 Click to Print Adobe PDF
Click to Print Adobe PDF
Winter 2015 - Vol. 10, No. 4
|
Evolving Treatment Strategies for Post-Concussion Syndrome
Jon E. Bentz, Ph.D., ABN
Manager, Lancaster General Health Physicians-Neuropsychology
Dale R. Walton, P.T., N.C.S.
Lead Therapist, LG Health Vestibular and Post-Concussion Programs
|
  |
INTRODUCTION
The identification and treatment of concussive brain injuries have been prominent topics over the past decade and remain major areas of research, with much learned and much changed over time. As with most medical conditions, treatments began with a simplistic general approach, and gradually became more refined, individualized, and specific.
Treatment of post-concussion syndrome at LGH has reflected that progress, and management of patients has become steadily more individualized. Since the initial symptoms of post-concussion syndrome vary considerably, optimally effective treatment strategies must be individualized and specific not only to the patients’ symptoms, but also to their psychological characteristics and lifestyle.
Fifteen years ago, patients with post-concussion syndrome whose recovery was prolonged by persistent symptoms received either limited treatment or none at all. Patients were left to endure their symptoms while awaiting spontaneous resolution. Treatment typically involved rest and perhaps medications for symptomatic relief of headache, nausea, or dizziness. Such general and non-specific treatments only superficially addressed disturbances in performance at work or in school, in relationships, and in mood. Return to athletics was guided by criteria based on whether there had been loss of consciousness, and on the duration of any post-trauma amnesia, regardless of the presence of symptoms.
Eventually, however, these criteria and treatment guidelines were shown to have limited predictive value with respect to persistence of symptoms and duration of recovery. Studies revealed that average duration of symptoms was much longer than previously assumed, and there were individual differences in rates of recovery.
In 2008 and 2009 we discussed our understanding and management of post-concussion syndrome at that time.1,2 In this article we update our understanding of these injuries, and provide an overview of our current approach to their treatment at LGH.
CONCUSSION AND POST-CONCUSSION SYNDROME: Biomechanical Forces, Metabolic Dysfunction and Psychological Factors
Concussion is caused by direct or indirect biomechanical forces, including linear acceleration-deceleration and rotational forces acting on the brain. These forces result in a neuro-metabolic energy crisis in the brain, with increases in levels of extracellular potassium and intracellular sodium and calcium.3 Since social and psychological factors may also impact symptoms of post-concussion syndrome, theories on its causes see it as multifactorial, resulting from any combination of metabolic dysfunction, structural damage below the sensitivity of traditional imaging, and social/psychological factors.
However, since patients with chronic pain and psychiatric disorders often present with similar complaints, symptoms of ordinary headaches, fatigue, cognitive issues, and disturbances of emotion or sleep may be misattributed to a head injury.4,5
RISK FACTORS FOR PROTRACTED RECOVERY
Studies suggest that symptoms resolve within three weeks in 80% of individuals who sustain a concussion. Prolonged symptoms are associated with various risk factors including gender (females are more vulnerable to sustaining a concussion and having more protracted symptoms), and age (younger individuals are more vulnerable and recover more slowly). Time to complete recovery is also prolonged in individuals with a history of concussion, developmental disorders, learning disability, migraine headaches, or psychiatric disorders. More recently, a history of motion sensitivity (e.g. motion sickness, car sickness) or oculomotor disorders (e.g. strabismus) have been suggested as possible risk factors, though the association has not been definitively demonstrated.6
Other symptoms associated with prolonged recovery include: dizziness immediately post injury,7 posttraumatic migraines with nausea, photo – or phono – sensitivity within the first week,8 multi-system symptoms, or more severe cognitive compromise.
A FEW WORDS ABOUT REST FOLLOWING CONCUSSION
For the last decade the standard of care after a concussion has been rest until the patient is symptom free. This recommendation originated from a landmark article published in the Journal of Athletic Training in 2001 which reviewed over 100 basic science and clinical articles that looked at the neuro-metabolic changes after traumatic brain injury. Notably, many of the studies had used animal subjects.3 The basic conclusion was that there are significant changes in cerebral glucose metabolism in head-injured patients for up to one month post injury. Bergsneider et al. found a reduction of cerebral glucose utilization up to four weeks post injury in a population of mild and severe brain-injured patients.9 Vagnozzi et al. found that concussed athletes who reported resolution of symptoms in 3–15 days showed metabolic abnormalities on magnetic resonance spectroscopy that peaked at three days and resolved by 30 days post injury.10 The medical community assumed that activity during this period of recovery would be detrimental to the overall recovery of the patient, in addition to the fact that return to play might increase the risk of repeat concussion.
Our experience confirms the prevalence of these practices, as many of the patients referred to our post-concussion program had been told to rest for up to several months until all their symptoms resolved. We have observed that these patients often have secondary symptoms of depression and anxiety, and their behavior often reflects a belief that they won’t recover. These secondary complaints seem more evident in athletes – whether they are competitive or casual. These findings indicate that prolonged enforced sedentary rest, and removal from physical activity and social interaction, can result in depression, anxiety, headaches and other secondary symptoms that can mimic the symptoms associated with concussion. Teens and athletes are especially vulnerable to the adverse effects of prolonged restrictions. Enforced rest (bed rest) of only three days causes neuro-hormonal modifications in the response to exercise that are most significant in endurance athletes.11
In 2009 a prospective study looked at over 635 concussed high school and college athletes of whom 60% were told to rest until they were symptom-free and 40% were not told to do so. Clinical outcomes were assessed with an inventory of symptoms and tests of neuropsychological function and balance. There were no significant differences in the outcomes for the two groups, whereas the rest group had a higher rate of concussions when they did return to play.12
This year, a randomized controlled study confirmed that prolonged rest can result in more protracted recovery.13 A group of 11 – 22 year old patients who presented to an emergency department with concussions were randomized to a regimen of either strict rest for five days or rest for one to two days followed by a stepwise return to usual activity. Symptoms were recorded by the patients daily; neurocognitive and balance testing were performed on days 3 and 10 post injury. There were no differences in the outcomes for the two groups, but the five-day rest group reported more post-concussive symptoms and overall their symptoms resolved more slowly.
There has never been any evidence to support rest after a concussion for more than a few weeks. Current evidence recommends no more than three days of enforced rest followed by a planned graduated return to activity, since complete rest exceeding three days is probably not helpful. Gradual resumption of pre-injury activities, with the exception of activities that have a high risk of exposure to MTBI (Mild Traumatic Brain Injury), should begin as soon as tolerated. Indeed, supervised exercise may benefit patients with persistent symptoms.14 Nonetheless, it must be emphasized that the rule still stands that athletes with symptoms should not return to contact sports until full, complete resolution of post-concussive symptoms is definite.
POST-CONCUSSION SYNDROME AS A HETEROGENEOUS DISORDER
Traditionally, symptom clusters were described as being in various domains termed somatic (e.g. headache, nausea, dizziness, visual disturbance, fatigue), cognitive, emotional and sleep disturbance. Kontos et al. identified a more common or universal symptom picture, consistent with the above symptom clusters, shortly after and lasting for approximately the first week post injury. More specific symptom clusters tend to appear approximately one week post injury.6
A recent approach proposed by Collins et al. is to individualize treatment according to specific post-concussion trajectories or symptom clusters. Primary, secondary, and other trajectories are determined according to the patient’s constitutional risk factors, subjective symptom complaints, vestibular and ocular screening tests, and neurocognitive function. Efficacy of treatments is enhanced when the best-fit trajectories guide the intervention plan.15
As Collins et al. emphasize, effective treatment calls for interventions specific to the patients and their symptoms. Concussions and post-concussion syndromes should be viewed as heterogeneous in nature; a single approach to treatment is likely to be ineffective and/or inefficient.
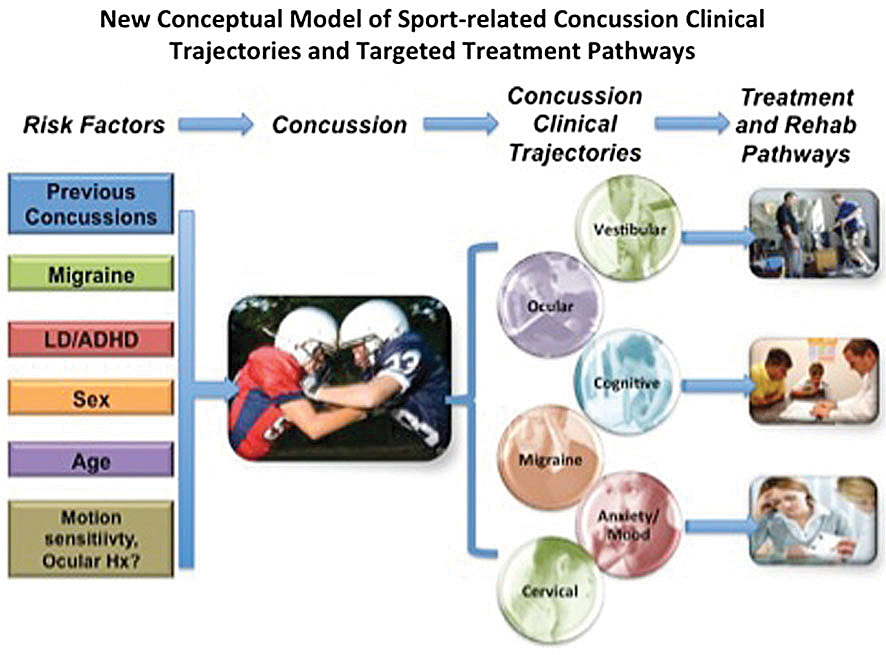
Fig. 1. From Collins et al.15
MULTI-SPECIALTY, INTERDISCIPLINARY APPROACH TO ASSESSMENT AND TREATMENT
It is clear from the above that patients who present with protracted symptoms including, but not limited to, headaches and dizziness, cognitive and memory deficits, sleep disturbances, or exacerbation of their symptoms with cognitive or physical effort should be referred to health professionals trained specifically in the rehabilitation of concussions. Prolonged and varied symptoms indicate the need for a multidisciplinary approach because they are a potential manifestation of continued metabolic abnormalities, autonomic dysfunction, cervical injury, post-traumatic migraine headache, vestibular dysfunction, visual dysfunction, psychological and social factors, or a combination of conditions.16
Our program at LGH utilizes an interdisciplinary approach that includes the patient’s own physicians as well as neuropsychologists, physical therapists, occupational therapists, and speech pathologists. Involvement of specialists in treatment of oculomotor disorders may also be indicated.
Also, as early as possible after injury the patient should be educated about the pathophysiology, symptoms, and usual course of recovery after concussion, all done in a manner that reinforces an expectation of full recovery and provides behavioral management strategies that foster recovery. While there are no definitive rules for when to refer for treatment, vestibular, oculomotor, and cognitive symptoms persisting beyond three weeks are a reasonable guideline. Best practice includes development of the most appropriate treatment plan based on initial evaluations by a physician, a neuropsychologist, and a physical therapist with expertise in concussion management.
a. Neuropsychology
A recent meta-analysis of the literature confirmed that symptoms can be improved, and the pathophysiology and course of post-concussion syndrome can be altered by early psychoeducational intervention; by review of the typical recovery course; by provision of reassurance; by reinforcing the expectation of full recovery; by normalizing symptoms; and by correcting any misconceptions a patient might have (e.g. an expectation of prolonged or incomplete recovery or having sustained a more malignant injury).14 Implementation of compensatory behavioral strategies to address difficulties with aspects of cognition (attention, memory, slowed processing, executive functioning), or to compensate for functional deficits may be indicated. Optimizing the patient’s sense of competency and empowerment, and assisting the patient in coping with deficits helps to optimize recovery and lessen symptom duration. Regulation of lifestyle behaviors, including diet, hydration, physical and cognitive activity, sleep, and stress management, can also help attenuate symptoms.
Psychological intervention in the form of cognitive behavioral therapy has also been shown to be effective in improving coping and adjustment while symptoms persist.17 Integration of treatment for cognitive impairments, somatic symptoms, and vestibular and oculomotor symptoms contributes to the development of treatment strategies and approach. Behavioral pain management strategies and biofeedback training for headache are also within the realm of neuropsychological intervention.
b. Physical Therapy
Physical therapists address many of the symptoms that are typically protracted, including exercise intolerance, headaches, vestibular symptoms (dizziness and intolerance to motion), and some oculomotor dysfunction. The physical therapist should have specialized training and experience in the assessment and treatment of vestibular dysfunction.
It is hypothesized that concussion may incite dysfunction of the regulatory system responsible for cerebral blood flow.18 Controlled aerobic exercise (after exercise capacity has been established) can assist recovery from post-concussion syndrome.19 Aerobic exercise two to three weeks after TBI (Traumatic Brain Injury) has been shown to upregulate brain-derived neurotropic factor, and is associated with an improvement in cognitive performance.20 TBI may also alter regulation of the autonomic nervous system. Athletes with TBI, including concussion, have been observed to have high resting heart rates and lower HR variability.21,22 which may provide an alternate explanation of why some concussed athletes report increased symptoms with physical exertion. Progressive rehabilitation with controlled aerobic exercise has been demonstrated to restore normal cerebral blood flow on functional MRI and reduce symptoms on treadmill testing.23
Cervical issues need to be fully addressed whether there is a headache or not. In many of these patients, but particularly those returning to impact sports, a program that strengthens cervical stability is appropriate and has been shown to reduce the risk of recurrent concussions.
These patients commonly have persistent dizziness and motion sensitivity, either due to persistent metabolic dysfunction or to micro trauma at the level of the vestibular nuclei in the ponto-medullary area. Trauma to this area may also contribute to autonomic dysfunction. Some of the common deficits in these patients are in the smooth pursuit, or saccadic eye systems. Concussed patients often exhibit very poor near-point convergence and have difficulty coordinating their eye movements. Mucha et al. recently developed and published “VOMS” (Visual Oculomotor Screen), a tool to detect oculomotor abnormalities by observing symptoms while the subject performs six oculomotor skills. Elevation of any of four symptoms triggers more advanced testing either by a Vestibular/Neuro Physical Therapist or by a vision professional.24
Another source of dizziness and motion sensitivity can be related to lack of gaze stability caused by deficits in the central vestibular system or the peripheral system. BPPV (Benign Paroxysmal Positional Vertigo) is always screened for and promptly treated when found. If gaze stability is impaired, a peripheral source such as labyrinthine concussion without fracture may be to blame. Treatment includes graded exercises for gaze stability and sensory organization with and without head motions. True balance deficits are rarely seen in these patients and perceived balance problems are usually vestibular in nature. Computerized Dynamic Posturography is used to define any balance deficits and to guide treatment that is specific to the impairment. When oculomotor symptoms persist after initial treatment or there are severe deficits in near-point convergence or the binocular vision system, or whenever a skew deviation or tropia is noted, referral is made to a neuro ophthalmologist or behavioral optometrist.
c. Speech Pathology
Speech therapy or other cognitive rehabilitation specialists work with patients who have prolonged cognitive complaints. Intervention is directed at the development of compensatory strategies and skills to improve function and lead to successful engagement in activities. Strategies for optimizing processing of information (e.g. elaboration, rehearsal, visual imagery, multi-modality processing, self-cueing) and employment of environmental modifications and external memory aids are often utilized.
d. Occupational Therapy
Occupational therapists work with patients to attenuate the functional impact of visual problems that impact reading or computer work. They may also assist patients in compensating for compromised cognition; developing strategies to manage daily routines; planning, organizing and managing time; and paying attention to detail. Occupational therapists can also employ other neuro/behavioral interventions to help with stress management.
CONCLUSIONS
Over the last two decades our understanding of the identification, pathology, and treatment of post-concussion syndrome has advanced considerably, and it is critical to change our practices in light of new findings. In particular, we now know that a short rest period followed by step-wise return to activity facilitates faster recovery in certain patients. Also, vestibular and aerobic exercise therapies are effective in the rehabilitation of patients with persistent symptoms.
Overall, optimal treatment requires an individualized treatment plan based on the patient’s symptoms, psychology, and lifestyle factors. The complexity and scope of post-concussive symptoms requires an integrated team that includes various specialists. Our program at LGH emphasizes initial evaluation by a patient’s physician, a neuropsychologist, and a physical therapist, all coordinating to develop the most appropriate treatment plan. Referrals to other disciplines are then made as indicated.
REFERENCES
1. Bentz JE, and Purzycki EJ: Concussion: Not so minor an injury; Incidence, pathophysiology, risks and management. J Lanc Gen Hosp. 2008; 3: 84-90.
2. Bentz JE. Concussion (2): Not so minor an injury; Incidence, pathophysiology, risks and management. J Lanc Gen Hosp. 2009; 4: 71-73.
3. Giza CC, Hovda DA. The neurometabolic cascade of concussion. J Athl Train 2003; 36:228–235
4. Hou R, Moss-Morris R, Peveler R, et al. When a minor head injury results in enduring symptoms: a prospective investigation of risk factors for postconcussional syndrome after mild traumatic brain injury. J Neurol Neurosurg Psychiatry 2012; 83:217.
5. Meares S, Shores EA, Taylor AJ, et al. Mild traumatic brain injury does not predict acute postconcussion syndrome. J Neurol Neurosurg Psychiatry 2008; 79:300.
6. Kontos AP, Elbin RJ, Schatz P, Covassin T, Henry L, Pardini J, Collins MW (2012) A revised factor structure for the post concussion symptom scale (PCSS): baseline and post-concussion factors. Am J Sports Med 2012; 40:2375–2384
7. Lau B, Lovell MR, Collins MW, Pardini J. Neurocognitive and symptom predictors of recovery in high school athletes. Clin J Sport Med 2009; 19:216–221
8. Lau BC, Kontos AP, Collins MW, Mucha A, Lovell MR. Which on-field signs/symptoms predict protracted recovery from sport-related concussion among high school football players? Am J Sports Med 2011; 39:2311–2318
9. Bergsneider M, Hovda DA, Lee SM, Kelly DF, et al. Dissociation of cerebral glucose metabolism and level of consciousness during the period of metabolic depression following human traumatic brain injury. J of Neurotrauma 2000; 17:389-401
10. Vagnozzi R, Signoretti S, Cristofori L, ALessandrini F, et al. Assessment of metabolic brain damage and recovery following mild traumatic brain injury: a multicenter, proton magnetic resonance spectroscopic study in concussed patients. Brain 2010; 133:3232-3242
11. Smoranwinski J, Nazar K, Kaciuba-Uscilko H, et al. Effects of 3-day bed rest on physiological responses to graded exercise in athletes and sedentary men. J of Applied Physiology 2001; 91:249-257
12. McCrea M, Guskiewicz KM, Randolph C, et al. Effects of a symptom-free waiting period on clinical outcome and risk of reinjury after sport related concussion. Neurosurgery. 2009; 65:876-882
13. Thomas DG, Apps JN, Hoffman RG, McCrea M, et al. Benefits of strict rest after acute concussion: a randomized controlled trial. Pediatrics 2015; 135:213
14. Silverberg ND, Iverson GL. Is rest after concussion “the best medicine?”: recommendations for activity resumption following concussion in athletes, civilians, and military service members. J of Head Trauma Rehabilitation 2013; 28:250-259
15. Collins MW, Kontos AP, Reynolds E, Murawski CD, Fu FH. A comprehensive, targeted approach to the clinical care of athletes following sport-related concussion. Knee Surgery, Sports Traumatology, Arthroscopy 2014; 22:235-246
16. Leddy JJ, Sandhu H, Sodi V, Baker JG, Willer B. Rehabilitation of Concussion and Post-concussion syndrome. Sports Health: A Multidisciplinary Approach 2013; 4:147-154
17. Al Sayegh A, Sandford D, Carson AJ. Psychological approaches to treatment of postconcussion syndrome: a systematic review. J Neurol Neurosurg Psychiatry 2010; 81:1128.
18. DeWitt DS, Prough DS. Traumatic cerebral vascular injury: the effects of concussive brain injury on the cerebral vasculature. J Neurotrauma. 2003; 20:795–825
19. Leddy JJ, Kozlowski K, Donnelly JP, et al. A preliminary study of subsymptom threshold exercise training for refractory post-concussion syndrome. Clin J Sport Med 2010; 20:21-27
20. Griesback GS, Hovda DA, Molteni R, et al. Voluntary exercise following traumatic brain injury: brain derived neurotrophic factor upregulation and recovery of function. Neuroscience 2004; 125:129-139
21. Visttisen ST, Hansen TK, Jensen J, et al. Heart rate variability in neurorehabilitation patients with severe acquired brain injury. Brain Injury 2014; 28:196-202
22. Perkes IE, Baguley IJ, Nott MT, et al. A review of paroxysmal sympathetic hyperactivity after acquired brain injury. Annals of Neurology 2010; 68:126-135
23. Leddy JJ, Cox JL, Baker JG, et al. Exercise treatment for postconcussion syndrome: a pilot study of changes in functional magnetic resonance imaging activation, physiology and symptoms. Journal of Head Trauma Rehabilitation 2013; 28:241- 249
24. Mucha A, Collins MW, Elbin RJ, et al. A brief vestibular/ocular motor screening (VOMS) assessment to evaluate concussions. The Amer J Sports Med 2014; 42:2479-2486