
Winter 2016 - Vol. 11, No. 4
Osteoporosis, the Silent Disease
Prevention and Treatment of Fragility Fractures
in a Structured Program
Rodney E. Brenneman, M.D.
Orthopedic Associates of Lancaster Ltd.
Physician Leader, Geriatric Fracture Program at Lancaster General Health
THE OSTEOPOROSIS CHALLENGE
In 2001, the National Institutes of Health defined osteoporosis as “a skeletal disorder characterized by compromised bone strength predisposing a person to an increased risk of fracture.”
1 Bone mass and density are highest between the ages of 18 and 25, and they decline slowly and steadily thereafter. Current estimates suggest that 200 million people worldwide are affected by osteoporosis, resulting in 8.9 million fractures annually.
2,3 The National Osteoporosis Foundation has estimated that 9.9 million Americans have osteoporosis.
4 Osteoporosis has been labeled the “silent” disease, because its development is often unrecognized until a fracture occurs. Risk factors for such fractures include low body mass index, a history of osteoporosis-related fracture, early menopause, smoking, vitamin D deficiency or insufficiency, other endocrine abnormalities, use of glucocorticoids, excessive alcohol intake, immobility, and other factors.
2
THE FRACTURE BURDEN
Approximately 50% of women and 25% of men over the age of 50 will have a fragility fracture in their lifetime.
5 Hip fractures are the most widely recognized type, though they comprise just a fraction of the burden of osteoporosis-related fractures, which can also occur at the proximal humerus, clavicle, distal radius, spine, pelvis, hip, knee, and ankle. There are more than 300,000 hospital admissions annually for hip fractures in patients over the age of 65 in the U.S.
6 By 2040 that number could exceed 550,000,
2 and by 2050 there could be more than 21 million hip fractures annually worldwide.
2 The estimated cost of hip fracture care in the U.S. rose from $7.2 billion in 1984 to $20 billion in 1997, and it could reach $62 billion by 2040.
7
Hip fractures may be only a fraction of all osteoporosis-related fractures, but they are the most easily studied due to their nearly universal requirement for surgical treatment. Their mandatory hospital admissions, operations, and associated services provide a captive population for research and quality improvement initiatives.
5 Hip fractures also have a much more deleterious effect on quality of life and functional independence than most other fractures. The one-year mortality rate following a hip fracture is 20-30%,
8 and 30-50% of hip fracture patients lose the ability to walk without assistance or to live independently.
4
DIAGNOSIS AND MANAGEMENT OF OSTEOPOROSIS
Despite national and global initiatives to increase awareness and detection, osteoporosis diagnosis and treatment remains at dismal levels, with only 23% of women over the age of 66 with an osteoporosis-related fracture receiving bone density testing or treatment for osteoporosis within six months of the fracture.
2 The diagnosis and management of osteoporosis should be directed by a physician comfortable with doing so. In that regard, many primary care physicians are proficient at osteoporosis management, but some may either lack expertise, or may simply be overwhelmed by the demands of patients with more acute health care problems.
Evaluation of patients should begin with a detailed history and physical examination, followed by bone density testing and/or FRAX assessment (see below), with further consideration of pharmacologic treatment. In addition, it is important to address exercise, calcium and vitamin D intake, fall prevention, lifestyle (including use of tobacco and alcohol), as well as any potential secondary causes of osteoporosis.
8
Bone Mineral Density and Prediction of Fractures
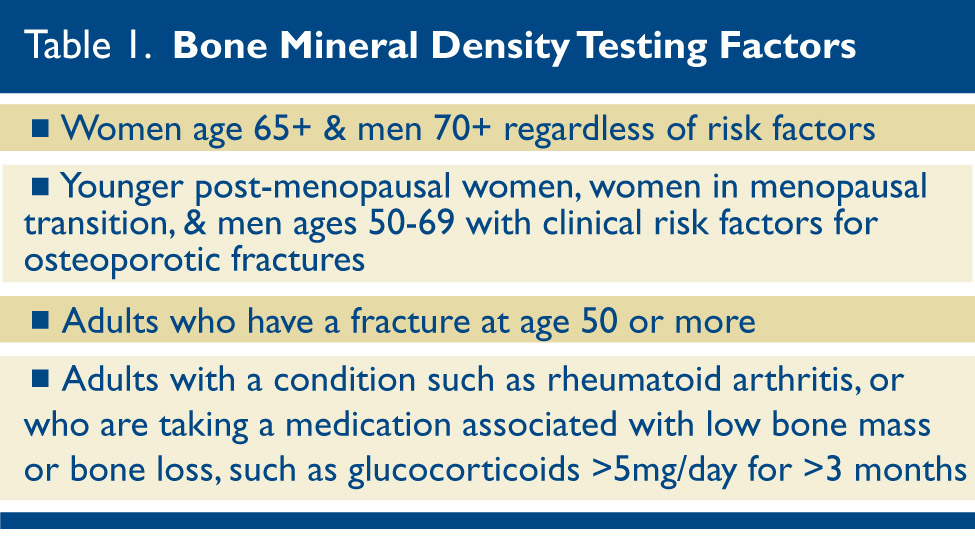
The U.S. Preventive Services Task Force offers guidelines for bone mineral density testing.
4 (Table 1.)
Dual-energy X-ray Absorptiometry (DXA) was developed in the 1980s and has become the mainstay of bone mineral density testing.
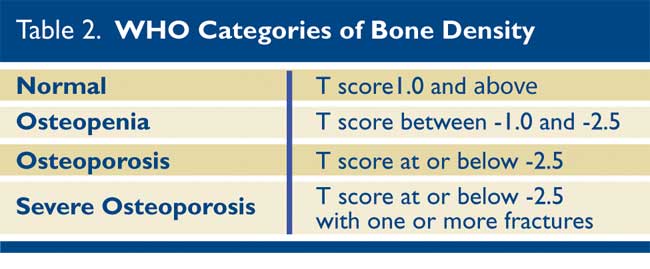
1,4 X-rays of the spine, hip, and sometimes wrist are taken, and the bone density at each area is compared either with a reference population matched for age, gender, and ethnicity (Z score), or with a young and healthy individual matched for gender (T score). The World Health Organization (WHO) has defined four categories of bone density.
4 (Table 2)
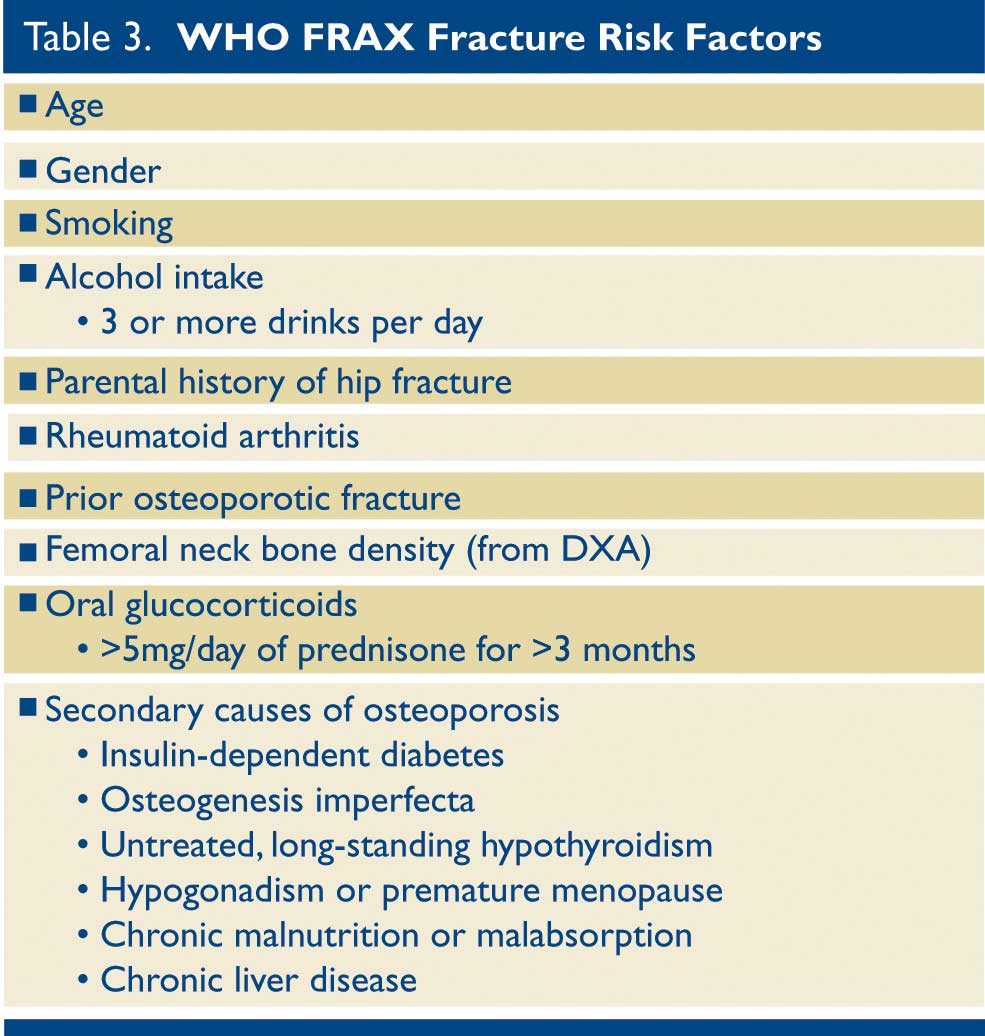
The WHO FRAX tool is a fracture prediction model that was developed recently by following 60,000 patients who sustained over 5,000 fractures. The model predicts the absolute risk of major osteoporotic fractures (hip, spine, forearm, and humerus), as well as the 10-year risk of hip fractures.
1 (Table 3)
Many “bone protective” medications, including bisphosphonates, have been shown to be very effective at slowing the progression of osteoporosis. They are well tolerated by most patients, but occasional side effects and a few very rare but drastic complications have produced an unnecessary fear of these medications among the public. Indeed, three separate reports by the U.S. Food and Drug Administration from 2005 to 2010 on extremely rare adverse effects have led to a severe decline in bisphosphonate use. In over 22,000 patients with hip fracture, the use of bisphosphonate medication decreased from an already-dismal 15% in 2004 to an abysmal 3% in 2013.
9 The lives saved and/or improved by the judicious use of appropriate bone-protective medications would far outweigh the potential risks of these rare side effects. A detailed discussion of the different pharmacologic options is beyond the scope of this article.
The rheumatologists and endocrinologists at LGH have specialized training in understanding, diagnosing, and managing the complexities of osteoporosis and treatment of its consequences.
A VISION FOR A GERIATRIC FRACTURE PROGRAM AT LGH
Studies of hip fracture management have shown that a structured approach with standardized and co-managed care can reduce length of stay and cost of care, and can improve functional outcomes after discharge.
10 In light of the societal and personal burden of hip fractures, over the past two decades there has been a rise in the number of comprehensive fracture programs that seek to optimize outcomes.
8
In 2009 Gerald W Rothacker Jr., M.D., returned from the annual meeting of the Pennsylvania Orthopedic Society with a vision for a Geriatric Fracture Program (GFP) at Lancaster General Hospital dedicated to improving the care of elderly patients with a fracture of the hip or femur. He was inspired by a model program developed by the orthopedic implant company Synthesis, but he was the visionary who developed the GFP and brought it to fruition at LGH.
The program began in September 2009 with monthly meetings involving representatives from a broad spectrum of teams that help care for these patients. Initial discussions involved physicians, mid-level providers, and nurses from Emergency Medicine, Orthopedics, Internal Medicine, Cardiology, Anesthesia, Geriatrics, and Rheumatology. There were also representatives from pharmacy, surgical services, social work, nutrition, physical therapy, hospital administration, data management, and marketing. Melody Dillman, R.N., was the LGH Orthopedic Program coordinator at the time and was also instrumental in the inception and development of the program. Stacey Youcis, who at that time was vice president of operations, participated, encouraged, and provided LGH institutional support. Richard W. Reese M.D., medical director of the LGH Orthopedic Center and senior rheumatologist at LGH Physicians Arthritis and Rheumatology Specialists, has been involved with the GFP from the outset. As a local champion of osteoporosis awareness, he continues to help the GFP focus on primary and secondary fracture prevention.
This initial team of dedicated individuals found many complex challenges that were impeding optimal care of these fragile patients. To identify and work through these challenges, the team meticulously inspected the path of hip fracture patients from their entry into the Emergency Department to their eventual discharge from the hospital. The team then developed order sets and treatment protocols that improved efficiency at every stage. Not surprisingly, though their primary goal was improved care of these patients, it became rapidly apparent that there were secondary benefits in decreased length of stay and cost of care.
THE GERIATRIC FRACTURE PROGRAM
Initial Evaluation
A patient with a hip fracture usually has a characteristic physical appearance, with a shortened and externally rotated leg.
11 Given the reliability of the initial physical exam by an experienced emergency medicine physician, timely treatment of a hip fracture begins at that moment, even prior to any confirmatory imaging. To eliminate any step-wise delay, an emergency department set of orders for all appropriate imaging and laboratory studies, pain management, and consultations was developed. The vast majority of these patients are admitted to the orthopedic service with an internal medicine consultation prior to surgery. The orthopedic and internal medicine physicians agreed to expedite their evaluations with the goal of reducing the amount of time a hip fracture patient remains in the Emergency Department.
Anticoagulant Reversal
Many of the patients with hip fractures are chronically anticoagulated. The various anticoagulants used require different “reversal” regimens, and can delay surgery. Though warfarin, the most common long-term anticoagulant, can be safely and effectively reversed with oral or intravenous vitamin K,
12 one early finding of the GFP was that physicians were slow or reluctant to order this medication. As a result, a conditional order for the prompt administration of vitamin K based on the initial PT/INR results was built into the orthopedic admission order set. This routine avoided the need for blood coagulation products or waiting for the passive normalization of the coagulation profile.
Timing and Surgical Delay
Improved communication between the inpatient charge nurse and the orthopedic operating room coordinator facilitated the physical transport of the patients to the operating room suite and helped clarify any pending or completed preoperative workup. Indeed, sometimes the patient would go directly from the Emergency Department to the preoperative holding area. Whereas only 54% of hip fracture patients had their surgery within 24 hours of presentation to the ED in 2009, that number had risen to 73% by 2014. Due to improvements in both preoperative and postoperative patient management, the average length of stay for a hip fracture patient at LGH decreased by 36%: from 6.7 days in 2009 to 4.3 days in 2014.
Preoperative Echocardiograms
The GFP found a strong association between the ordering of a preoperative echocardiogram and a delay in surgery of as much as 66 hours. With emerging literature supporting the need to perform hip fracture surgery as soon as medically reasonable, a dedicated collaborative team from cardiology, anesthesia, medicine and orthopedics developed a stringent algorithm to decide exactly which patients must have a preoperative echocardiogram.
13 Implementing this algorithm brought the use of preoperative echocardiograms down from 19% in 2009 to 9% in 2012 without an increase in complications, including in-hospital mortality.
Blood Transfusions
Blood transfusions have been shown to increase the risk of perioperative infections, length of stay, and overall cost of care. Multiple studies of different transfusion protocols have shown that stricter criteria for transfusion do not increase complications.
14,15 A restrictive transfusion protocol (hemoglobin 7 gm/dL absolute threshold; 8 gm/dL for those with unstable angina, myocardial infarction, or cardiogenic shock) was adopted based on recommendations by the American Academy of Orthopedic Surgeons Clinical Practice Guidelines.
16 Transfusion rates at LGH in hip fracture patients subsequently dropped from 55% in 2010 to 25% in 2016 without a rise in readmissions for anemia.
Nursing Unit and Delirium
A major logistical tactic was to consolidate all patients with hip fractures in one nursing unit (4 North). The nursing staff became dedicated to the nuances of this fragile population, particularly with regard to recognizing the subtle but important impact that delirium can have on a hip fracture patient. Delirium, defined as temporary confusion and disorientation distinct from dementia, has a reported incidence in hip fracture patients of 35-65% nationally. It can lead to an additional seven days of hospitalization and a proportionate increase in cost.
17 The Confusion Assessment Method is a verified delirium assessment tool that was adopted to screen for delirium, along with the development of standardized order sets for treatment to shorten the duration of delirium.
18 The real work in this arena is in the prevention of delirium, and the nursing staff is increasingly engaging family members to help recognize the warning signs and to prevent or detect delirium early. The rate of delirium in LGH hip fracture patients has dropped from 21% in 2011 to 9.7% in 2016. The nursing staff from 4 North has been teaching other nursing units about the impact, prevention, detection, and treatment of delirium.
Pain Management
Pain management is a unique challenge in the hip fracture patient for several reasons: a) a hip fracture is sudden so neither the patient nor the family has any chance to prepare; b) schedules and plans are immediately disrupted; c) the patient may feel that s/he is now even more of a burden on family and loved ones, which compounds the patient’s own physical and psychological suffering. Elderly patients often under report pain, whether from a true increase in pain threshold, cognitive impairment, or the feeling of personal burden. Uncontrolled pain can in turn lead to delirium, increased length of stay, and unwillingness to participate in therapy. On the other hand, elderly patients often have increased cerebral sensitivity to narcotics, which can in turn induce delirium.
Notwithstanding its cost, intravenous acetaminophen can reduce length of stay, pain scores, and narcotic usage, and can increase participation in therapy, all of which increase rates of discharge to home.
19,20 Scheduled IV acetaminophen was therefore introduced into preoperative and postoperative order sets and the ordering of narcotics was highly discouraged unless pain levels required it. The reporting of pain management has been a challenge to document, with the current methodology showing approximately 50-60% effectiveness in meeting the patient’s expected level of manageable pain.
Physical Therapy
Participation in therapy is a key element in postoperative management of hip fractures. The immediate benefits of mobilization out of bed are a reduction in atelectasis (which can lead to pneumonia), decreased risk of skin compromise from pressure necrosis, and simplification of personal care. Weight-bearing status can have a profound effect on overall mobilization, since most hip fracture patients are unable to accomplish limited weight bearing. While the characteristics of their fracture and subsequent treatment are unique to each patient, the goal after surgery is to achieve weight bearing as tolerated. The long-term focus of postoperative therapy is on gait, balance, and strengthening – with intention of preventing future falls.
11,20
In the last few years, 80% of the LGH hip fracture patients have been getting out of bed the day after surgery. To encourage early mobilization, a recent initiative has been to have them sitting on the side of their bed the evening of surgery.
Nutrition
The nutritional status of many hip fracture patients is less than ideal, which may have itself contributed to the level of osteoporosis or even to the event that precipitated the fracture. Cognitive impairment, poor dentition, lack of appetite, delirium and dementia can all have a negative impact on postoperative nutrition. Adequate caloric intake and proper blood glucose control are imperative for good wound healing, which is inversely correlated with postoperative wound infection.
11,20 Nutritionists and nurses together have spearheaded an initiative through the GFP called PRONS – Promoting Recovery through Oral Nutritional Supplements. Through creative techniques, oral supplements have become standard both in the diet and with medication, sometimes representing the majority of caloric intake. The success of this program has been presented at a recent national nursing convention, and is also now being implemented throughout LGH.
Post-acute Care and Prevention
Discharge destinations of LGH hip fracture patients has varied somewhat over the last few years, with 70% currently going to Skilled Nursing Facilities (SNFs), 23% to inpatient rehab, and 6% to independent living. Recently the LGH GFP has been part of a collaborative initiative to improve the care of hip fracture patients after they are discharged from the hospital. LGH has partnered with 10 area SNFs to develop a Hip Fracture Clinical Plan including a standardized approach for wound management, physician follow-up visits, medication management, nutrition, therapy, and pain control. One goal is to reduce the length of stay at the SNF in an effort to reduce the overall cost of post-acute care. Recent reports show that only 27% of hip fracture costs are associated with the acute inpatient hospitalization, while the remainder comes from managing these patients after discharge.
5 With the growing burden of the aging population and its associated health-care costs, improving the efficiency of care will increasingly be the center of attention.
Though the risk of non-hip fractures obviously increases with age, their peak incidence is earlier. Forearm fractures, for example, peak in the sixth decade, whereas hip fractures tend to occur in the eighth decade.
3 The appropriate diagnosis and treatment of osteoporosis after the forewarnings provided by lower-impact fractures can lead to the secondary prevention of additional fractures – potentially preventing much more ominous hip fractures. The LGH GFP is currently working with representatives from the Radiology department to have automated letters generated based on the results of all X-rays performed in the LGH system. This has the potential for outreach to a vast number of patients who may not receive osteoporosis education otherwise.
The treatment of osteoporosis in geriatric hip fracture patients remains a challenge for the GFP. Because patients are scattered throughout the post-acute care network, many with new primary care physicians, and because use of resources is currently focused on recovery and rehabilitation, the diagnosis and treatment of osteoporosis is often neglected. This area will remain an active area of future development for the GFP.
REFERENCES
1. Lorentzon M, Cummings SR. Osteoporosis: the evolution of a diagnosis. J Intern Med. 2015;277:650-61.
2. Pisani P, Renna MD, Conversano F, et al. Major osteoporotic fragility fractures: risk factor updates and societal impact. World J Orthop. 2016 Mar 18;7(3):171-81.
3. Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteopros Int. 2006 Dec;17(12):1726-33.
4. Cosman F, de Beur SJ, LeBoff MS, et al. Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int. 2014;25:2359-81.
5. Nazrun AS, Tzar MN, Mokhtar SA, et al. A systematic review of the outcomes of osteoporotic fracture patients after hospital discharge: morbidity, subsequent fractures, and mortality. Ther Clin Risk Man. 2014;10:937-48.
6. Agency for Healthcare Research and Quality. HCUP facts and figures: statistics on hospital-based care in the United States. 2009.
http://www.hcup-us.ahrq.gov/reports/factsandfigures/2009/pdfs/FF_report_2009.pdf
7. Kates SL, Mendelson DA, Friedman SM. The value of an organized fracture program for the elderly: early results. J Orthop Trauma. 2011;25:233-37.
8. Collinge CA, McWilliam-Ross K, Beltran MJ, et al. Measures of clinical outcome before, during, and after implementation of a comprehensive geriatric hip fracture program: is there a learning curve? J Orthop Trauma. 2013;27:672-6.
9. Kim SC, Kim DH, Mogun H, et al. Impact of the U.S. Food and Drug Administration’s safety-related announcements on the use of bisphosphonates after hip fracture. J Bone Miner Res. 2016;31(8);1536-40.
10. Wang H, Li C, Zhang Y, et al. The influence of inpatient comprehensive geriatric care on elderly patients with hip fractures: a meta-analysis of randomized controlled trials. Int J Clin Exp Med. 2015;8(11):19815-30.
11. Bukata SV, DiGiovanni BF, Friedman SM, et al. A guide to improving the care of patients with fragility fractures. Ger Orthop Surg Reh. 2011;2(1):5-37.
12. Vitale MA, Vanbeek C, Spivack JH, et al. Pharmacologic reversal of warfarin-associated coagulopathy in geriatric patients with hip fractures: a retrospective study of thromboembolic events, postoperative complications, and time to surgery. Geriatr Orthop Surg Rehabil. 2011 Jul;2(4):128-34
13. Fleisher LA, et al. ACC/AHA 2007 guidelines on perioperative cardiovascular evaluation and care for noncardiac surgery. J Am Coll Cardiol. 2008 Aug 26;52(9):793-4.
14. Spahn DR. Anemia and patient blood management in hip and knee surgery: a systematic review of the literature. Anesthesiology. 2010;113:(2),482-95.
15. Brunskill SJ, Millette SL, Shokoohi A, et al. Red blood cell transfusion for people undergoing hip fracture surgery. Cochrane Database Syst Rev. 2015 Apr 21;(4).
16. Carson JL, et al. Liberal or restrictive transfusion in high-risk patients after hip surgery. N Eng J Med. 2011 Dec 29;365(26):2453-62.
17. Zywiel MG, Hurley R, Perruccio A, et al. Health economic implications of perioperative delirium in older patients after surgery for a fragility hip fracture. JBJS. 2015;97:829-36.
18. Inouye SK, van Dyck CH, Alessi CA, et al. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990 Dec 15;113(12):941-8.
19. Bollinger AJ, Butler PD, Nies MS, et al. Is scheduled intravenous acetaminophen effective in the pain management protocol of geriatric hip fractures? Geriatr Orthop Surg Rehabil. 2015;6(3):202-8.
20. Roberts KC, Brox WT, Jevsevar DS, et al. AAOS clinical practice guideline summary: Management of hip fractures in the elderly. J Am Acad Orthop Surg. 2015;23(2):131-37.