
Winter 2016 - Vol. 11, No. 4
A Brief History of Bloodletting
Timothy M. Bell, MLS (ASCP)CM
For the Edward Hand Medical Heritage Foundation
Editor’s Note: This article is another demonstration of our productive relationship with the Edward Hand Medical Heritage Foundation, and the sophisticated work that can be done by outstanding students even before they embark on their graduate education. Readers may recall the excellent article on Poliomyelitis in Lancaster County that we published in the Summer 2015 issue by Ellen Hendrix, then a senior at Franklin & Marshall College. The following article was written by a student working on an internship from the EHMHF.
INTRODUCTION
Bloodletting is a medical tradition that probably began in prehistoric times. Its rationale was based on the belief that removing blood eliminated “impure” fluids. From antiquity until the beginning of the 19th century, bloodletting was considered a panacea, and it was the most common and versatile form of medical treatment. Not only was it believed to cure the sick, but also to promote vigor in the healthy.
One medieval author wrote, “It makes the mind sincere, it aids the memory, it purges the brain, it reforms the bladder, it warms the marrow, it opens the hearing, it checks tears, it removes nausea, it benefits the stomach, it invites digestion, it evokes the voice, it builds up the sense, it moves the bowels, it enriches sleep, it removes anxiety.”
1
METHODS
Depending on the illness, bleeding was done at different areas of the body, although it was traditionally performed at the elbows and knees using one of several different methods. The most common, called general bloodletting, involved cutting open a vein (phlebotomy) or artery with a tool.
2 Among the earliest were naturally sharp thorns or animal teeth, or sharpened pieces of wood, stone or bone. Later, sharper instruments were developed, and since the time of Hippocrates surgeons frequently carried a variety of different sized lancets or scalpels. These small and extremely sharp double-bladed instruments were used for a variety of procedures, but as bloodletting became popular in the Roman Empire, flebotomes, a type of lancet known for its straight, sharp-pointed, double-edged blade, became popular. The thumb lancet was introduced in the 15th century and consisted of a double-edged blade of iron or steel screwed together between two decorative covers, usually of horn or shell. It became the preferred tool for opening veins because it could be used at various angles, and the width of the blade could be varied depending on where the vein was located. In the 17th and 18th centuries, fleams became popular. These cutting implements utilized a pointed edge set at a right angle to the handle (Fig. 1).
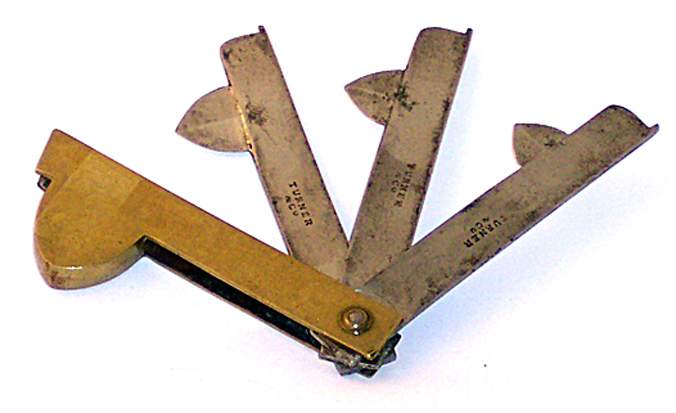 Fig. 1. Brass and steel fleam signed "Turner & Company." Photo courtesy of Ed Welch Antiques.
Fig. 1. Brass and steel fleam signed "Turner & Company." Photo courtesy of Ed Welch Antiques.
Later, spring lancets were invented in Vienna, which allowed a physician to open a vein without applying manual pressure. The small blade was attached at a right angle to a spring-loaded lever in the handle that could be released with a lever or button (Fig. 2).
 Fig. 2. Spring-loaded fleam imprinted "Wiegand &
Fig. 2. Spring-loaded fleam imprinted "Wiegand &
Snowden, Philadelphia." Photo courtesy of the
Edward Hand Medical Heritage Foundation.
At the time, the spring lancet was a safer way to draw blood due to its small size and design. The lancet’s intricate construction made it harder to clean, however, and often resulted in a higher rate of infection.
3
Other, more localized methods of bloodletting removed blood only from capillaries. Application of one or more leeches was a popular method, since a single leech can ingest 5-10mL of blood, and due to the anticoagulant effects of their bite, a total of 40-60mL of blood might be lost at once.
4 Cupping was another popular method that is still practiced today in traditional Chinese medicine. (See editor’s note at end for a comment on its use in modern Western subjects, particularly athletes.) It was favored if a patient was thought to be too young, too old, or too weak to undergo phlebotomy. Either dry or wet cupping was used. In the former, blood was not actually removed from the body, but a glass cup from which the air had been extracted by heating the glass or by vacuum-suction, was placed over the area. This process caused the skin to become swollen and bruised. For wet cupping, the skin was either scraped or cut open before the cups were applied, thus actually removing blood from the body.
HISTORY
Bloodletting is one of the oldest medical treatments in the world, and has been found in societies everywhere, ranging from the writings of esteemed Chinese and Tibetan physicians, to African shamans and Mayan priests. Writing and pictorial references to phlebotomy have also been found in texts dating back to the ancient Mesopotamians and Egyptians. Some medical anthropologists have even suggested that bloodletting as a medical treatment is embedded in our common human subconscious, which explains why it appeared in so many diverse cultures.
5
In Western medicine, the use of bloodletting originated with the Greeks, who received it from the Egyptians and passed it onto the Romans. Hippocrates recorded that bleeding was good for reducing local inflammation and treating fevers and apoplexy. Celsus, a Roman medical writer in the 1st century AD, wrote, “To let blood by incising a vein is no novelty: what is novel is that there should be scarcely any malady in which blood should not be let.”
4
GALEN AND THE FOUR HUMORS
The popularity of bloodletting in Ancient Rome was heavily influenced by Galen, the foremost authority on anatomy and medicine, who became the personal physician to Marcus Aurelius.
6 Galen’s writings became the foundation of the Western medical tradition for over 1,300 years. He summarized the knowledge of his predecessors while adding his own experiences and philosophies gleaned from treating the wounds of gladiators as well as from dissections of pigs and monkeys. (Roman law at the time prohibited the dissection of human cadavers). Among his other contributions to medicine, Galen was the first to show that blood, not
pneuma (vital spirit), flowed through veins, and to document the difference between arterial and venous blood. He ascribed to the Hippocratic principles of pathology, which were based on the idea that there is a balance between four primary fluids in the body: blood, yellow bile, black bile and phlegm. Each of the fluids was paired with one of the four elements of nature, an organ of the body, and a human temperament. Blood was associated with air, the heart, and a sanguine temperament, described as optimistic and leader-like. Yellow bile was associated with fire, the liver, and a choleric temperament with irritability. Black bile was linked with earth and the spleen, and those with excess black bile were thought to be melancholic, analytical, and quiet. Finally, phlegm was associated with water and the brain and led to a phlegmatic temperament, which was relaxed and peaceful.
It was believed that illness occurred because these fluids, also known as humors, became unbalanced within the patient’s body, a condition known as plethora. Based on this belief, the physician needed to rebalance the humors to cure the illness. The evacuation of the offending humor could be carried out through purging, starvation, or bloodletting.
The humor-based theory of disease remained the prevailing standard of care throughout the West. The Church, the only institution to survive the Fall of Rome, became the repository of medical knowledge, but it focused on the metaphysical aspects of life and often took a dim view of science. During the Middle Ages, physicians were often academics who were contemptuous of surgery, which led to the rise of barber-surgeons who performed many operations including bloodletting, tooth-pulling and amputations.
* After the fall of Constantinople, fleeing Greek and Jewish scholars spread Hellenistic medical traditions in the diaspora, combined with the advances made by the Arabs during the Golden Age, which included developments in pharmacology, anatomy, and differential diagnosis.
7
BLOODLETTING IN RECENT TIMES
Bloodletting was still practiced up through the 18th and 19th centuries, especially in Europe, for fever, hypertension, pulmonary inflammation, and pulmonary edema. Blood was usually drained until the patient exhibited syncope, which usually occurred after about 600mL. Despite William Harvey’s discovery of the circulation of blood, even he continued to believe that bloodletting was a reasonable treatment for disease, proclaiming: “daily experience satisfies us that bloodletting has a most salutary effect in many diseases, and is indeed the foremost among all the general remedial means: vitiated states and plethora of blood are causes of a whole host of disease; and the timely evacuation of a certain quantity of the fluid frequently delivers patients from very dangerous disease and even from imminent death.”
3 Francois Broussais, a prominent early 17th century Parisian physician, proposed the theory that all fevers were due to inflammation of a specific organ, and that use of leeches along with aggressive bloodletting was the best course of treatment. John Hunter, the founder of modern surgery, advocated the use of bloodletting in his 1794 treatise for the treatment of apoplexy and inflammation.
4 He believed that in some cases bleeding could be effective in treating smallpox. For gonorrhea, he recommended the application of leeches to the scrotum and testicles.
Bloodletting became popular in early American history; Benjamin Rush, a prominent Philadelphia physician and a signer of the Declaration of Independence, now hailed as the “Pennsylvania Hippocrates” and “Father of Modern Psychiatry,” fiercely advocated its use. Percy Moreau Ashburn, a professor of medical hygiene at West Point, wrote of Rush in his 1929
History of the Medical Department of the United States Army:
“By virtue of his social and professional prominence, his position as teacher and his facile pen, Benjamin Rush had more influence upon American medicine and was more potent in propagation and long perpetuation of medical errors than any man of his day. To him, more than any other man in America, was due the great vogue of vomits, purging, and especially of bleeding, salivation and blistering, which blackened the record of medicine and afflicted the sick almost to the time of the Civil War.”
8
Nonetheless, the tide of public opinion was slowly turning against phlebotomy despite these prominent vocal supporters. Rush, and the practice of bloodletting, were targeted by the satirical journalist William Cobbett, who demonstrated that the mortality rates in Philadelphia
increased after bloodletting was instituted under Rush’s recommendation.
8 Cobbett wrote in the
Porcupine’s Gazette, “The times are ominous indeed when quack to quack cries purge and bleed.” Rush sued for libel and eventually won, but the damage to his reputation was already done.
9
The death of George Washington also ignited a storm of controversy over the use of bloodletting. Washington had developed a severe throat infection after riding around his Mount Vernon estate in the winter. A firm believer in phlebotomy, Washington insisted that his blood be drained. He was bled four times, and it is estimated that he lost between 5 to 9 pints of blood within a few hours.
9 Despite his strong constitution, Washington passed away the next night. Dr. James Craik, Washington’s trusted friend and physician of 40 years, later admitted that the removal of so much blood could have been the cause of his death.
Modern opposition to phlebotomy within the medical community began gaining traction as early as the 18th century with Rene Laennec, the famous French inventor of the stethoscope. In 1834, Pierre Charles Alexandre Louise, regarded by many as “the father of modern epidemiology,” presented statistical evidence that bloodletting was ineffective for treating pneumonia. Through the 1840s to the 1850s, there were intense philosophical battles between the proponents and the skeptics of bloodletting. The most famous of these disputes erupted in Edinburgh between Dr. William P. Alison and Dr. John Hughes Bennett. As these debates raged, the use of phlebotomy at this time depended on a physician’s personal belief about its efficacy. Bloodletting was still used during the American Civil War, where military doctors, overwhelmed by rampant disease and lack of medicines, bled both soldiers and civilians in an attempt to treat them.
Ultimately, however, the studies carried out by Louis Pasteur and Robert Koch conclusively proved the Germ Theory, invalidated the humoral theory of disease, and destroyed the credibility of bloodletting for the treatment of inflammation.
10 Their work ushered in a new scientific, empirically-based method for evaluating the pathophysiology of diseases and the ways to treat them. Despite these advances, advocacy for bloodletting continued into the 20th century. It is remarkable that even William Osler wrote in his 1892 textbook, The
Principles and Practice of Medicine,“During the first 5 decades of this century the profession bled too much, but during the last 5 decades we have certainly bled too little. Pneumonia is one of the diseases in which a timely bleed may save life.” He also advocated bloodletting in arteriosclerosis with acute heart failure, cerebral hemorrhage, emphysema, sunstroke, right-sided heart failure, and systemic hypertension. Even the 1935 edition of his book, edited by Thomas McCrae, included bloodletting as a treatment for pneumonia.
4
CURRENT STATUS OF BLOODLETTING
To the modern public, bloodletting may seem barbaric and archaic, but it continues to be used effectively for a small number of myeloproliferative disorders based on empirical evidence, not – as in the past – on superstition and faith.
10 Currently, phlebotomy is used in the treatment of hemochromatosis and porphyria cutanea tarda (PCT) to help prevent organ damage from the accumulation of iron. Polycythemia vera is also commonly treated with phlebotomy to reduce blood viscosity and prevent thrombotic events.
Recently, the use of leeches has also made a comeback, especially in plastic surgical settings.
Hirudo medicinalis leeches, used in microsurgery and re-implantation operations to enhance blood flow by preventing venous congestion, secrete several biologically active substances such as hyaluronidase, fibrinase, vasodilators, and anticoagulants.
11
Bloodletting continues to be used as an alternative therapy around the world. Cupping is used in traditional Chinese medicine to treat a variety of illnesses.
** Even as recently as 2008, Kashmiri hospitals in Pakistan were applying leeches to patients to treat a range of diseases including heart problems, arthritis, gout, headaches, and sinusitis.
12 Overall, bloodletting has been a common medical practice for centuries and continues to remain relevant today in specific circumstances, despite modern technological advances.
*This dichotomy endures in the British tradition of addressing surgeons as "Mister," rather than "Doctor."
**Editor’s Note: Television viewers of the 2016 Rio Olympics were at first mystified, and then amused, by the circular lesions often seen on swimmers, notably Gold Medalist Michael Phelps (Fig. 3).
 Fig. 3. Gold Metalist Michael Phelps, in this Reuters photo by Dominic
Fig. 3. Gold Metalist Michael Phelps, in this Reuters photo by Dominic
Ebenbichler, is shown competing at the 2016 Olympics in Rio de Janeiro,
Brazil, with red cupping marks on his shoulder.
They were also used by other athletes, but were not as visible for obvious reasons. Their popularity reflected the belief that dry cupping can improve blood flow, provide deep massage, relieve pain and inflammation, and accelerate recovery from strenuous exercise. None of these claims is substantiated by controlled studies, since it is impossible to eliminate the powerful placebo effect of such a tactile and visible intervention.
An interesting side story with geopolitical implications was reported by Foreign Policy magazine online. Russian State TV Rossiya-24 inadvertently gave cupping a boost in a special program on Aug. 9, 2016, by claiming that cupping is a “muscle relaxing routine” that can help athletes recover more quickly from strenuous exercise. They asserted that it is tantamount to doping, and gave Michael Phelps an unfair advantage. But while the International Olympic Committee could dismiss such complaints as mere Russian blather, the public could be excused for wondering why the Russians would bother to complain about it if it had no effect.
Actually, it seems that in a convoluted way the Russians were trying to reverse the Olympic ban on Russian athletes who took meldonium. By claiming that cupping and meldonium were similarly effective for their respective purposes, the Russians wanted both held to the same standard. If cupping is allowed, why not meldonium?
In the final analysis, if athletes want to inflict cupping on themselves, and it has no significant physiological effect, it is tempting to dismiss the practice as a private matter. Unfortunately, publicity about its use by athletes and other celebrities grants placebos a veneer of legitimacy. (See “Please Michael Phelps, Stop Cupping,” by James Hamblin, M.D., in The Atlantic:
http://www.theatlantic.com/health/archive/2016/08/phelps-cupsanity/495026/)
Cupping can have all the usual disadvantages of placebos – wasting time and money, delaying legitimate therapy, and in some cases, even causing actual harm.
REFERENCES
1. Kuriyama S. Interpreting the history of bloodletting. Journal of the History of Medicine and Allied Sciences, 1995; 50(1), 11-46. Retrieved from SCOPUS database.
2. Papavramidou N, Thomaidis V, Fiska A. The ancient surgical bloodletting method of arteriotomy. J Vasc Surg. 2011; 54(6): 1842-1844. doi:
http://dx.doi.org.proxy1.lib.tju.edu/10.1016/j.jvs.2011.05.100
3. Davis A, Appel T. Bloodletting instruments in the national museum of history and technology. Smithsonian Studies in History and Technology. 1979; 28:41
4. DePalma RG, Hayes VW, Zacharski, LR. Bloodletting: Past and present. Journal of the American College of Surgeons. 2007; 205(1): 132-144. doi:
http://dx.doi.org.proxy1.lib.tju.edu/10.1016/j.jamcollsurg.2007.01.071
5. van Tellingen C. Bleeding-edge technology in cardiology - or the mixed blessings of phlebotomy throughout the ages. Netherlands Ht J. 2010; 18(4): 218-222. Retrieved from SCOPUS database.
6. Mattern S. Galen and his patients. Lancet. 2011; 378(9790): 478-479. doi:
http://dx.doi.org.proxy1.lib.tju.edu/10.1016/S0140-6736(11)61240-3
7. Falagas ME, Zarkadoulia EA, Samonis G. Arab science in the golden age (750–1258 C.E.) and today. The FASEB Journal. 2006; 20(10): 1581-1586. doi:
10.1096/fj.06-0803ufm
8. North RL Benjamin Rush, MD: Assassin or beloved healer? Proceedings of Baylor U. Med Ctr. 2000; 13(1): 45-49.
9. Thomas DP. The demise of bloodletting. J Royal Coll Phys Edinburgh. 2010; 44(1): 72-77.
10. Jhang JS, Schwartz J. Phlebotomy or bloodletting: From tradition to evidence-based medicine. Transfusion. 2012; 52(3): 460-462. doi:10.1111/j.1537-2995.2012.03548.x
11. Kraemer BA, Korber KE, Aquino TI, Engleman A. Use of leeches in plastic and reconstructive surgery: a review. J Reconstr Microsurg. 1988; Oct;4(5):381-6.
12. Parapia LA. History of bloodletting by phlebotomy. Br J Haematol. 2009.143(4): 490-495.