
Summer 2016 - Vol. 11, No. 2
Evolution of a DaVinci Robotic Program
George J. Olt, M.D.
LGHP — Gynecologic Oncology
HISTORY
The DaVinci robot (Intuitive Surgical) was named after the first robot, thought to have been designed by Leonardo DaVinci in 1495. As one would expect, due to the lack of necessary technology, no functional surgical robots appeared until the late 20th century. At that time, the Department of Defense collaborated with the Stanford Research Institute in an unsuccessful attempt to develop a remote battlefield surgical robot. Although it was not successful, Intuitive Surgical licensed this early robot, known as the SRI Green Telepresence Surgery System. This system underwent extensive redesign and was reintroduced as the DaVinci Robotic System, which obtained FDA approval in 2000. By June 30, 2014, 2,153 units were in use in the United States.
1
Despite the rapidly growing interest in the use of robotic surgery for various surgical procedures, its use remained controversial, primarily due to concerns about cost and safety. Currently, cost issues remain contentious depending on one's accounting perspective, but there are benefits that cannot be ignored, including enhanced patient safety, shorter hospitalizations, and more rapid return to work. In gynecology, a recent publication demonstrated decreased intraoperative and postoperative complication rates compared with other methods of hysterectomy.
2 Since there have been numerous papers published elsewhere that deal with the cost/safety controversies, this article will focus on the advantages that have resulted from the evolution of robotic gynecologic surgery within the Lancaster General Hospital System.
TRENDS IN SURGICAL APPROACHES TO GYNECOLOGICAL PROCEDURES
In 2008, when Lancaster General Hospital acquired its first DaVinci Robot, most procedures were done with open techniques. Because of the technical difficulty of traditional laparoscopic (straight stick) hysterectomy, only one gynecologic surgeon was performing that procedure, and only two were performed that same year.
Traditional straight stick laparoscopic hysterectomy is associated with several problems that limit its utility. As the patient's body mass index increases, surgery becomes more difficult. In a Gynecologic Oncology Group Study, one half of endometrial cancer patients with a BMI of 35 or greater undergoing lymph node sampling required an open procedure to complete the operation, resulting in increased morbidity.
3 This issue is particularly problematic for patients with endometrial cancer because morbid obesity is their primary risk factor for developing the disease. Of interest, Pennsylvania has the highest per capita rate of endometrial cancer in the United States. The mean BMI of Lancaster General Health patients with endometrial cancer is 48.2.
Other problems associated with traditional straight stick laparoscopy include reliance on the experience level of an assistant; use of a two dimensional camera which reduces depth perception; and most importantly, the design of unwristed instruments that limits their mobility and dexterity. Therefore, the learning curve for traditional straight stick laparoscopic surgery is actually steeper than for the robotic-assisted approach.
After the DaVinci robot was obtained in 2008, one robotic-assisted hysterectomy was performed that year, but adaptation to robotic-assisted surgery was rapidly achieved by surgeons in the divisions of gynecology and gynecologic oncology. (Table 1)
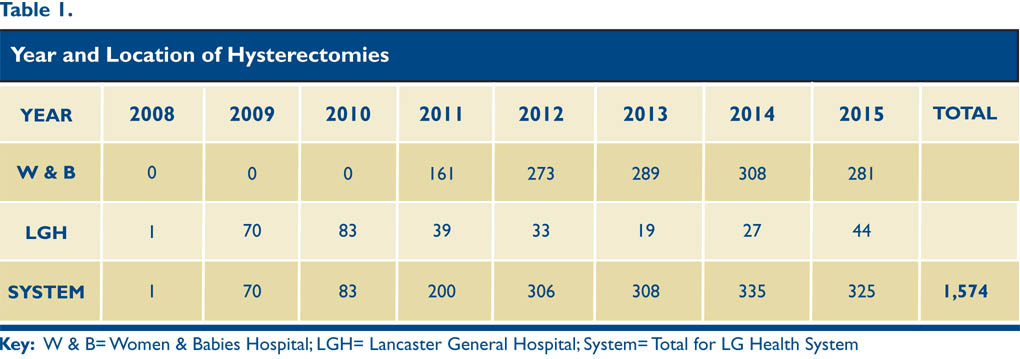
By 2013, 14 gynecologists were certified to perform robotic-assisted surgery, with the result that the ratio of open to minimally invasive procedures decreased dramatically. (Figure 1).
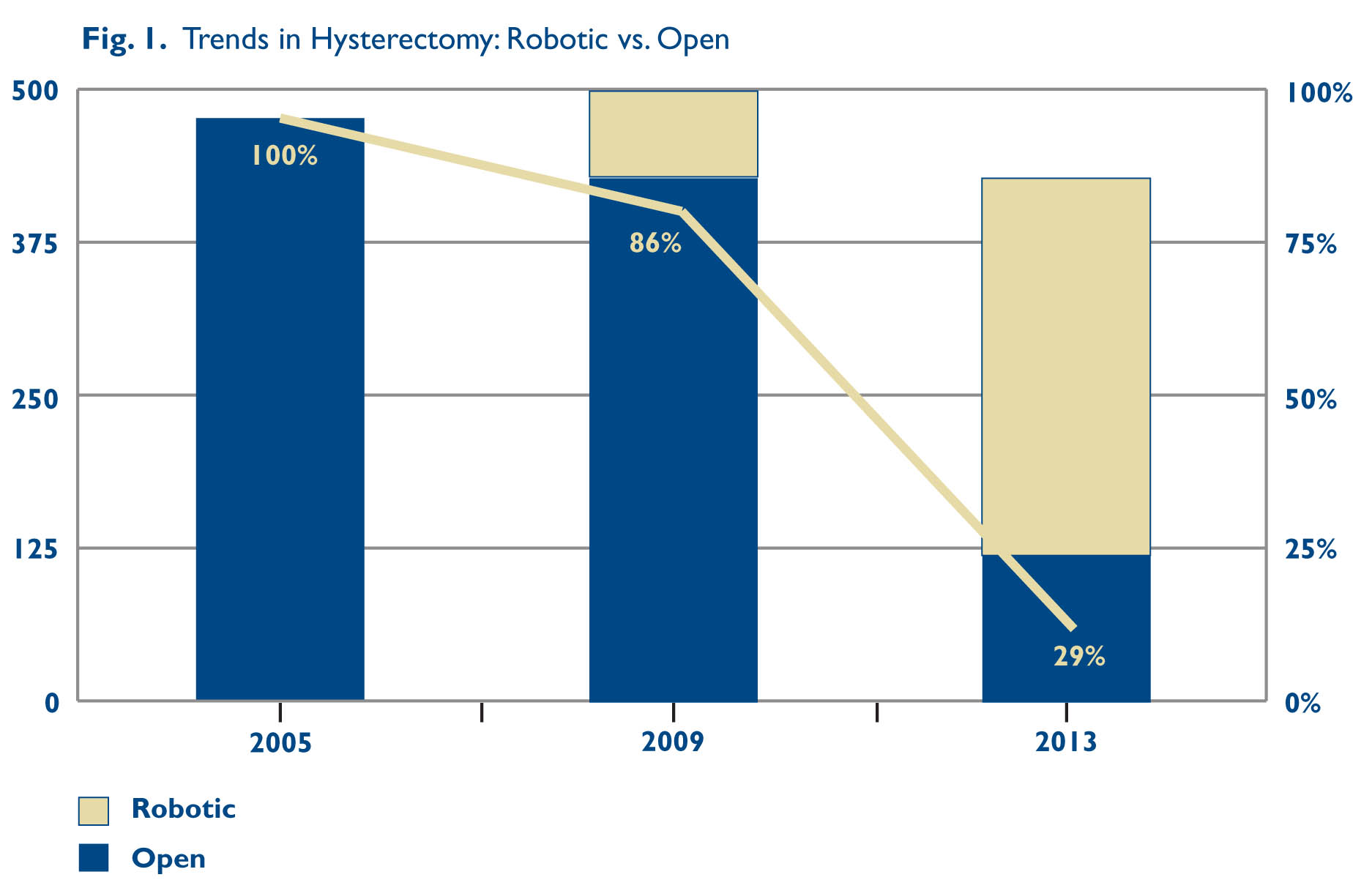
The benefits of the increasing percentage of minimally invasive hysterectomies include shorter hospital stays, fewer lost work days, decreased surgical site infections, and increased safety. Our standard length of stay for robotic hysterectomy is same-day/overnight, and for an open case two days post op. Return to work is recommended in two weeks after a robotic procedure, vs. six weeks after an open operation.
ADVANCES IN SURGERY: COMBINED BOWEL AND GYNECOLOGIC TECHNIQUES
The next stage in the development of robotic techniques for gynecology was the progression from simple robotic hysterectomy to more difficult combined cases, but this advance required new technology. The new Xi model of the Da Vinci robot was introduced in 2015. Numerous modifications that provided enhanced performance of the robotic arms allows the Xi robot to be more easily docked and undocked, which facilitates repositioning for enhanced access to the upper abdomen and pelvis. It is now possible to perform minimally invasive combined colon and gynecological procedures, as exemplified below.
A patient who was a member of a family with Lynch Syndrome, which manifests as a genetic predisposition to colon and endometrial cancers, required risk reduction surgery. Traditionally, these patients would undergo a total colectomy with rectal preservation coupled with a total abdominal hysterectomy through a large midline incision. Instead, this patient was offered a robotic-assisted approach.
The operation was initiated by placing four 8-millimeter trocars transversely slightly above the umbilicus. The patient was placed in the left lateral position, which allowed take down of the right colon and hepatic flexure mesenteries. The robot was undocked and the patient was placed in steep Trendelenberg to facilitate access to the pelvis. A robotic total laparoscopic hysterectomy and bilateral salpingo-oophorectomy was performed, but the vaginal cuff was not closed. Again, the robot was undocked and the patient was placed in a right lateral position for takedown of the left colon and splenic flexure. The distal ileum and rectum were stapled and divided. The colon was removed through the vagina. The distal ilium was brought through the vagina, an end-to-end stapler (EEA) anvil was placed, and the ileum closed. The EEA stapler was then inserted into the rectum and joined to the previously placed anvil utilizing laparoscopy. After joining the ilium and rectum, the vagina was closed robotically.
The major drawback of this operation was the need for docking and undocking of the robot several times during the procedure to allow access to different areas of the abdomen and pelvis. Fortunately, an operating table has been developed which can be computer controlled in tandem with the robot to allow repositioning of the patient without requiring undocking. This modified table facilitates robotic approaches to gynecologic surgery that require access to the upper abdomen, such as ovarian staging or splenectomy associated with ovarian cytoreduction (tumor debulking for advanced ovarian cancer).
Another example of combined minimally-invasive bowel and gynecologic surgery involved take down of an end colostomy in the descending colon and re-anastomosis to the distal rectum aided by hysterectomy for exposure. The patient had multiple previous abdominal operations as well as abdominal infection, resulting in a hostile pelvis with multiple adhesions. Furthermore, a previous incisional hernia repair utilizing mesh became infected and required removal of the graft. Another midline incision would have likely resulted in a recurrent hernia, which could be avoided by a laparoscopic approach.
The operation began with take down of the stoma allowing direct visualization of the peritoneal cavity. Adhesions of the small bowel to the anterior abdominal wall were lysed sharply allowing safe placement of four 8-millimeter trocars. The patient was placed in steep Trendelenberg position and the robot was docked. Numerous loops of the small bowel adherent to the pelvis were mobilized to expose the uterus and adnexa, followed by a total laparoscopic hysterectomy and bilateral salpingo-oophorectomy to allow access to the distal rectum. The distal rectum was mobilized. An EEA stapler anvil was placed in the proximal colon, which was then stapled, and the stoma was removed. The colon was re-anastomosed utilizing laparoscopic guidance. The stoma and trochar sites were closed.
SENTINEL LYMPHADENECTOMY
Several types of cancer associated with lymph node metastasis are surgically managed with sampling of sentinel lymph nodes utilizing a radioactive isotope and a visual dye for identification. This more limited lymphadenectomy results in decreased surgical morbidity and lymphedema, but until recently it was not feasible for patients with endometrial cancer undergoing laparoscopic surgery. The Xi robot is equipped with a near infrared light source and camera that detects fluorescence. Indocyanin is injected into the uterine cervix immediately prior to surgery. When the nodal-bearing areas are exposed, the first node in the area of lymphatic drainage can be identified by its apple green glow and it can be removed for sampling.
SUMMARY
It is clear that robotic surgery has had a major impact on gynecologic surgery. The increase in minimally invasive surgery and concomitant decrease in open surgery has resulted in shorter hospitalizations and recovery times. Post-operative infections are very rare and complications appear less frequently. Most laparoscopy patients do not need narcotic analgesia post-operatively due to the small incisions. Robotic surgery is particularly helpful for obese patients because the ability to visualize the pelvis more closely makes surgery easier for the experienced surgeon and avoids the need for an open incision with its potential complications in these patients. Robotic technology and techniques are advancing far more rapidly than standard laparoscopy and will be the wave of the future.
REFERENCES
1. daVinci Products FAQ. Intuitive Surgical.
2. Lim PC, Crane JT, English EJ, et al. Multicenter analysis comparing robotic, open, laparoscopic, and vaginal hysterectomies performed by high-volume surgeons for benign indications. Int J Gynecol Obstet. In press. 2016.
3. Walker JL, Piedmont MR, Spiritos NM. Laparoscopy compared with laparotomy for comprehensive staging of uterine cancer: GOG Study LAP2. J Clin Oncol 2009; 27 (32) :5331-6.