
Summer 2017 - Vol. 12, No. 2
Axillary Central Venous Cannulation
for Cardiac Surgery
James J. Lamberg, D.O.
Anesthesia Associates of Lancaster
Editor’s Note: With this article, the Journal uses video-sharing for the first time, to enhance this article about the use of ultrasound for insertion of a central venous line. The links to the videos can be found in the on-line version of this article.
The technology for provision of a link to videos is well-established, but it is a new frontier for JLGH. We hope you find it intriguing, even if this procedure is not one you perform personally.
We can now incorporate links to videos stored on the hospital’s servers or on YouTube. Though videos can enhance articles of various types, they are particularly valuable for illustrating procedures and techniques. We hope the availability of videos in JLGH will prompt other authors to submit articles that utilize videos.
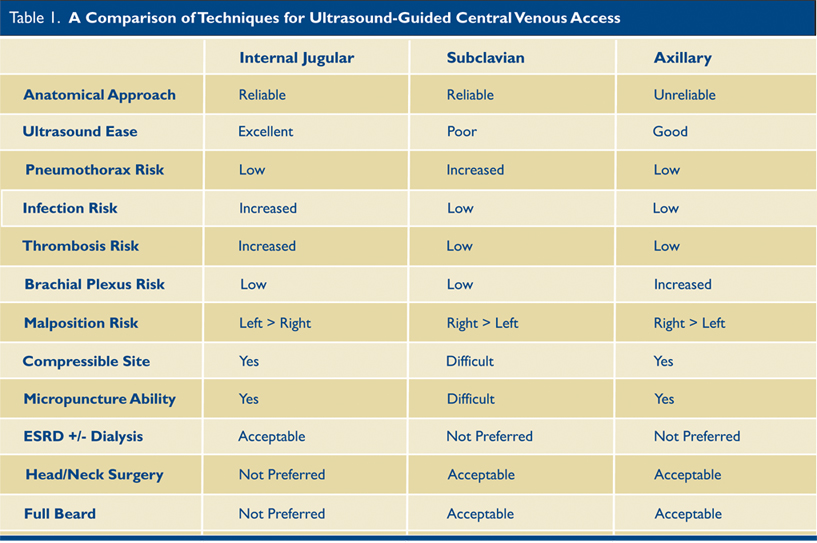
WHICH CENTRAL LINE LOCATION IS BEST?
Patients undergoing cardiac surgery have, by definition, severe cardiac disease, and complications during central line placement, such as iatrogenic pneumothorax, can have devastating consequences. Further, these patients will be fully anticoagulated for surgery, so accidental arterial puncture may further complicate their perioperative course. Several studies have compared central venous cannulation at the femoral, subclavian, and internal jugular sites. The axillary central line provides an alternative approach in cardiac surgery patients that can help to mitigate the risks involved with other central line locations.
CONFUSING TERMINOLOGY
Vascular cannulation is commonly named according to the vessel being cannulated, not the location of cannulation. To add some confusion for anesthesiologists, peripheral nerve blocks are commonly named by the location of needle insertion. Thus, an infraclavicular block is an approach to the brachial plexus for peripheral nerve block with insertion of the needle below the clavicle. For this nerve block, placement of the ultrasound probe and the site for needle insertion are similar to the axillary central line, which is placed into the axillary vein in the infraclavicular region, and not in the axilla.
To add another layer of confusion, study investigators do not always differentiate between ultrasound-guided axillary cannulation and subclavian cannulation. Anatomically, the subclavian vein becomes the axillary vein as it crosses the first rib underneath the clavicle. Ultrasound imaging of the subclavian vein is difficult due to its location, whereas imaging of the axillary vein is much less difficult. Studies that describe imaging of the subclavian vein in cross section (short-axis), may actually be describing imaging of the axillary vein.
ULTRASOUND VS. ANATOMICAL LANDMARK APPROACHES
Several randomized controlled-trials have compared anatomical versus ultrasound-guided approaches to the internal jugular vein.
1 The ultrasound-guided approach is associated with a higher first pass success rate, fewer overall attempts, and fewer complications. Similar findings were observed for femoral access, particularly in pediatric patients. For these reasons, ultrasound guidance is recommended by several organizations, including the American Society of Anesthesiologists.
1
For the subclavian approach, ultrasound allowed inexperienced operators to achieve higher success rates.
2 Another study showed higher success rates, reduced access time, and fewer arterial punctures with fewer hematomas.
3 (That study looked at the infraclavicular approach to the subclavian vein, with physicians rating the use of ultrasound technically difficult given acoustic shadowing of the first rib and sternum.) Ultrasound guided approaches are also more amenable to the micropuncture technique for central venous access,
4 which allows use of a needle smaller than the traditional 18-gauge steel needle, thereby reducing complications.
For axillary vein cannulation, an anatomical approach is discouraged because of the anatomical variance in this region and the risk of pneumothorax, so comparisons between anatomical and ultrasound-guided approaches need to be extrapolated from subclavian vein cannulation studies. However, an anatomical approach is described for infraclavicular peripheral nerve block,
5 which provides a starting point for ultrasound imaging of the axillary vein.
NECK OR CHEST?
There are four common ultrasound approaches to central venous access for the upper body: internal jugular, axillary, supraclavicular subclavian, and infraclavicular subclavian. The internal jugular (“neck line”) has been compared to the infraclavicular subclavian (“chest line”) in several studies. The infraclavicular site is associated with fewer infections,
6 easier maintenance, and improved patient tolerance.
7 For the anatomical approach at the infraclavicular site, there is a higher risk of pneumothorax and arterial puncture, including hemothorax and mediastinal hematoma. For cardiac surgery patients, the risk of these complications typically outweighs the risk of infection, thus many practitioners choose the internal jugular route for cannulation.
The axillary approach provides unique advantages. Infection risk is at least as low as the internal jugular approach
8 and may be similar to the subclavian approach. Additionally, the axillary vein is in a compressible site (whereas the subclavian vein is not), which enhances safety in the event of inadvertent arterial puncture or difficulty with vein dilation. The incidence of pneumothorax is also reduced,
2,3 and with experience, can approach that of internal jugular cannulation. Thus, the axillary central line is a suitable alternative for patients undergoing cardiac surgery.
There are several other situations in which the internal jugular or axillary vein would be preferable. The subclavian vein caliber is less susceptible to position changes and may remain patent in shock states,
9 making axillary or subclavian approaches favorable in patients who cannot lie flat or are hypotensive; there is less arterio-venous overlap at the axillary vein than at the subclavian vein,
10 reducing the risk of inadvertent arterial puncture; the risk of thrombosis for non-tunneled lines is lower for the axillary/subclavian approach compared with internal jugular cannulation,
11 though this may not be true for tunneled infusion catheters;
12 but given the location of the brachial plexus in relation to the axillary artery, the axillary approach has a theoretically greater risk of injury than other approaches.
13
In stroke patients, or those with traumatic brain injury, internal jugular access is commonly avoided due to the theoretical and debatable risk of venous outflow obstruction, which would increase intracranial pressure. Internal jugular access would also not be preferred for neck surgery or in patients with a cervical collar. Axillary and subclavian access is not preferred in patients with advanced renal failure or dialysis due to the risk of vein stenosis.
6 Axillary cannulation is useful in cardiac surgery patients with full beards that cannot be shaved for cultural and/or religious reasons (e.g. the Amish, Sikhs, and Muslims).
Regarding ultrasound-guided approaches to the subclavian vein, imaging was significantly better with the supraclavicular approach than the infraclavicular approach,
14 and in children the supraclavicular approach was preferred.
15 It should be noted that the infraclavicular approach studied here is the true subclavian puncture in the long-axis view, not the axillary puncture technique. Extrapolating these results to the axillary approach is difficult given the difference in ultrasound technique and the difficulty with imaging the subclavian vein beneath the clavicle.
Malposition of central venous catheters during insertion is an ongoing concern.
16 Several case reports have shown the tip of subclavian catheters in the contralateral subclavian or neck veins, too far into the right atrium (which is easily resolved), or in the axillary vein. One meta-analysis showed that catheter malposition is more common with subclavian catheters than with internal jugular cannulation,
16 but two case series with experienced operators showed higher rates of malposition with internal jugular catheters,
17,18 while yet another study showed no difference in malposition rates.
19 Despite the wide variation in study results, traditionally the risk of malposition occurs in the following order from highest to lowest: left internal jugular, right subclavian, left subclavian, right internal jugular.
20 This makes sense anatomically as the right internal jugular vein follows a direct path to the right atrium as does the left subclavian (or axillary) vein. Therefore, in cardiac surgery patients the left axillary vein would be preferred to the right for pulmonary artery catheterization.
AXILLARY CENTRAL VENOUS CANNULATION
Cannulation of the axillary vein in the infraclavicular region follows an approach similar to other ultrasound-guided central venous lines. Common safety measures for upper body central lines include Trendelenburg position to reduce air embolism, a sterile procedural bundle to reduce infections, patient monitoring for complications of sedation, and proper guidewire techniques to reduce the risk of cardiac arrhythmias and lost guidewire.
1
AXILLARY CENTRAL VENOUS CANNULATION PROCEDURE
The ultrasound probe is placed inferior to the mid clavicle. Probe orientation may be short-axis (“out of plane”), long-axis (“in plane”), or oblique. The short-axis orientation allows for both the axillary vein and artery to be visualized together (Fig. 1). Compressing the soft tissues allows differentiation of the compressible vein compared with the artery (Fig. 2). The long-axis orientation (Fig. 3) allows better visualization of the needle or wire during the procedure (Fig. 4)
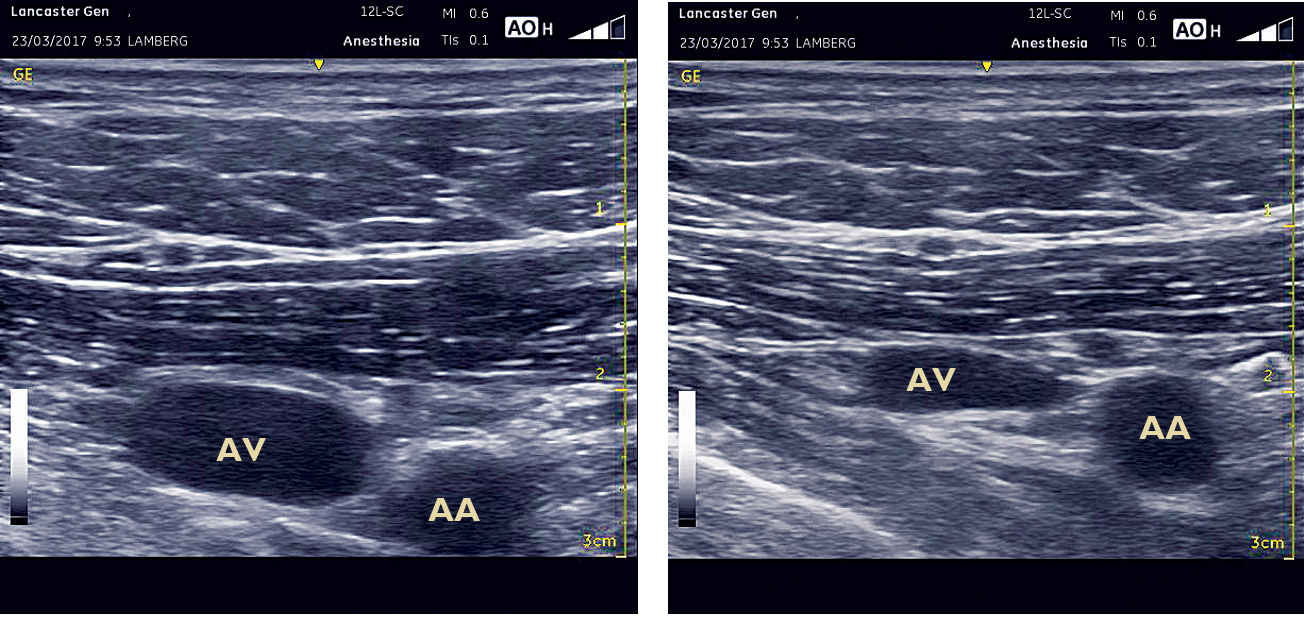 Fig. 1. Fig. 2.
Fig. 1. Fig. 2.
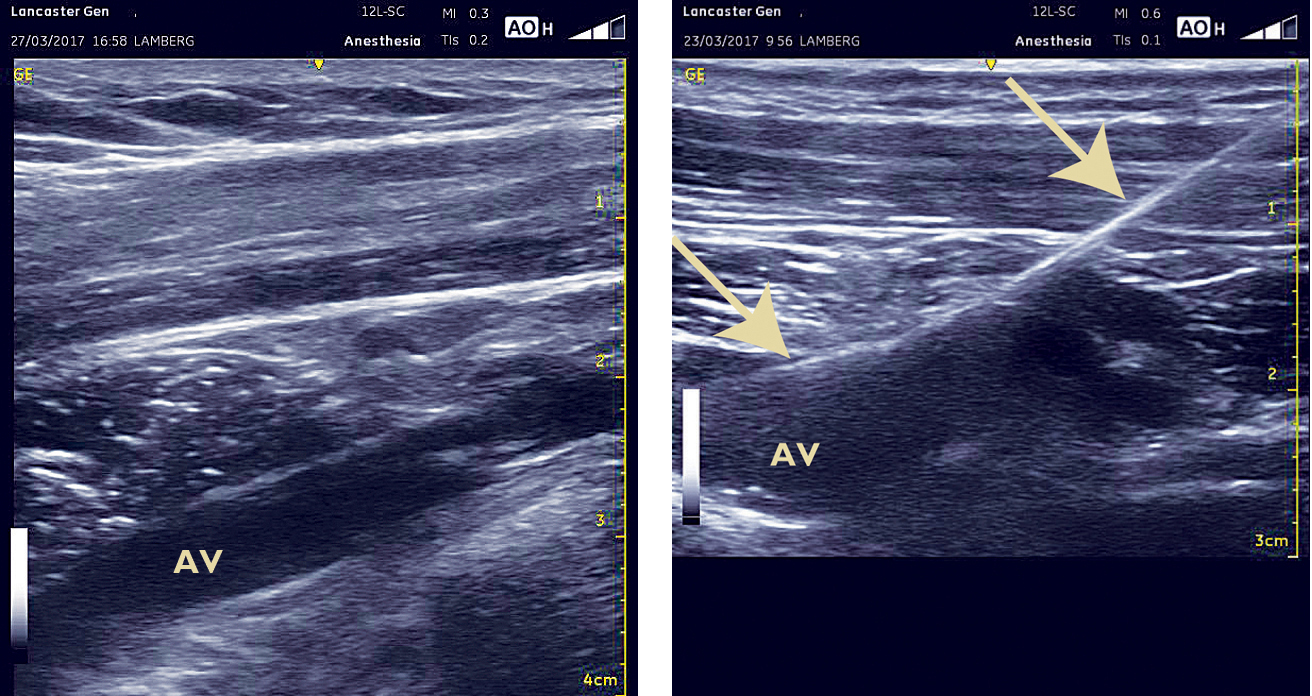 Fig. 3
Fig. 3.
Fig. 4.
AA=axillary artery; AV=axillary vein

The long-axis view was found to be more efficient and had fewer posterior wall penetrations,
21 which can decrease the risk of pneumothorax. The oblique view, which is far less common, is an attempt to provide the benefits of both the short- and long-axis orientations.
22
In the short-axis, the artery is commonly found cephalad. As the needle is advanced toward the target, ultrasound tissue movement is followed with the axillary vein centered on the ultrasound screen.
In the long-axis, sliding the probe caudal allows for visualization of both the artery and the compressible vein.
The micropuncture technique combined with the modified Seldinger technique is a common approach. This approach allows for a smaller gauge needle for vessel cannulation and allows for the insertion of a narrow catheter before vessel dilation. A guidewire can then be inserted and viewed in the long-axis (Fig. 4), or traced down to the vessel in the short-axis.
Before the vessel is dilated, venous placement should be confirmed. Pressure measurement has been found to have better sensitivity than ultrasound alone,
23 thus reducing the risk of inadvertent dilation of the artery. Since ultrasound reduces the risk of arterial puncture at the outset, these modalities are best used together.
24
SUMMARY
In cardiac surgery patients at risk for complications of subclavian central venous catheterization, the axillary central line provides an alternative to internal jugular venous cannulation. When central venous access via the subclavian vein is indicated, axillary cannulation with ultrasound guidance provides a reduced incidence of procedural complications.
In memory of Serge-Marcel Cabrol.
REFERENCES
1. American Society of Anesthesiologists Task Force on Central Venous Access. Practice guidelines for central venous access: a report by the American Society of Anesthesiologists Task Force on Central Venous Access. Anesthesiology. 2012;116:539-73.
2. Gualtieri E, et al. Subclavian venous catheterization: greater success rate for less experienced operators using ultrasound guidance. Crit Care Med. 1995;23:692-7.
3. Fragou M, et al. Real-time ultrasound-guided subclavian vein cannulation versus the landmark method in critical care patients: a prospective randomized study. Crit Care Med. 2011;39:1607-12.
4. Castillo D, et al. Micropuncture needles combined with ultrasound guidance for unusual central venous cannulation. Anesth Analg. 2012;114:634-7.
5. Mosaffa F, et al. Comparing vertical and coracoid approaches for infraclavicular block in orthopedic surgery of the forearm and hand. J Clin Anesth. 2012;24:196-200.
6. O'Grady NP, et al. Guidelines for the prevention of intravascular catheter-related infections. Am J Infect Control. 2011;39:S1-34.
7. Kaplan JA, et al. Central Venous Pressure Monitoring: Technique and Insertion Sites. Kaplan’s Cardiac Anesthesia. Philadelphia, PA: Elsevier, Inc., 2017. pp 390-426.
8. Martin C, et al. Catheter-related infections following axillary vein catheterization. Acta Anaesthesiol Scand. 1998;42:52-6.
9. Bannon MP, et al. Anatomic considerations for central venous cannulation. Risk Manag Healthc Policy. 2011;4:27-39.
10. Galloway S, et al. Ultrasound imaging of the axillary vein--anatomical basis for central venous access. Br J Anaesth. 2003;90:589-95.
11. Parienti JJ, et al. Intravascular Complications of Central Venous Catheterization by Insertion Site. N Engl J Med. 2015;373:1220-9.
12. Trerotola SO, et al. Tunneled infusion catheters: increased incidence of symptomatic venous thrombosis after subclavian versus internal jugular venous access. Radiology. 2000;217:89-93.
13. Mackey SP, et al. Ultrasound imaging of the axillary vein--anatomical basis for central venous access. Br J Anaesth. 2004;93:598-9; author reply 599.
14. Stachura MR, et al. A comparison of the supraclavicular and infraclavicular views for imaging the subclavian vein with ultrasound. Am J Emerg Med. 2014;32:905-8.
15. Byon HJ, et al. Comparison between ultrasound-guided supraclavicular and infraclavicular approaches for subclavian venous catheterization in children--a randomized trial. Br J Anaesth. 2013;111:788-92.
16. Timsit JF. What is the best site for central venous catheter insertion in critically ill patients? Crit Care. 2003;7:397-9.
17. Gladwin MT, et al. Cannulation of the internal jugular vein: is postprocedural chest radiography always necessary? Crit Care Med. 1999;27:1819-23.
18. Lefrant JY, et al. Risk factors of failure and immediate complication of subclavian vein catheterization in critically ill patients. Intensive Care Med. 2002;28:1036-41.
19. Iovino F, et al. [Central venous catheterization: complications of different placements]. Ann Chir. 2001 Dec;126(10):1001-6.
20. Schummer W, et al. Mechanical complications and malpositions of central venous cannulations by experienced operators. A prospective study of 1794 catheterizations in critically ill patients. Intensive Care Med. 2007;33:1055-9.
21. Vogel JA, et al. Is long-axis view superior to short-axis view in ultrasound-guided central venous catheterization? Crit Care Med. 2015;43:832-9.
22. Phelan M, et al. The oblique view: an alternative approach for ultrasound-guided central line placement. J Emerg Med. 2009;37:403-8.
23. Togashi K, et al. A multicenter evaluation of a compact, sterile, single-use pressure transducer for central venous catheter placement. Anesth Analg. 2013;116:1018-23.
24. Bowdle A. Vascular complications of central venous catheter placement: evidence-based methods for prevention and treatment. J Cardiothorac Vasc Anesth. 2014;28:358-68.
.