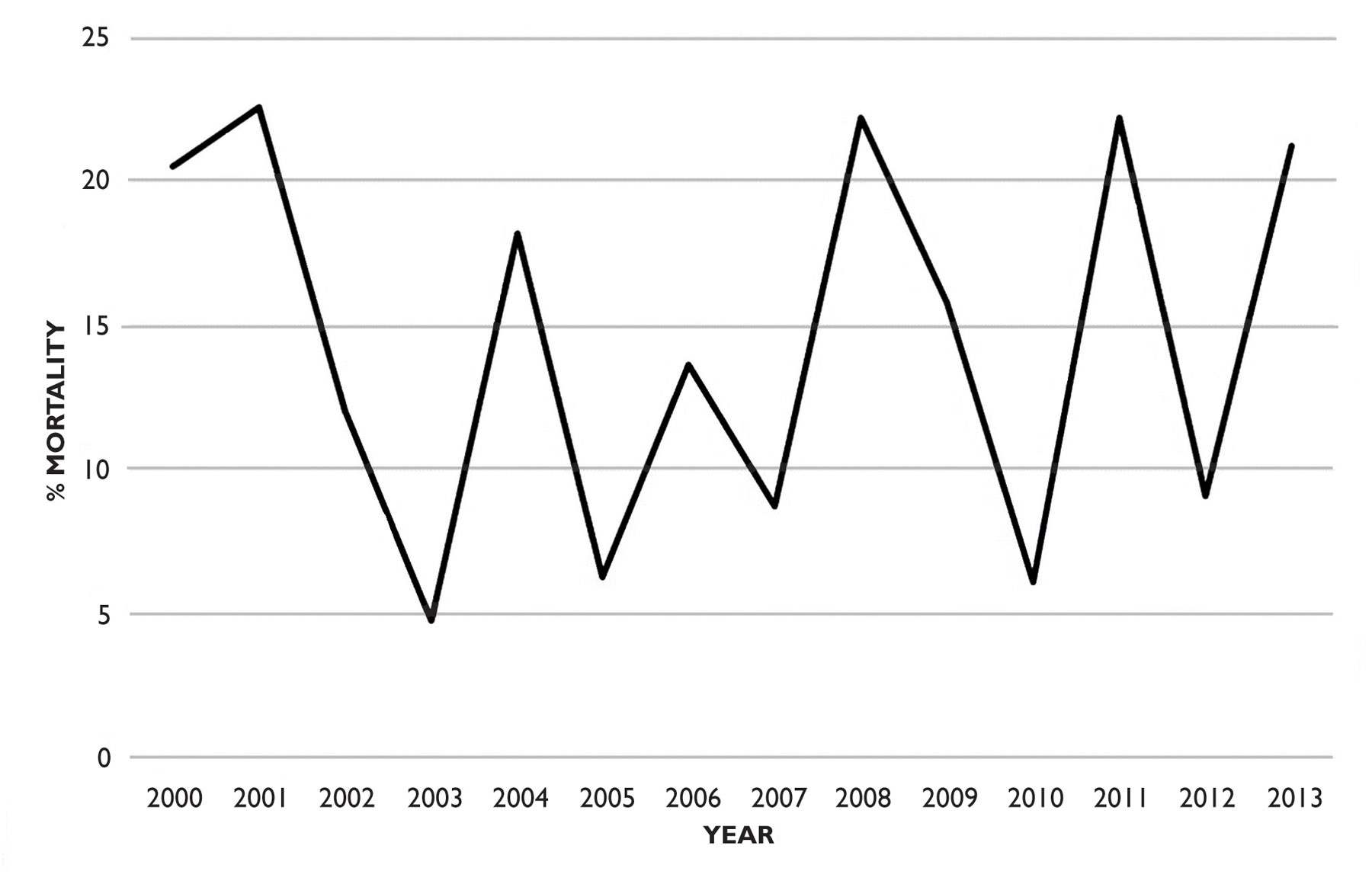 Source: Morrison, J Surg Res. 2015 Nov:199(1):190-6
Source: Morrison, J Surg Res. 2015 Nov:199(1):190-6
In the last calendar year, we admitted 31 GSW patients with one fatality. This statistic includes patients we pronounce dead on arrival, but it does not account for those who are pronounced dead at the scene (the city of Lancaster has recorded four to seven homicides annually for the past five years). Thus, Lancaster County, although spared the horrific ongoing levels of violence seen in major urban centers, has an endemic rate of gun violence that seems to change very little from year to year.
GUNFIRE VIOLENCE IN PENNSYLVANIA
Although the overall violent crime rate has declined significantly in Pennsylvania during the past five years,
8 gunfire is still a scourge on the state level as well. When our group analyzed data statewide, we found that 19,342 patients were admitted to the hospital with gunshot injuries from 2003 to 2015, averaging 1,488 per year, with little variation from year to year.
9 The total number was 1,278 in 2003, for example, and 1,672 in 2006. Dishearteningly, adjusted mortality from these injuries did not change over time, despite advances in resuscitation and critical care. Of all homicides in Pennsylvania, firearms accounted for 78%, and a handgun was used in 59%. Data from the CDC show that Pennsylvania has an age-adjusted death rate from firearms of 10.5 per 10,000 residents, which places it in the midpoint of states (2). In 2015, for example, 1,485 people were killed by firearms.
Pennsylvania, a state with a mixed urban and rural population, has relatively few legal restrictions on gun ownership, and the restrictions have lessened over time with passage of the “stand your ground legislation” in 2011,
10 as well as a recent bill designed to expose municipalities to lawsuits over restricting rights of gun ownership and gun carrying.
11 Consistent with the national trend, our violence tends to cluster in relatively high crime areas, as has been shown in data from New Jersey data and Philadelphia.
12
GUNFIRE VIOLENCE AT THE NATIONAL LEVEL
As indicated in the introduction, the burden of gunfire injury at the national level is striking. Of all injury-related deaths in the United States, 17% are caused by firearms, making them the third leading cause behind only poisoning and motor vehicle crashes.
13,14 The clinical burden of non-fatal firearm-related injuries is estimated to be approximately three times that of fatal injuries. The injury burden has a reported incidence of over 700,000 ED visits per year, resulting in mean per person ED and inpatient charges of $5,254 and $95,887, respectively, yielding an annual cost of approximately $2.8 billion.
15
Interestingly, whereas roughly two thirds of
deaths in this extensive survey were suicidal, only 5% of
injuries were the result of attempted suicide – half intentional, and the rest accidental. But these suicide attempts had a strikingly higher mortality than assaults or injuries. (Fig. 3)
Fig. 3.
Percentages of Emergency Department (ED) or Inpatient Mortality by Selected Characteristics Among Patients Who Reached the ED Alive After a Firearm-Related Injury
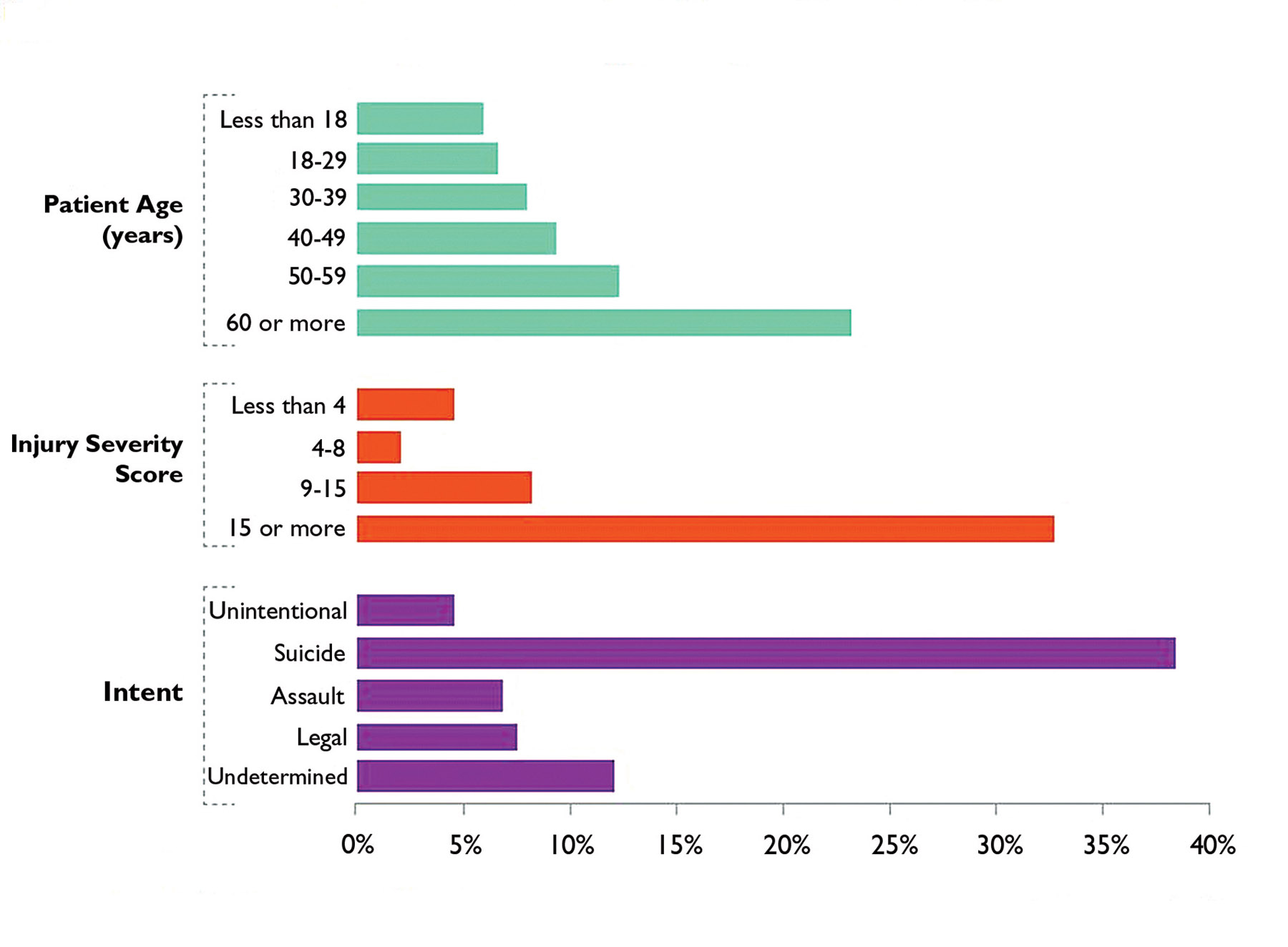 Source: Faiz Gani et al. Health Aff 2017;36:1729-1738. Authors' analysis of data for 2006-2014 from the Nationwide Emergency Department Sample. "Legal" refers to injuries incurred during legal interventions.
Source: Faiz Gani et al. Health Aff 2017;36:1729-1738. Authors' analysis of data for 2006-2014 from the Nationwide Emergency Department Sample. "Legal" refers to injuries incurred during legal interventions.
It is worth mentioning that many patients arrive with nonsurvivable injuries, particularly those with gunshot wounds to the head, which have 91% mortality rate.
16 It is also important to note that several studies have documented increased rates of firearm injury and death when access to guns was liberalized and concealed carry was permitted.
17,18
ATTITUDE OF PROVIDERS TO GUNS AND GUNFIRE VIOLENCE
Most providers understand the magnitude of the scourge of gunfire injury, but the medical community is comprised of diverse and strong-willed individuals, and their attitudes mirror the controversy in society at large; they agree on many aspects of the problem, and disagree on others. Recently, members of the American College of Surgeons Committee on Trauma (who are representative of the leaders of trauma care in the country) were surveyed about their attitudes toward various methods of prevention of gunfire violence. There was strong support for conducting mandatory background checks, preventing people with mental illness from obtaining guns, limiting civilian access to assault rifles and high capacity magazines, and requiring features that promote gun safety, including child proof locks and “smart gun” technology.
19 Interestingly, a substantial percentage of these physicians were firearm owners, and there was notably less support of these measures among these firearm owners, though they rarely voiced strong opposition. In an interesting side note, the lead author of the study, Dr. Deb Kulhs, is a personal friend of mine, and was one of the trauma surgeons called upon to respond to the recent horrific incident in Las Vegas. Similar results were found in a survey of the Board of Governors of the American College of Surgeons.
20
GUNFIRE VIOLENCE: A WAY FORWARD
While the magnitude of the problem reflects the many differing viewpoints and vested interests in American society, I believe clinicians are uniquely qualified advocates on this issue. We can provide data, agitate to diminish the lethality of weapons that are available to the public, and focus on firearm safety. Indeed, various professional medical groups have issued statements and offered strategies that address this problem. As an example, The American College of Surgeons Committee on Trauma recently released a consensus statement that detailed a strategy aimed at reducing death and disability from firearm injuries, which is built on a trauma system/public health model.
21
The ACS strategy offers some approaches that are currently being tried, as well as a plan for future efforts:
1) Prevent injuries by offering firearm injury and violence prevention programs. Trauma centers are uniquely qualified to offer these programs to the community; to support reasonable firearm regulations; to advocate for firearm safety; and to enhance gun safety programs for those who own firearms.
2) Increase the likelihood of immediate bleeding control at the scene of injury
before emergency medical professionals arrive, by turning bystanders into immediate responders through the proliferation of Stop the Bleed
® and www.bleedingcontrol.org and by providing support for Emergency Medical Services. As mentioned above, LGH is partnering in these efforts. No one should die from exsanguinating hemorrhage if it is controllable by application of direct pressure or tourniquets. Along with this initiative, we should ensure the delivery of rapid and effective on-site medical care with bleeding control from our EMT first responders
3) Our trauma centers have made significant advances in the care of wounded patients, often in collaboration with our military partners. A good example of such advances is the current concept of balanced resuscitation with liberal use of blood products, with perhaps even the return of using whole blood for fluid resuscitation with relatively restricted administration of IV crystalloids. Such efforts should be sustained by vigorous research and continuation of certification of trauma centers at the state and national level.
4) Promote robust rehabilitation and reintegration programs for injured patients that minimize disability. Gunfire injuries represent a significant loss of productivity and quality-adjusted life years, and can result in substantial long-term disability. In my opinion, these efforts should be integrated into a robust health care system that provides quality accessible health care to all. Since it is often the most economically vulnerable people who are injured by guns, reducing their disability would improve their reintegration into society as productive citizens.
THREE PROPOSALS TO ALLEVIATE GUN VIOLENCE
First is a recommendation for legislation to limit the lethality and firepower of weapons that are sold to the general public. It is perhaps a truism that if there were no rapid fire and high capacity weapons available, they would not be used for mass shooting events, but there are data that make this statement more than a tautology. In 1996, after a mass shooting that killed 35 people (the Port Arthur Massacre), Australia introduced extensive gun law reform that included a ban on highly lethal weapons that are not used in hunting, such as semiautomatic rifles. Since then,
there have been no fatal mass shootings in Australia.
22 Furthermore, between 1997 and 2013 firearm deaths fell from 3.6/100,000 persons to 1.2/100,000, a decline that was more rapid than before 1997. Interestingly, after gun law reform firearm suicides declined more rapidly than homicides, with no evidence that suicidal people simply substituted other techniques. (Fig. 4)
Fig. 4.
Suicide and Homicide Death Rates According to Firearm Involvement 1979-2013
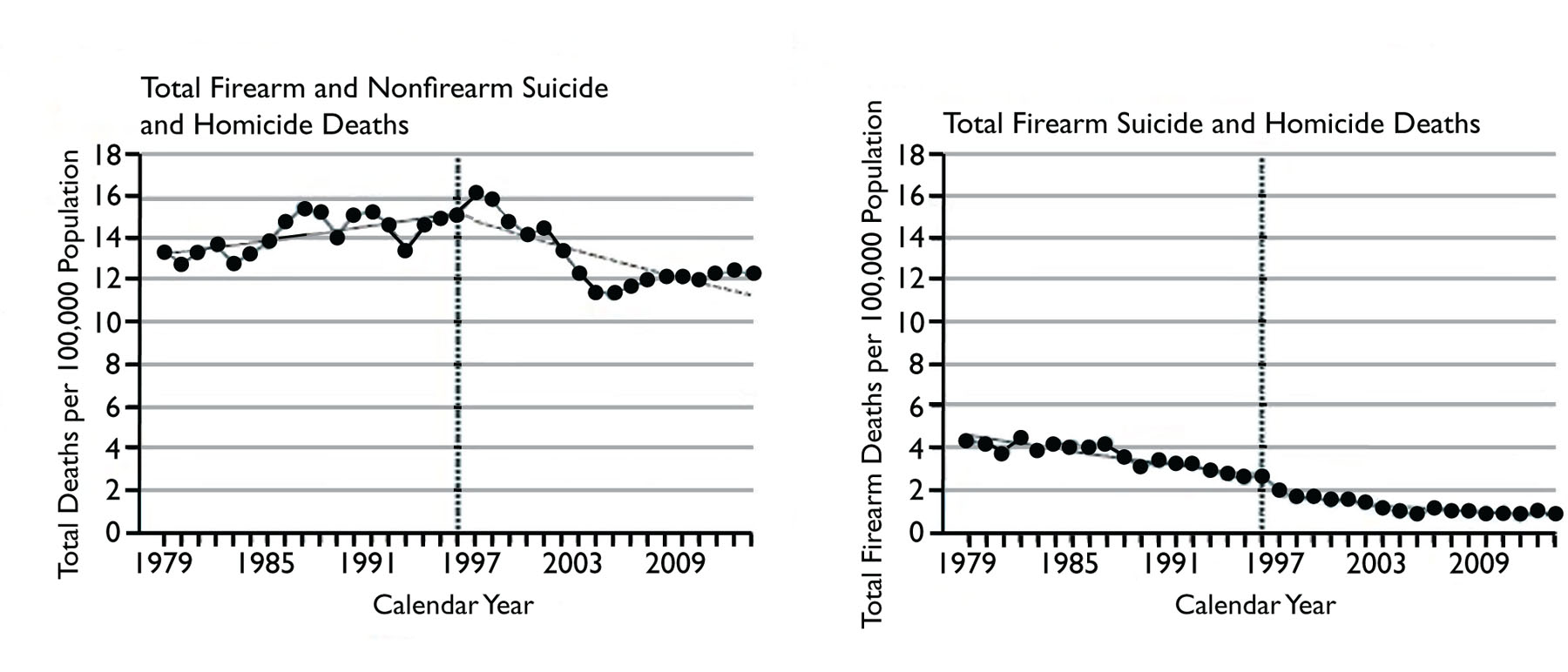 Source: Chapman S, Alpers P; Jones M. Association Between Gun Law Reforms and Intentional Firearm Deaths in Australia, 1979-2013 JAMA 2016,316(3):291-299
Source: Chapman S, Alpers P; Jones M. Association Between Gun Law Reforms and Intentional Firearm Deaths in Australia, 1979-2013 JAMA 2016,316(3):291-299
While the Australian approach is probably not politically feasible in the United States at this time, it does raise the possibility that firearm regulation here can perhaps be synergistic with renewed efforts in mental health care to decrease our firearm suicide rate. In terms of what is feasible, very recent data presented at a major national trauma meeting indicate a decrease in firearm related fatalities and hospital utilization when a state banned open carry of an unloaded firearm, having long since banned open carry of loaded firearms.
23 Even this seemingly trivial adjustment to the law was followed by a lower incidence of firearm-related fatalities and nonfatal incidents, independent of other factors. Conversely, and perhaps controversially, laws which make it easier to obtain firearms have been shown to lead to an increase in fatalities.
24 As one researcher put it: “We found that making it easier to kill people resulted in more dead people.”
25
Second, far more research and innovation need to be done to guide public policy, to inform the public, and possibly to make firearms safer and less likely to be used in a crime. It might surprise people to learn, for example, that owning a firearm does not make them less likely to be murdered. In fact, the data we have seem to indicate that a firearm places people at increased risk of dying by gunfire.
25
Finally, we should continuously strive to translate these findings into robust public education and advocacy efforts in a non-political way. Like other public health issues, gun violence should ideally be viewed as a public health problem. As such, management of the problem should include attempts to alleviate not only mental health problems, but also difficulties with access to the health care system in general, and persistent poverty and crime in the inner city where violence is endemic.
Considering all the different aspects of this public scourge it is easy to succumb to a kind of nihilistic fatalism given the lethality of the injuries, the intractable societal problems, and the seeming immovability of public policy and public opinion on the issue. The horrifying events in Orlando and Las Vegas support that attitude, but there have been other scourges of the past that seemed similarly intractable yet yielded to a concerted effort to decrease fatalities and suffering. AIDS, cancer, and motor vehicle fatalities are prominent examples, as all of these problems have shown dramatic declines in mortality due to a combination of medical advances and sound public policy decisions that largely came about due to increased awareness.
26,27,28 The advances are not necessarily easy, often involve tradeoffs and expense, and can be contentious, but I, along with many other clinicians and researchers, hope that the scourge of firearm violence can yield similar results with similar efforts.
REFERENCES
1. Blair JP, Schweit KW. A Study of active shooter incidents 2000-2013. Washington D.C.: Texas State University and Federal Bureau of Investigation, U.S. Department of Justice; 2014
2. Centers for Disease Control and Prevention. Fatal injury data [Internet].Atlanta (GA): CDC; [last updated 2017 Jun 22; cited 2017 Aug 22]. Available from:
https://www.cdc.gov/injury/wisqars/fatal.html. Accessed 9 October 2017
3. [13] National Academies of Sciences, Engineering, and Medicine. A National Trauma Care System: Integrating Military and Civilian Trauma Systems to Achieve Zero Preventable Deaths After Injury. Washington, D.C.: The National Academies Press. 2016. Available at:
www.nap.edu/23511. Accessed September 22, 2017. The entire report is available online and well worth the read.
4. Kellerman AL, Rivare FP. Silencing the science on gun research. JAMA. 2103;309:549-550
5. Livingston DH, Lavery RF, Lopreiato MC, et al. Unrelenting violence: an analysis of 6,322 gunshot wound patients at a Level I trauma center. J Trauma Acute Care Surg. 2014 Jan;76(1):2-9
6. Wintemute GJ. The Epidemiology of firearm violence in the twenty first century United States. Ann Review Public Health 2015;36:5-9
7. Morrison C, Gross B, Horst M, et al. Under fire: gun violence is not just an urban problem. J Surg Res. 2015 Nov;199(1):190-6.
8. Pennsylvania Uniform Crime Reporting System, Crime in Pennsylvania Annual Uniform Crime Report.
http://ucr.psp.state.pa.us/UCR/Reporting/Annual/AnnualFrames.asp?year=2015. Accessed 4 October 2017
9. Gross BW, Cook AD, Rinehart CD, Lynch CA, Bradburn EH1, Bupp KA, Morrison CA, Rogers FB. An epidemiologic overview of 13 years of firearm hospitalizations in Pennsylvania. J Surg Res. 2017 Apr;210:188-195.
10. National Conference on State Legislatures, Self Defense and “Stand Your Ground,” July 26, 2013, http://
www.ncsl.org/issues-research/justice/selfdefense-and-stand-your-ground.aspx. Accessed 28 Dec 2014
11. Gun bill passed by House could lead to NRA lawsuit against Pittsburgh. Pittsburgh Post-Gazette. October 21, 2014
12. Beard JH, Morrison CN, Jacoby SF, et al. Quantifying Disparities in Urban Firearm Violence by Race and Place in Philadelphia, Pennsylvania: A Cartographic Study, American Journal of Public Health 107, no. 3 (March 1, 2017): pp. 371-373.
13. Steinbrook R, Redberg RF. Firearm Injuries as a Public Health Issue JAMA Intern Med. 2013;173(7):488-489
14. Kalesan B, Vasan S, Mobily ME, et al. State-specific, racial and ethnic heterogeneity in trends of firearm-related fatality rates in the USA from 2000 to 2010 BMJ Open 2014;4:e005628 doi:10.1136/bmjopen-2014-005628
15. Faiz G, Sakran JV and Canner JK. Emergency department visits for firearm-related injuries in the United States, 2006–14 Health Aff October 2017 36:10 1729-1738
16. Aarabi B, Tofighi B, Kufera JA, et al. Predictors of Outcome in civilian gunshot wounds to the head. J Neurosurg 2014 May 120 (5): 1138-46
17. Ginwalla R, Rhee P, Friese R, et al. Repeal of the concealed weapons law and its impact on gun-related injuries and deaths. J Trauma Acute Care Surg. 2014 Mar;76(3):569-74
18. Webster D, Crifasi CK, Vernick JS. Effects of the repeal of Missouri's handgun purchaser licensing law on homicides. J Urban Health 2014 Apr;91(2):293-302
19. Kuhls DA, Campbell BT, Burke PA, et al. Survey of American College of Surgeons Committee on Trauma members on firearm injury: Consensus and opportunities. J Trauma Acute Care Surg. 2017;82(5):877-886
20. Puls MW, Kuhls DA, Campbell BT, et al. Survey of the American College of Surgeons Board of Governors on firearm injury prevention: Consensus and opportunities. Bulletin AM Coll Surgeons. 2017 102 (5) 30-36
21. Stewart RM, Kuhls DA, Campbell BT, et al. The COT’s consensus-based approach to firearm injury: An introduction. Bulletin AM Coll Surgeons. 2017 102 (5) 12-13
22. Chapman S, Alpers P, Jones M. Association Between Gun Law Reforms and Intentional Firearm Deaths in Australia, 1979-2013 JAMA. 2016;316(3):291-299.
23. Callcut RA, Robles AJ, Mell MW. Banning open carry of unloaded handguns decreases firearm related fatalities and hospital utilization. Presented at the 76th Annual Meeting of the American Association for the Surgery of Trauma, Baltimore, MD, Sept 14, 2017.
24. Cheng C, Hoekstra M Does strengthening Self-Defense law deter crime or escalate violence? Evidence from Castle Doctrine Working Paper 18134. http://
www.nber.org/papers/w18134 National Bureau of Economic Research Cambridge, MA 02138 June 2012. Accessed Oct 10 2017. Another paper well worth the read.
25. Moyer, MW Journey to Gunland. Scientific American, October 2017, 317: 4, 54-63
26. Murray CJL, Ortblad CG, Guinovert C, et al. Global, regional, and national incidence and mortality for HIV, tuberculosis, and malaria during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013 Lancet. 2014 Sep 13; 384(9947): 1005–1070.
27. DeSantis CE, Ma J, Goding Sauer A, et al. Breast cancer statistics, 2017, racial disparity in mortality by state. CA: A Cancer Journal for Clinicians. doi:10.3322/caac.21412
28. U.S. Department of Transportation An Analysis of the Significant Decline in Motor Vehicle Traffic Fatalities in 2008. https://
crashstats.nhtsa.dot.gov/Api/Public/ViewPublication/811346. Accessed 4 October 2017