 Click to Print Adobe PDF
Click to Print Adobe PDF
Fall 2015 - Vol. 10, No. 3
|
Non-Alcoholic Liver Disease:
Today's Epidemic?
Lorenzo Galindo, M.D., F.A.C.P.
Chair and Medical Director, LGH Department of Pathology
Professor of Pathology, Drexel University College of Medicine
Emma Furth, M.D.
Professor of Pathology and Laboratory Medicine,
University of Pennsylvania Perelman School of Medicine
Director, Gastrointestinal and Liver Pathology Fellowship Program
|
  |
BACKGROUND
Non-alcoholic fatty liver disease (NAFLD) is a chronic liver disease that is rapidly increasing in incidence and is currently the most common cause of liver disease worldwide. Its distribution is tightly linked to diabetes and obesity, two diseases that have reached epidemic proportions in many countries (Fig. 1), which is why lifestyle intervention is a key factor in managing patients with NAFLD.
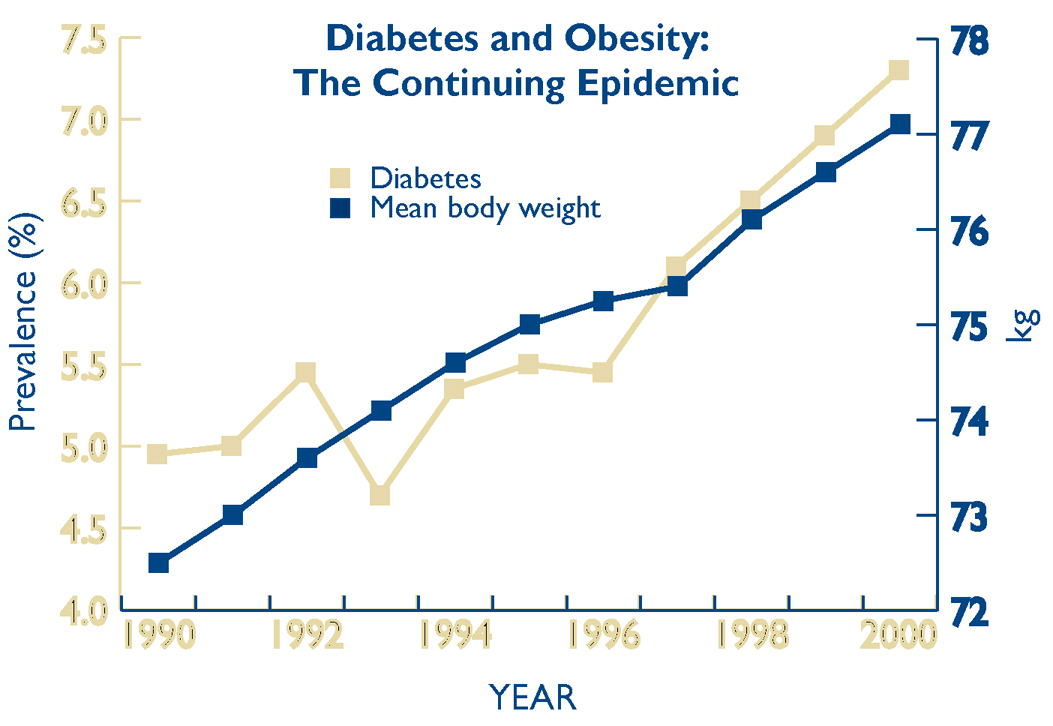
Sources: Mokdad AH et al. Diabetes Care. 2000;23:1278-83. Mokdad AH et al. JAMA. 1999;282: 1519-22. Mokdad AH et al. JAMA. 2001:286;1195-200.
Non-alcoholic fatty liver disease is the result of the accumulation of lipid vacuoles in the cytoplasm of hepatocytes in individuals without a history of alcohol consumption, and it is characterized by the presence of histopathologic lesions that are similar to, if not exactly the same as, those seen in the context of alcoholic liver disease. The terminology was first introduced by Ludwig in 19801 and encompasses a spectrum of histopathologic changes that range from pure steatosis of the liver to steatohepatitis with inflammation and fibrosis, leading to cirrhosis and in some cases to hepatocellular carcinoma. Cirrhosis is the third leading cause of death in patients with NAFLD and is rapidly becoming a leading indication for liver transplantation.
TERMINOLOGY
(from 2012 Practice Guidelines of the Am. Assoc. for the Study of Liver Disease [AASLD)
Non-alcoholic Fatty Liver Disease (NAFLD): Encompasses the entire spectrum of fatty liver disease in individuals without significant alcohol consumption, ranging from fatty liver to steatohepatitis and cirrhosis.
• Non-alcoholic Fatty Liver (NAFL): Presence of hepatic steatosis with no evidence of hepatocellular injury in the form of ballooning of the hepatocytes or no evidence of fibrosis. The risk of progression to cirrhosis and liver failure is minimal.
• Non-alcoholic Steatohepatitis (NASH): Presence of hepatic steatosis and inflammation with hepatocyte injury (ballooning) with or without fibrosis. This can progress to cirrhosis, liver failure, and rarely liver cancer.
• NASH Cirrhosis: Presence of cirrhosis with current or previous histological evidence of steatosis or steatohepatitis.
• Cryptogenic Cirrhosis: Presence of cirrhosis with no obvious etiology. Patients with cryptogenic cirrhosis are heavily enriched with metabolic risk factors such as obesity and metabolic syndrome.
• NAFLD Activity Score (NAS): An unweighted composite of steatosis, inflammation, and ballooning scores. It is a useful tool to measure changes in liver histology in patients with NAFLD in clinical trials.
DEFINITIVE DIAGNOSIS
NAFLD is defined by the presence of hepatic steatosis either by imaging or histology in a patient without significant alcohol consumption, use of steatogenic drugs, or hereditary disorder. There is no universally accepted definition of what constitutes significant alcohol consumption, but it is generally accepted that more than 21 drinks a week for men and more than 14 drinks a week for women constitutes significant alcohol consumption.2
PREVALENCE
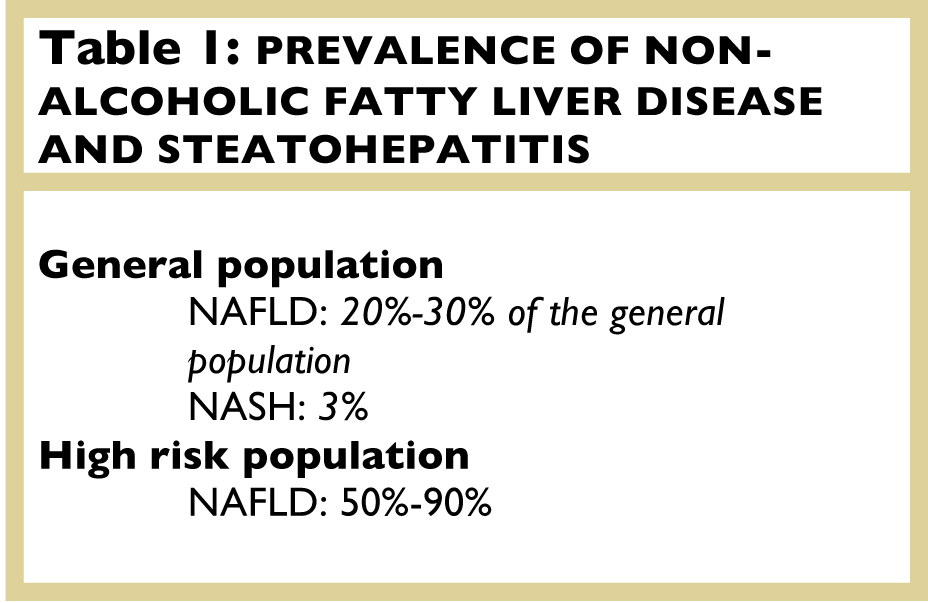
There are only a few large studies that looked at the prevalence of NAFLD but since most patients are asymptomatic until late in the course of the disease, it is widely accepted that the prevalence is underestimated in the general population.3,4,5 Data obtained from two studies that looked at potential living donors found that the histologically proven prevalence of NAFLD in this population was 20%-50%. Studies that used liver ultrasound to define the prevalence of NAFLD found that it ranges between 17%-46%. Published data obtained from autopsy studies show that between 2% and 3% have histologic evidence of non-alcoholic steatohepatitis (NASH) (Table 1). In patients with severe obesity undergoing bariatric surgery the prevalence of NAFLD can exceed 90% and up to 5% of these patients may have unsuspected cirrhosis. In the United States alone it is estimated that 100 million individuals suffer from NAFLD.6,7,8,9,10
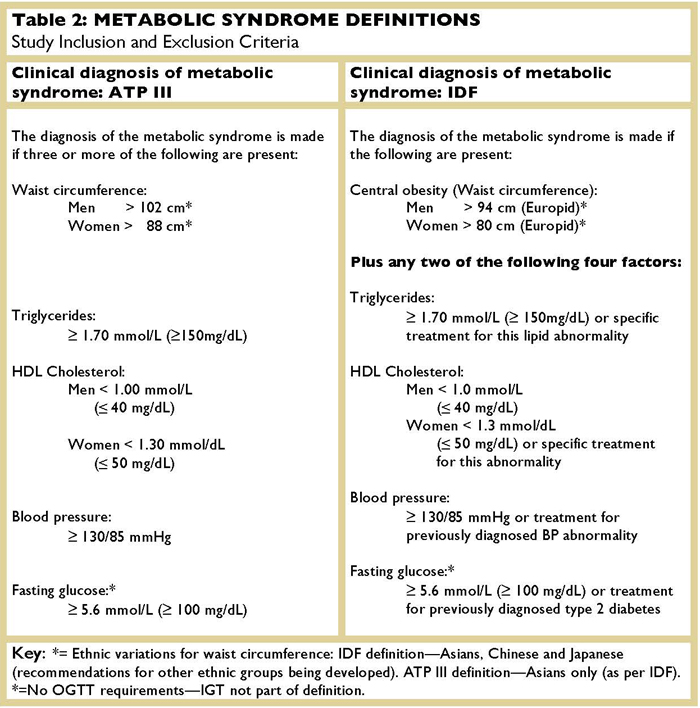
The current concept is that NAFLD is strongly linked to the metabolic syndrome which is defined by having at least three out five of the following conditions: abdominal obesity, high triglycerides, Low HDL, hypertension, low fasting glucose (Table 2).
The exact cause of NAFLD remains unknown but it is evident that it is not the same in all patients. Even though there is a strong association with the metabolic syndrome, not all patients with metabolic syndrome will develop NAFLD and not all patients with NAFLD have the metabolic syndrome. It is currently believed that several “hits” are involved in the development of NAFLD, initially resulting in macrovesicular steatosis. Insulin resistance seems to play a key role in the cascade of events that lead to the accumulation of lipids within the hepatocytes.
NATURAL HISTORY
It is generally agreed that patients with simple steatosis (NAFL) will have a very slow progression to cirrhosis (approximately 4%) while patients with steatohepatitis (NASH) have an estimated risk of progression to cirrhosis of approximately 20%. Between 30%-40% of patients with NAFLD will show a significant degree of fibrosis at the time of diagnosis and between 10%-15% will already have established cirrhosis. The coexistence of other diseases such as HCV in these patients can accelerate the progression of disease.
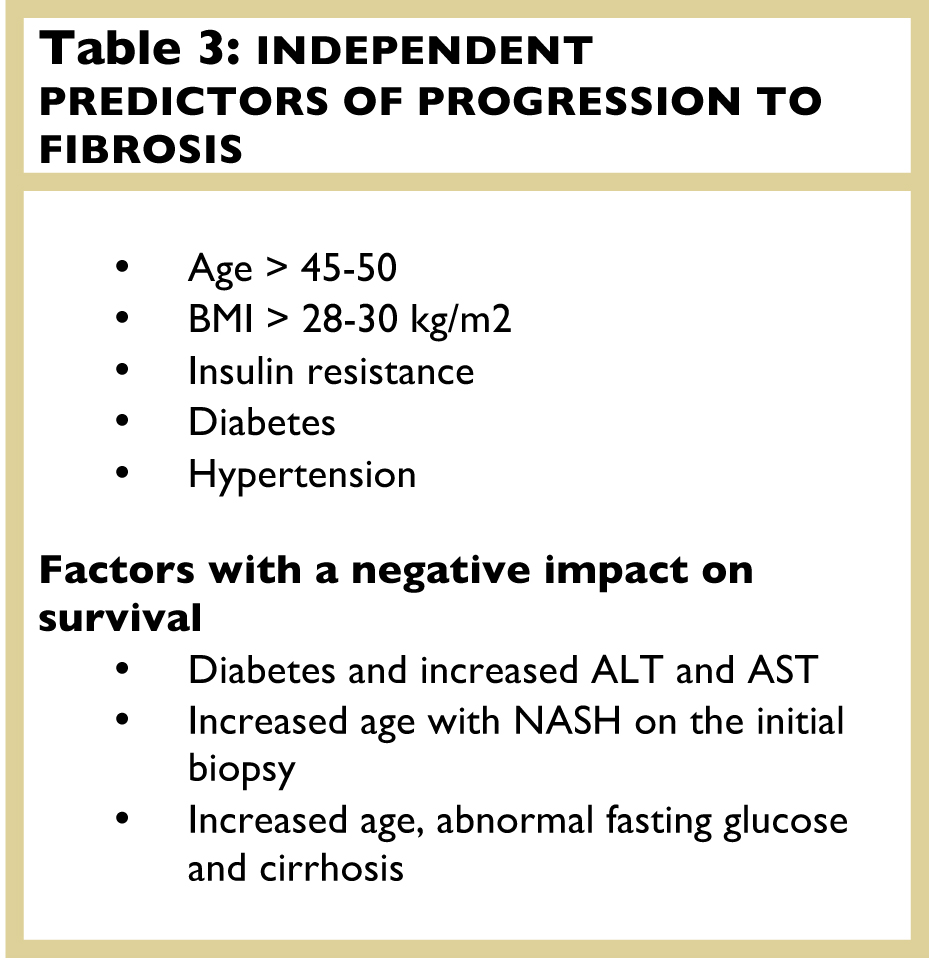
A study that followed 22 NAFLD patients with repeat biopsies for a mean of five years showed that most already had NASH on initial biopsy and that patients had a variable histological course.11 Of the 22 patients, one third had progression of fibrosis and one-third of these had rapid progression to advanced fibrosis, with the only clinical correlate of histologic progression being a higher serum AST. It has also been suggested that NASH is possibly a major cause of “cryptogenic cirrhosis.” Although the natural history of NAFLD is ill-defined, it seems to be determined by the severity of histologic damage. The presence of hepatic fibrosis remains the most important determinant of the patient outcome. Overall, patients with NAFLD have an increased mortality when compared with matched control populations (Table 3).
LABORATORY FINDINGS
Nonalcoholic fatty liver disease is the most common cause of elevated liver chemistry test results. There are currently no specific laboratory tests to diagnose, or for that matter, to monitor NAFLD. The most common findings are mild to moderate elevations of the ALT and AST, but unfortunately there is no correlation between their level of elevation and the severity of inflammation or fibrosis seen on the liver biopsies. Approximately 30% to 60% of patients with biopsy-proven NASH have normal ALT levels.1,12,13 Some studies have shown that patients with a persistently elevated ALT have an increased risk of progression however patients with advanced fibrosis often can have normal liver enzymes.
A new test on the horizon that is showing some promising results as a marker for the presence of steatohepatitis (NASH) is the determination of circulating levels of cytokeratin 18 (CK18), but it seems premature to recommend its use in the absence of supporting published data. In a multi-ethnic cohort, its sensitivity and specificity in the detection of NASH were 58% and 68% respectively.14,15
LIVER BIOPSY
Currently the only accurate way to assess the degree of steatosis, inflammation, and fibrosis in NAFLD patients is a tissue biopsy. Liver biopsy is an invasive procedure that has the potential for severe complications such as bleeding, and it is relatively expensive. It should therefore only be performed when it will benefit patients by guiding therapeutic decisions. A recent article suggests the algorithm below when considering a biopsy in patients with the presumed diagnosis of NAFLD in whom serological evaluation is negative and alcohol has been excluded as a contributing factor.16 (Table 4)
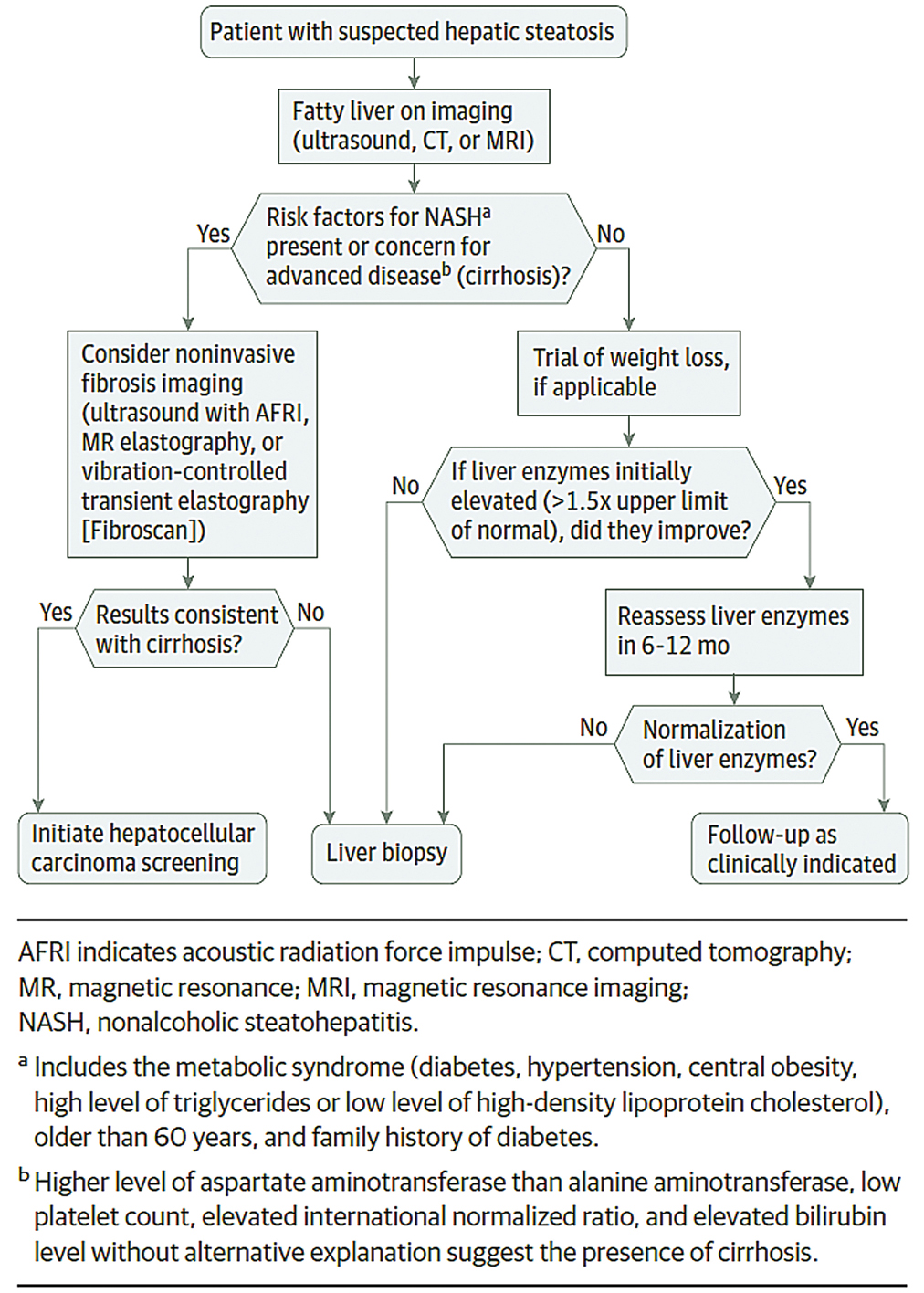
Table 4. Algorithm for determining need for a liver biopsy in patients with presumptive NAFLD (from Rinella ME: Non-alcoholic Fatty Liver Disease: A systematic Review. JAMA. 2015;313(22):2263-2273)
A prerequisite for an accurate diagnosis is an adequate liver biopsy that should be at least 2 cm. in length and contain at least 11 complete portal tracts. It is important to emphasize that liver biopsy is currently the only accurate mean to diagnose NASH, since we know that a) patients whose first biopsy shows evidence of NASH will more likely progress to liver fibrosis; and b) biopsy is required prior to initiating treatment. The pathologist evaluating a liver biopsy must have a detailed clinical history of the patient with special attention to the patient’s serology studies, alcohol intake, and medication history since there are many different etiologies that must be considered in the differential diagnosis of a biopsy that shows steatosis. (Table 5)
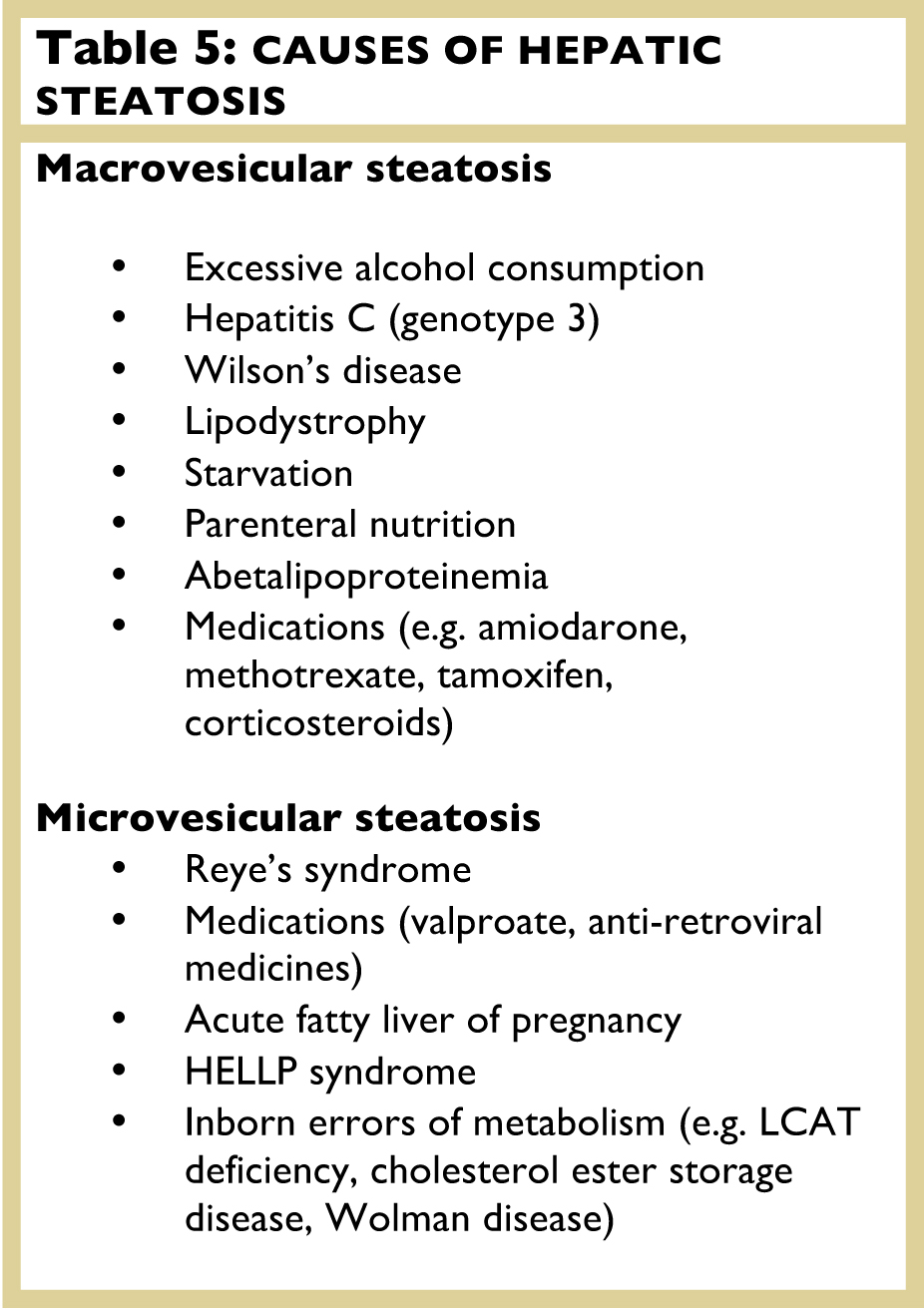
Source: ASSLD Practice Guidelines
HISTOLOGICAL FINDINGS
The histological findings are fairly well defined. In general they are divided into two main subtypes – those that show pure steatosis without inflammation (NAFL), and those that show steatosis with inflammation (NASH). (Figure 2)

Fig. 2: Histological Changes in Hepatic Steatosis With and Without Inflammation (From Rinella ME: Nonalcoholic Fatty Liver Disease: A systematic Review. JAMA. 2015;313(22):2263-2273)16
As stated previously, the presence of hepatic fibrosis is the most important factor that will determine the outcome of patients with NAFLD. Currently the two most commonly use scoring systems are the METAVIR and the Batts-Ludwigs (Bellow). (Figure 3)
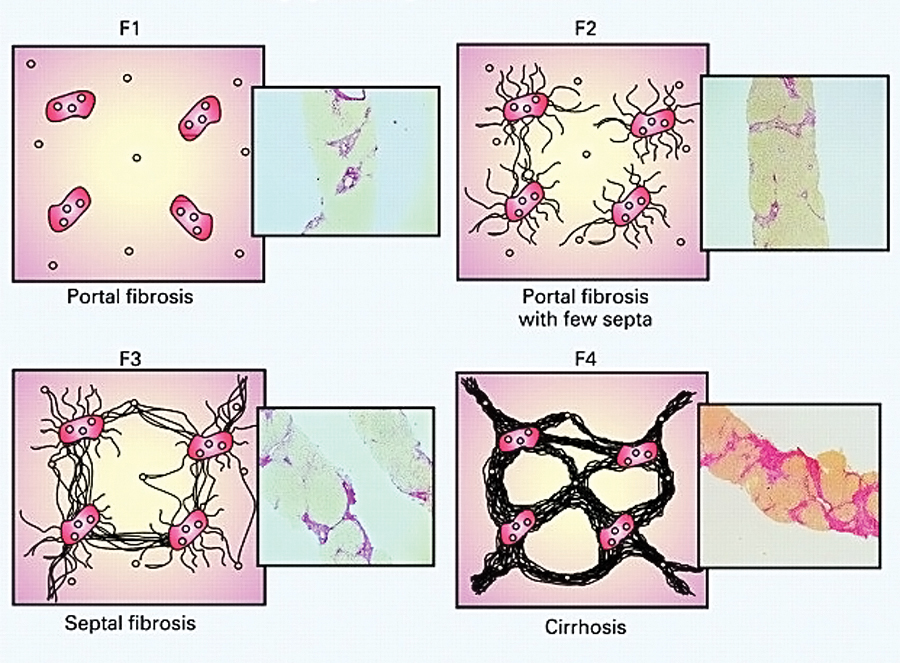
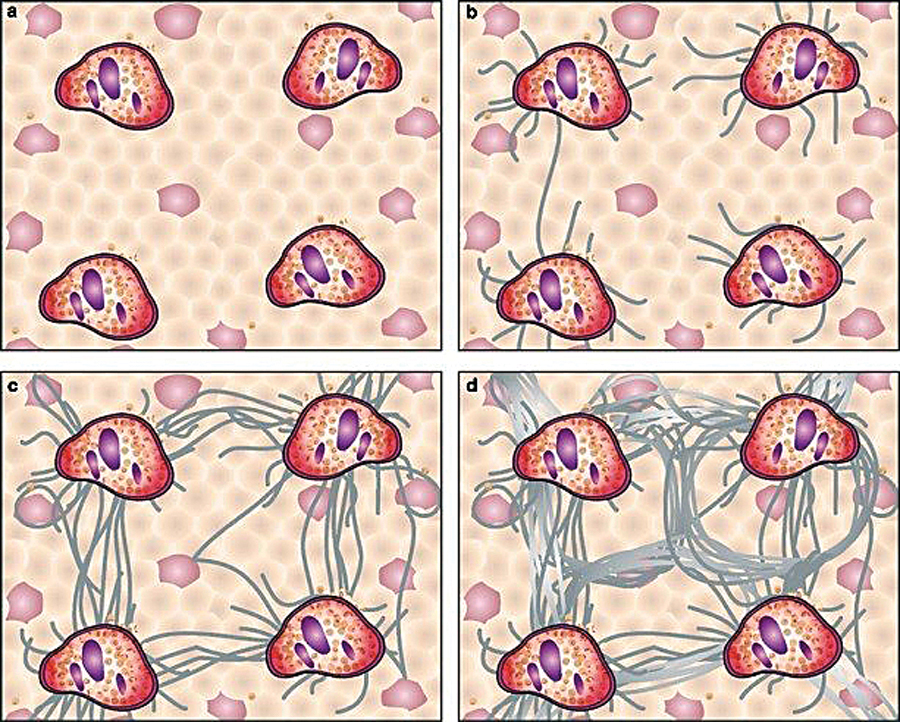
Fig. 3: Scoring Systems for Hepatic Fibrosis. (From Theise MD, Liver Biopsy Assessment in Chronic Viral Hepatitis; A Personal, Practical Approach. Mod. Path. 2007; 20: S3-S14.)
With the aid of special stains such as the trichrome stain the pathologist can identify even early lesions such as pericentral and perisinusoidal fibrosis typically seen in NASH.
SUMMARY
Non-alcoholic fatty liver disease is related predominantly to the metabolic syndrome, and thus is occurring with increasing prevalence. It is quickly becoming the No.1 cause of liver disease in the USA and in the near future will be the most common etiology of cirrhosis and need for liver transplantation. As with other etiologies of cirrhosis, NAFLD cirrhosis incurs not only all the metabolic and hemodynamic dysfunctions of cirrhosis, but also the increased probability of hepatocellular carcinoma. The factors leading to steatosis, and the additional factors needed to develop fibrosis, are largely unknown. Fortunately, the degree of liver steatosis and—in some circumstances—fibrosis, may regress with modification of diet and lowering of BMI. Currently, while imaging and laboratory studies are helpful, the liver biopsy remains a valuable modality to determine the presence and degrees of liver damage and fibrosis.
REFERENCES
1. Ludwig J, Viggiano TR, McGill DB, Oh BJ: Non-alcoholic steatohepatitis: Mayo Clinic experiences with a hitherto unnamed disease. Mayo Clin Proc 55(7):434–438, 1980
2. Naga Chalasani, MD, FACG, Zobair Younossi, MD, FACG, Joel E. Lavine, MD, PhD, et al. The Diagnosis and Management of Non-Alcoholic Fatty Liver Disease: Practice Guideline by the American Association for the Study of Liver Diseases, American College of Gastroenterology, and the American Gastroenterological Association. HEPATOLOGY, Vol. 55, No. 6, 2012.
3. Angulo P, Lindor KD: Non-alcoholic fatty liver disease. J Gastroenterol Hepatol 17 (Suppl):S186–S190, 2002
4. Tominaga K, Kurata JH, Chen YK, et al.: Prevalence of fatty liver in Japanese children and relationship to obesity. An epidemiological ultrasonographic survey. Dig Dis Sci 40(9):2002–2009, 1995
5. Franzese A, Vajro P, Argenziano A, et al.: Liver involvement in obese children. Ultrasonography and liver enzyme levels at diagnosis and during follow-up in an Italian population. Dig Dis Sci 42(7): 1428–1432, 1997
6. Boza C, Riquelme A, Iba~nez L, et al. Predictors of non-alcoholic steatohepatitis (NASH) in obese patients undergoing gastric bypass. Obes Surg. 2005;15:1148-53.
7. Haentjens P, Massaad D, Reynaert H, et al. Identifying non-alcoholic fatty liver disease among asymptomatic overweight and obese individuals by Clinical and biochemical characteristics. Acta Clin Belg. 2009;64:483-93.
8. Machado M, Marques-Vidal P, Cortez-Pinto H. Hepatic histology in obese patients undergoing bariatric surgery. J Hepatol. 2006;45:600-6.
9. Colicchio P, Tarantino G, del Genio F, et al. Non-alcoholic fatty liver disease in young adult severely obese non-diabetic patients in South Italy. Ann Nutr Metab. 2005;49:289-95.
10. Beymer C, Kowdley KV, Larson A, Edmonson P, Dellinger EP, Flum DR. Prevalence and predictors of asymptomatic liver disease in patients undergoing gastric bypass surgery. Arch Surg. 2003;138: 1240-4.
11. Harrison SA, Torgerson S, Hayashi PH: The natural history of nonalcoholic fatty liver disease: a clinical histopathological study. Am J Gastroenterol 98:2042–2047, 2003
12. Powell EE, Cooksley WG, Hanson R, et al. The natural history of nonalcoholic steatohepatitis: a follow-up study of forty-two patients for up to 21 years. Hepatology 11(1):74–80, 1990
13. Diehl AM, Goodman Z, Ishak KG: Alcohol-like liver disease in non-alcoholics. A clinical and histologic comparison with alcohol induced liver injury. Gastroenterology 95(4):1056–1062, 1988
14. Wieckowska A, Zein NN, Yerian LM, et al. In vivo assessment of liver cell apoptosis as a novel biomarker of disease severity in non-alcoholic fatty liver disease. Hepatology. 2006;44(1):27-33.
15. Feldstein AE, Wieckowska A, Lopez AR, et al. Cytokeratin-18 fragment levels as non-invasive biomarkers for non-alcoholic steatohepatitis: a multicenter validation study. Hepatology. 2009;50(4):1072-1078.
16. Rinella ME: Non-alcoholic Fatty Liver Disease: A systematic Review. JAMA. 2015;313(22):2263-2273