Fall 2015 - Vol. 10, No. 3
Click HERE to download the Lipid Guidelines
Lipid Management:
Current Challenges of Reaching Consensus
Tina M. Davis, MSN, CRNP, CLS
Rolf L. Andersen, MD, FACC, BCCL
Eric F. Hussar, MD
Paul N Casale, MD, MPH
Paul M. Conslato, MD, FACP, MBA*



Health care providers who treat dyslipidemias were presented with a dilemma following the recent release of two conflicting lipid guidelines by different nationally recognized organizations. First, the American College of Cardiology and the American Heart Association (ACC/AHA) jointly released the Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults in November 2013.
1 Subsequently, the National Lipid Association (NLA) released the NLA Recommendations for Patient-Centered Management of Dyslipidemia in September of 2014.
2 Differences between these guidelines created confusion and even division among health care providers about the “correct” way to treat dyslipidemias.
In response to the need for clear direction and standardization across our entire organization, in June of 2014 Lancaster General Health assembled a panel of health care providers to develop lipid guidelines. The panel was comprised of seven physicians, a nurse practitioner, a quality assurance clinician, and a clinical pharmacist, who collectively provided expertise in primary care, internal medicine, endocrinology, cardiology, lipidology, quality assurance, pharmacology, and population health.
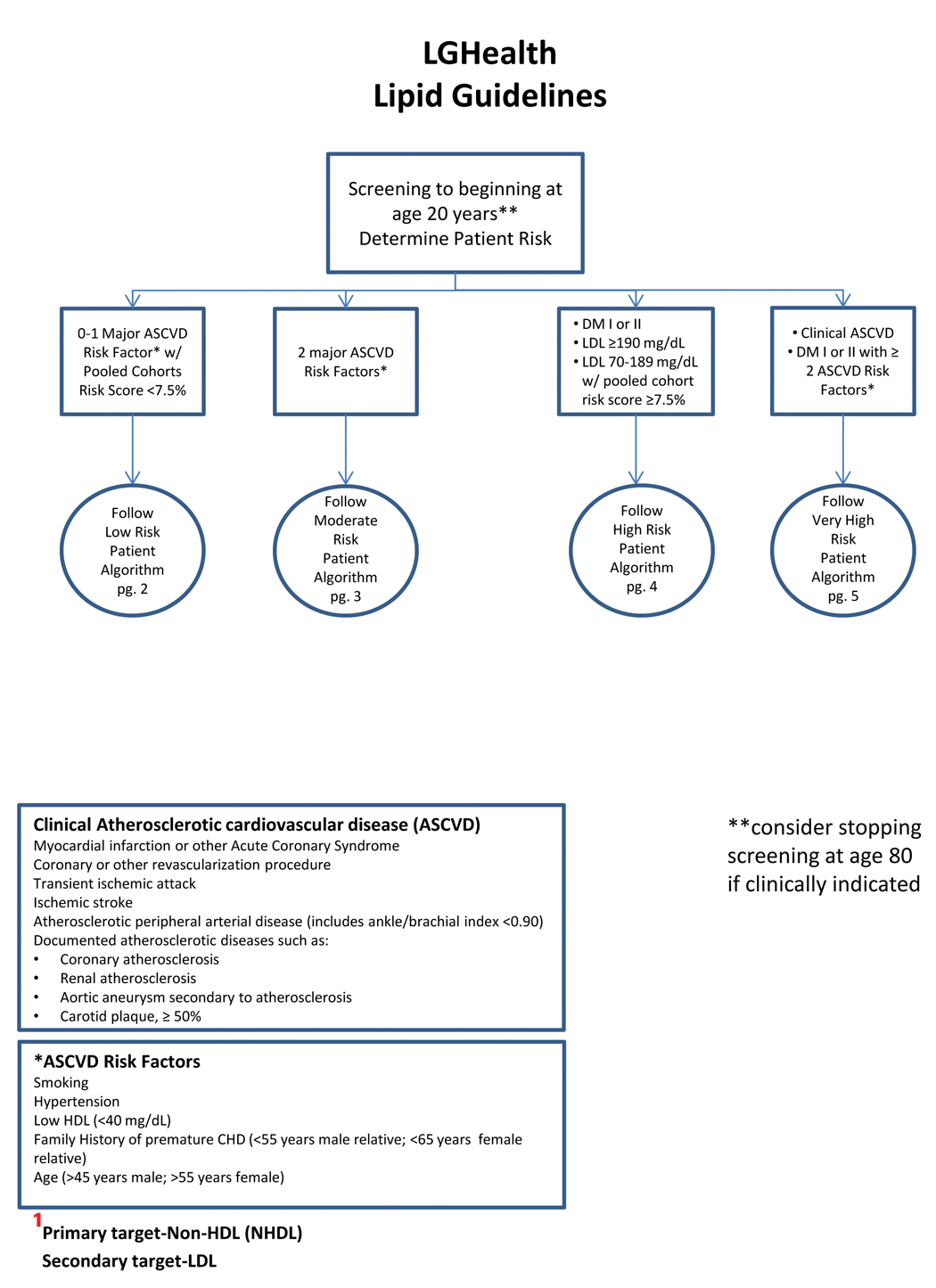
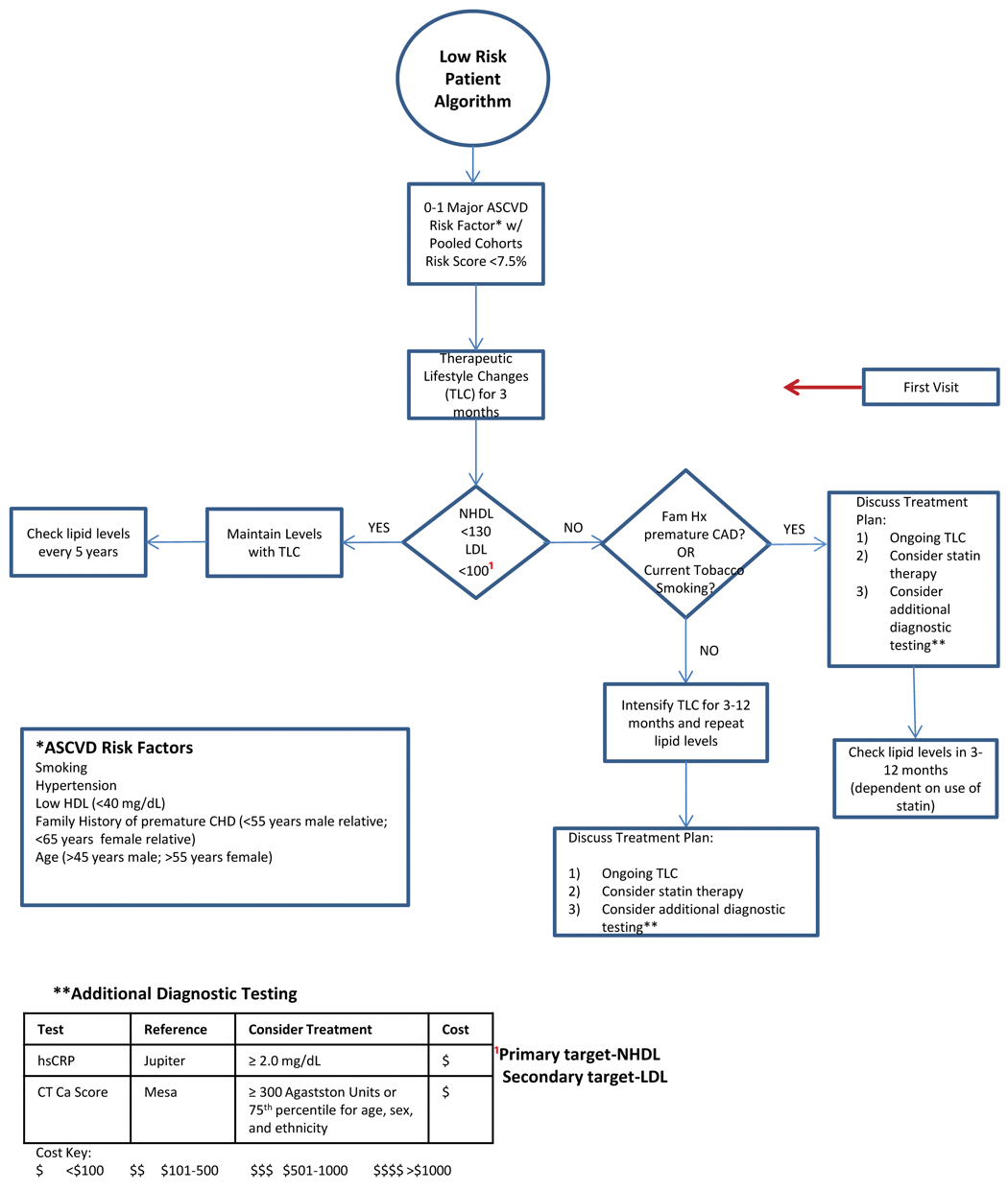
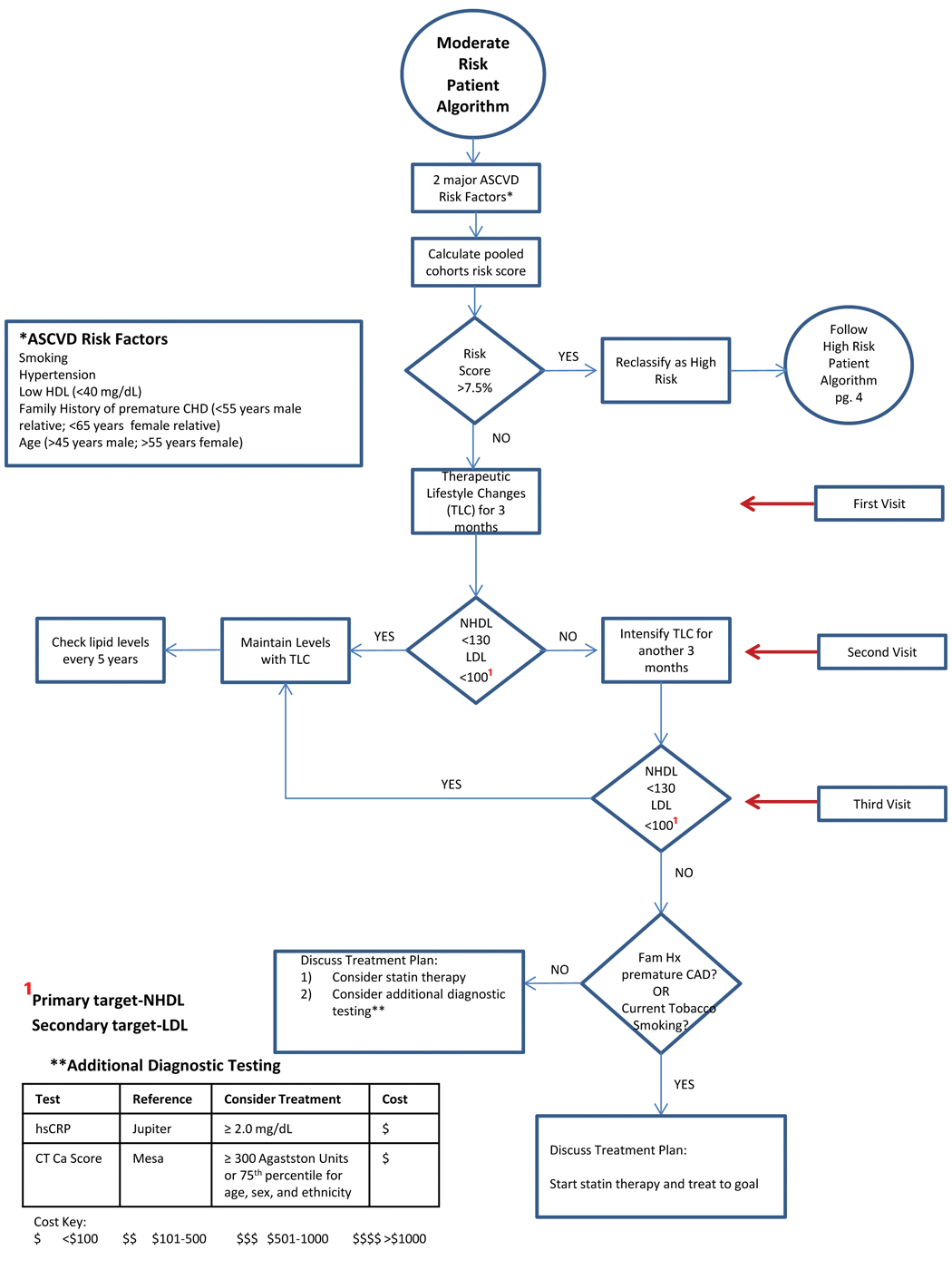
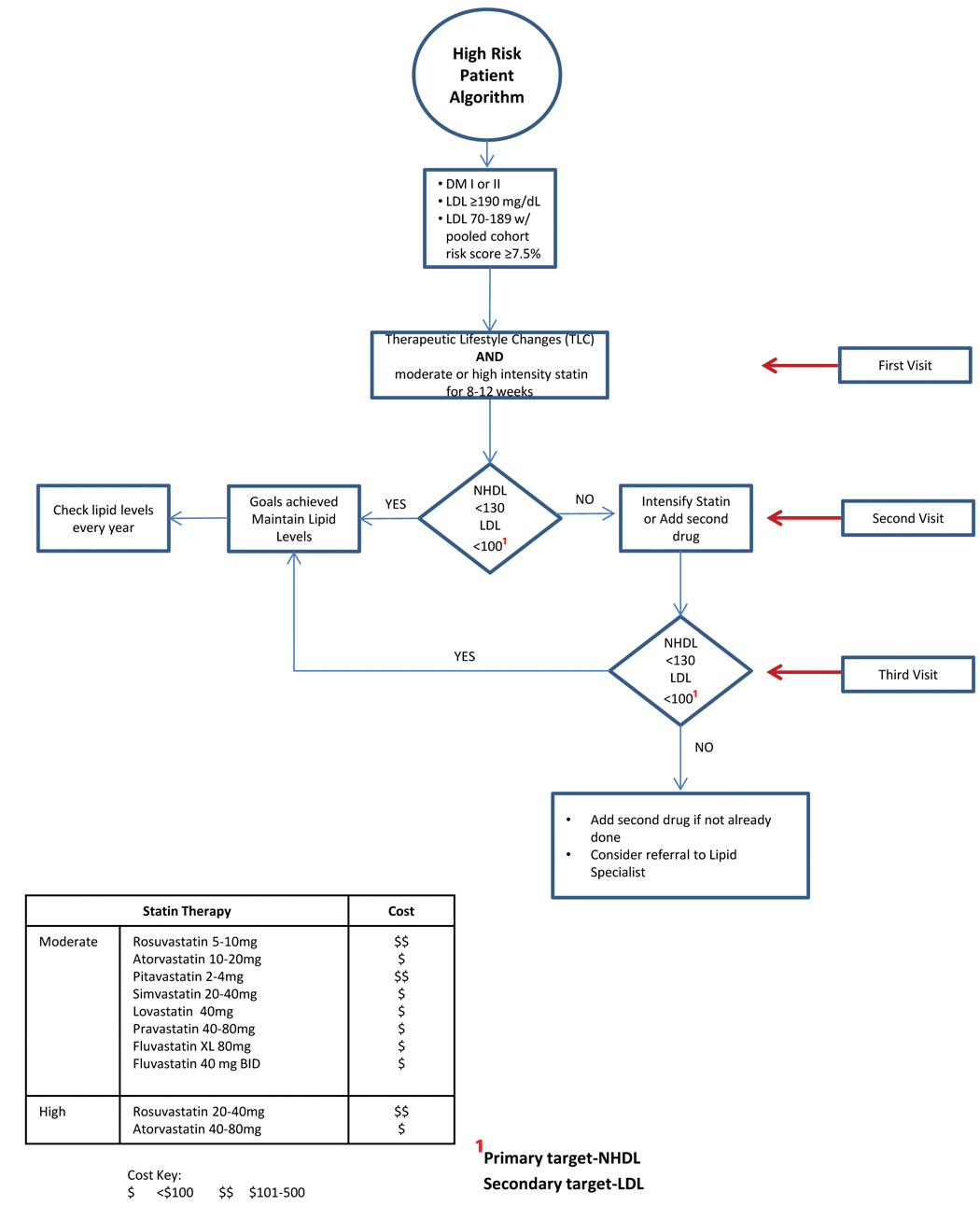
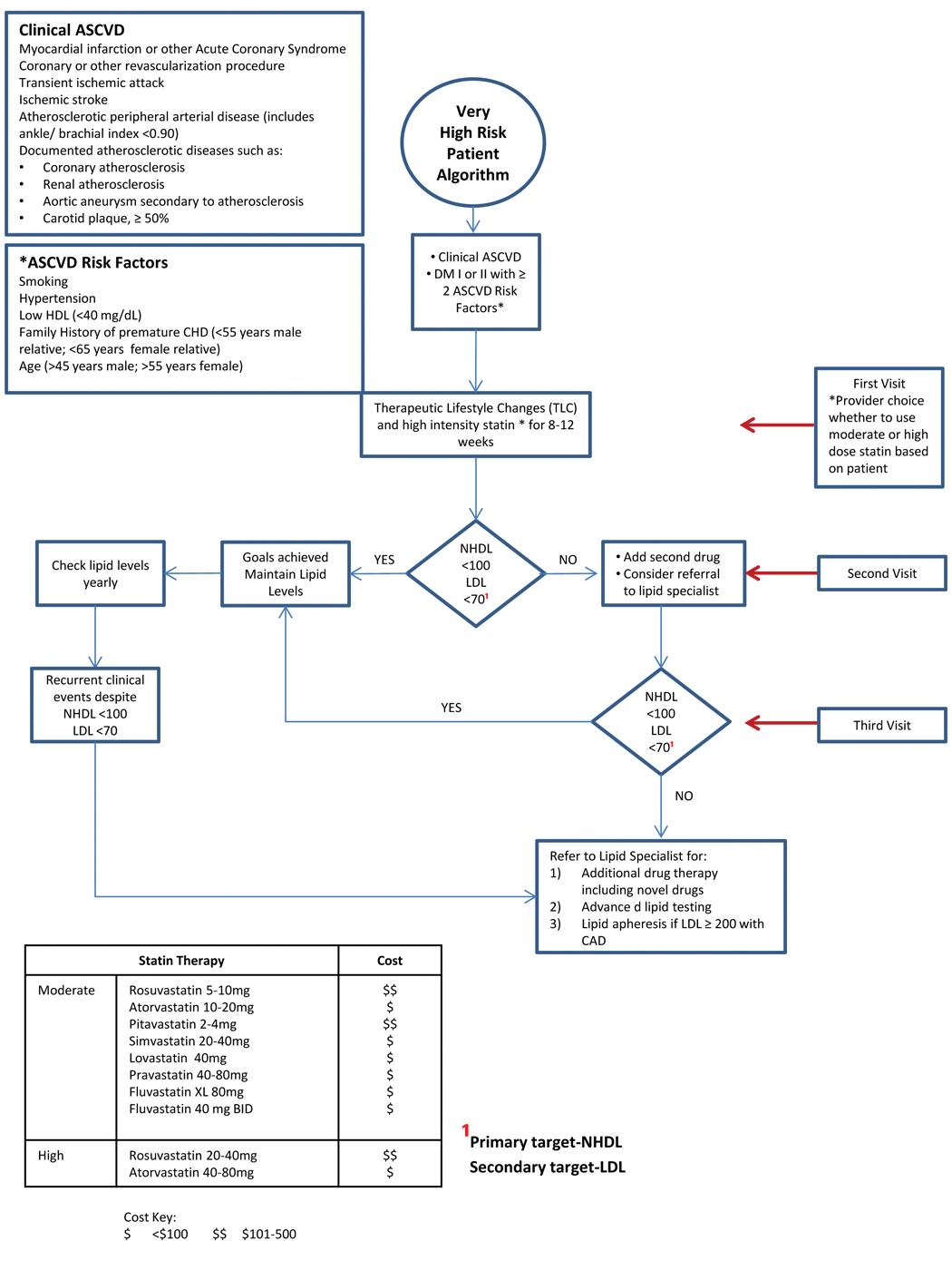
Named the Lipid Task Force (LTF), this team of primary and specialty care providers collaborated to develop guidelines that would provide optimal care for individual patients while improving patient outcomes and retaining cost effectiveness. Over a period of 10 months, the guidelines were analyzed, additional information was reviewed, and a set of algorithms was developed that directed lipid management based on the “best” from both guidelines. The LTF agrees with the ACC/AHA and the NLA that the primary treatment for all risk levels is Therapeutic Lifestyle Changes (TLC). However, when statins are indicated, providers are encouraged to engage their patients in discussions about treatment options to arrive at a unified decision. LGH’s algorithms are meant to guide treatment but not to replace clinical judgment, and they are realistic in recognizing that deviation from their recommendations may sometimes be necessary in individual cases.
The LTF rendered conclusions on lipoprotein treatment targets, defined risk categories, and identified appropriate tests for determining risk.
1. Treatment targets
The first decision to be made was whether to treat by percentile or lipoprotein targets. The National Cholesterol Education Panel (Adult Treatment Panel III) in 2001 (updated in 2004) followed the 13-year tradition of treating to specific lipoprotein targets.3 The ACC/AHA guidelines presented a paradigm shift from treating to lipoprotein targets to prescribing statins based on their intensity to achieve percentile reductions in LDL-C and risk.1 For instance, patients at high risk for Atherosclerotic Cardiovascular Disease (ASCVD) are advised to take a moderate intensity statin to reduce LDL-C by 30-<50%. This alteration in treatment goals is based on the findings of Randomized Controlled Trials (RCTs) performed since 2009, even though those (and prior) studies used fixed doses of lipid medications without titration to specific targets. Although RCTs are generally felt to provide sound scientific evidence, they do not necessarily provide the last word: a) their results in defined populations often cannot be applied to individual patients in clinical settings; and b) investigators who are the beneficiaries of corporate support for the studies may not be fully objective in their interpretations. It is therefore helpful to include other scientific data, such as from epidemiological, genetic, metabolic, and mechanistic trials, to supplement evidence found in RCTs and to make it more generalizable.2
In addition, multiple trials support the concept that when it comes to serum lipid levels, “lower is better,” and the risk of ASCVD is proportional to the degree of lipoprotein reduction that is achieved. The evidence includes trials like the Scandinavian Simvastatin Survival Study, Management of Elevated Cholesterol in the Primary Prevention Group of Adult Japanese trial, the Air Force/Texas Coronary Atherosclerosis Prevention Study, Treating to New Targets trial, and Reversal of Atherosclerosis with Aggressive Lipids Lowering.4,5,6,7,8 More recently, the IMPROVE-IT trial (IMProved Reduction in Outcomes: Vytorin Efficacy International Trial) revealed an additional 10% reduction in ASCVD events when Ezetimib was combined with a statin.9 Post hoc analysis of ODYSSEY trials suggests a 50% additional reduction in LDL-C and further risk reduction in ASCVD when a PSCK9 (Proprotein convertase subtilisin kexin 9) inhibitor was added to a statin.10 Thus, treating to specific lipoprotein targets with medication therapy in addition to lifestyle modification would assure the proper aggressiveness in modifying the patient’s absolute risk. In addition, specific targets would effectively communicate clear goals for the patient and the provider, likely improving long-term adherence to prescribed therapy.
Next, an agreement was reached to use Non HDL cholesterol (NHDL-C) as the primary treatment target, and LDL-C as a secondary target. Elevated levels of apoB- containing lipoproteins have been linked to the formation of atherosclerosis and the occurrence of ASCVD events. NHDL–C is a sum of all apoB-containing lipoproteins, which makes it a more useful indicator of risk. The decision to use NHDL-C as the primary target is supported by a substantial amount of evidence from 2001 forward that NDHL-C is a better predictor than LDL-C alone.11-17
2. Risk Assessment
Risk assessment is an integral part of determining lipid treatment, so the LTF made a specific decision about which risk calculator they would recommend. For years, clinicians used the Framingham Risk Score to estimate a patient’s 10-year CHD risk. In 2013, ACC/AHA recommended switching to The Pooled Cohorts Equation risk calculator because it provided better risk estimation for a more diverse population that includes African Americans and women, it included diabetes in the assessment, and it identified risk for stroke as well as coronary heart disease. This risk calculation was used by the LTF over a period of time and found to be relatively easy to use and valuable in determining treatment. Currently, the Pooled Cohorts Equation is being built into the Electric Medical Records (EMR) system to promote easier use by clinicians. The LTF suggests that providers calculate the risk score with patients, discuss the guidelines for when to start statins, and explain the 20%-38% risk reduction that results from statin use. This may help patients better understand the benefits statins provide.
3. Diagnostic Tests
Additional diagnostic testing to ascertain the level of risk for low and moderate risk patients, and to determine the need for statins, was suggested by both ACC/AHA and NLA. The LTF evaluated the scientific data about the usefulness of available diagnostic tests and their costs in the low and moderate risk category, and determined that a high sensitivity C-Reactive protein determination, and/or CT scan Calcium score, provide the best information to guide the decision about prescribing statin therapy. Both diagnostic tests are financially reasonable in the LGH system, with a cost below $100.
LIPID ALGORITHMS
A proposed set of algorithms was developed and modified over a 9-month period, and was reviewed by experts in the health care system for comments and questions before finalization. The most common question was whether there is any age at which it is no longer necessary to begin a statin or to continue to treat. The LTF reviewed available scientific data though there is little pertaining to statin use above the age of 80. Accordingly, the LTF did not include an age limit in its guidelines, but recommended evaluation of each patient to determine appropriate individual plans.
In March, a continuing medical education (CME) program was presented to educate health care providers about the new lipid algorithms. Forty-eight health care providers attended, representing 20 out of 26 practices in the Lancaster General Health system. An evaluation of the audience response data revealed that there was a need for standardized guidelines. Providers reported differences in treatment targets with many physicians treating to specific lipoprotein levels (72%), a few to a percentage (3%), and a few treating with no specific goal in mind (3%).
Interpreting a patient’s risk was determined by using the Framingham risk score (12% of respondents), Pooled Cohorts score (46%), traditional risk factors (27%), and gut instinct (15%). 56% of respondents felt that the best predictor of ASCVD risk was NHDL, 38% thought it was LDL-C, and 6% preferred ApoB. In addition, knowledge about appropriate LDL and NHDL goals and moderate and high intensity statins was variable. Later feedback obtained through post CME evaluations disclosed that 57% of the participants felt the CME would improve their care, 20% felt it would change care, and 30% felt it confirmed the current care in their practices.
Future endeavors of the LTF include building the algorithms into the EMR system for ease of use in the clinical setting and investigating the guidelines’ impact on cost of care. Expected outcomes include standardizing patient treatment, avoiding unnecessary laboratory and imaging tests in primary prevention, and preventing duplication of services between specialty and primary care. Ongoing educational opportunities will be offered to improve the providers’ knowledge of the algorithms and their ease of use. Patient engagement and activation tools are being developed in print and multimedia to better enable providers to engage their patients in TLC that are desirable and practical. In addition, patient tools assist providers to deliver better healthcare in a more efficient manner, promoting greater provider satisfaction.
The desired outcomes of standardizing the guidelines are to provide clarity for providers concerning appropriate treatment, to ensure optimal health care for patients system-wide, and to provide these services in a cost effective manner.
REFERENCES
1. Stone NJ, et al. 2013. ACC/AHA guideline e on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25Pt B): 2889-2934.
2. Jacobson, TA, et al. National Lipid Association recommendations for patient –centered management of dyslipidemia: part 1-full report. J Clin Lipidol. 2015; (9)2: 129-169.
3. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circ. 2002;106: 3143-3421.
4. Scandinavian Simvastatin Survival Study Group. Randomized trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet. 1994; 344:1383-1389.
5. Nakamura H ,et al. Primary prevention cardiovascular disease with pravastatin in Japan (MEGA Study): a prospective randomized controlled trial. Lancet. 2006;368(9542): 1155-63.
6. AFCAPS/TEXCAPs: Downs, JR et al. Primary prevention of acute coronary events with Lovastatin in men and women with average cholesterol levels. JAMA 1998: 279; 20 1615-1621.
7. LaRosa, JC, et al. Treating to New Targets (TNT) Investigators. Intensive lipid lowering with atorvastatin in patients with stable coronary disease. NEJM. 2005; 352: 1425-1435.
8. Nissen SE, et al. Effect of intensive compared with moderate lipidlowering therapy on progression of coronary atherosclerosis: a randomized controlled trial (REVERSAL). JAMA. 2004; 291(9): 1071-1080.
9. Cannon CP, et al. Ezetimibe added to statin therapy after acute coronary syndromes. NEJM. 2015; 372: 2387-2397.
10. Robinson, JG, et al. Efficacy and Safety of Alirocumab in Reducing Lipids and Cardiovascular Events. NEJM. 2015; 372:1489-1499
11. Cui, Y et al. Non-high density lipoprotein cholesterol level as a predictor of cardiovascular disease mortality. Arch Intern Med. 2001; 1413-1419.
12. Farwell, WR, et al. Non-high-density lipoprotein cholesterol versus low-density lipoprotein cholesterol as a risk factor for a first nonfatal myocardial infarction. AM J Cardiol. 2005; 96: 1129-1134.
13. Ridker, PM et al. Non-HDL cholesterol, apolipoproteins A-1andn B-100, standard lipid measures, lipid ratios, and CRP as risk factors for cardiovascular disease in women. JAMA. 2005; 294:326-333.
14. Liu, J et al. Non-high-density lipoprotein and very-low-density lipoprotein cholesterol and their risk predictive values in coronary heart disease. Am J Cardiol; 2006; 98:1363-1368.
15. Home, I et al. Relationships between lipoprotein components and risk of myocardial infarction: age, gender and short versus longer follow-up periods in the Apolipoprotein MOrtality RISk study (AMORIS). J Intern Med. 2008; 264:30-38.
16. Emerging Risk Factors Collaboration, Di Angelantonio, E et al. Major lipids, apolipoproteins, and risk of vascular disease. JAMA. 2009; 302:1993-20000.
17. Robinson, JG et al. Meta-analysis of the relationship between nonhigh- density lipoprotein cholesterol reduction and coronary heart disease risk. J AM Coll Cardiol. 2009; 53:316-322.
* For The Lipid Task Force of Lancaster General Health, which also includes: Kimberly A Bahata, Douglas C. Gohn, MD, Amber L Jerauld, PharmD, BCACP, Adam C Lake, MD, and Matthew A Sauder, MD
Click HERE to download the Lipid Guidelines