
Fall 2015 - Vol. 10, No. 3
Enhanced Recovery After Surgery:
My Journey from Skeptic to Believer
Walid Hesham, M.D.
General Surgeon, LGHP Surgical Group
I vividly remember sitting next to one of my mentors when I was an impressionable junior resident, and listening to a presentation by Dr. Graham MacKay, a visiting professor who had traveled from Scotland to Boston to speak about a new approach in the care of patients undergoing colorectal surgery. It was called Enhanced Recovery after Surgery or ERAS, and it consisted of a series of new protocols before and after surgery that had a significant impact on the length of stay and complication rates in surgical patients. I, like many others in the audience that day, made light of Dr. Graham’s claims; the changes he described were dramatic and a vast departure from the more traditional methods that had been in use for decades. Yet, as experience has accumulated over the years, many skeptics like me have become advocates for this multimodal, evidence-based approach, because it offers undeniable benefits in the care of surgical patients.
WHAT IS ENHANCED RECOVERY AFTER SURGERY (ERAS)?
ERAS is a set of changes in perioperative care that represents a fundamental shift from the traditional management of the colorectal surgical patient. It uses an evidence-based framework for standardizing care, while simultaneously recognizing the needs of individual patients. The main components of ERAS center on new approaches to preoperative preparation of the patient (i.e. nutrition, hydration, and bowel preparation), and post-surgical pain control, activity, and feeding.1
For instance, prolonged fasting before and after surgery has traditionally been routine for surgical patients. This practice was combined with the administration of excessive fluids intra-operatively, and was originally intended to decrease the likelihood of aspiration, to combat dehydration, and to protect from complications such as renal failure. However, a review of 22 randomized control trials has shown that preoperative fasting after midnight is unnecessary; there is no difference in the reduction of the volume or pH of gastric contents when patients who fast after midnight are compared with those who are allowed to drink clear fluids until two hours before surgery.2 ERAS principles therefore limit fasting and even promote high carbohydrate drinks two to three hours prior to the surgery, thus reducing the need for excessive fluid repletion during the procedure.
Mechanical bowel preparation prior to surgery has similarly been a routine practice in traditional surgical practice, but eliminating stool by means of cathartics has not been shown to change patient outcomes. A 2011 review involving 18 randomized controlled trials of almost 6,000 patients did not find statistically significant differences between patients who had mechanical bowel preparation vs. those who did not, specifically in regard to wound infection, anastomotic dehiscence, reoperation, and mortality.3 In fact, mechanical bowel preparation has adverse effects associated with dehydration and prolonged ileus. ERAS principles discourage bowel preparation prior to surgery thus preventing significant fluid shifts that can lead to dehydration.
Another major change in ERAS involves a reduction in the use of opiate pain medications, as they can significantly delay return of bowel function. The agonistic effects of opioids on mu receptors aid in pain management, but also inhibit peristaltic action of the GI tract. ERAS protocols therefore emphasize non-opioid pain management to decrease opioid-induced inhibition of GI motility and encourage quicker return of bowel function. Other adjuncts to minimize pain and promote speedier return of bowel function include using a minimally invasive approach whenever possible, and ambulating the patients within hours of surgery. Post-operatively, ERAS also encourages nutritional intake prior to return of bowel function, since early enteral feeding is associated with earlier recovery as well as shorter lengths of hospital stay, without increasing the risk of anastomotic dehiscence.4
EVOLUTION OF ERAS
Dr. Henrik Kehlet, Professor of Surgery at Copenhagen University, is credited with initiating the concept of multimodal surgical care during the 1990s. Dr. Kehlet questioned the traditional principles of perioperative care such as prolonged fasting, limitations on mobility, use of mechanical bowel preparations, slow advancement in diet after surgery, and routine use of drains. By avoiding such measures, and subsequently reducing the amount of stress on the body, Dr. Kehlet was able to demonstrate a dramatic decrease in hospital length of stay. Further clinical advances were developed by Dr Kehlet’s colleagues, Professors Ken Fearon and Olle Lungqvist, who assembled the ERAS study group in 2001, and later the ERAS Society in 2010. This milestone coincided with the publication of a meta-analysis by Varadhan et al, which included six randomized trials of more than 450 patients undergoing major elective open colorectal surgery.5 The results indicated a significant reduction in length of stay and complication rates in the enhanced recovery group, with no statistically significant differences in readmission or mortality rates.
Clinicians in the United States followed suit and formed the American Society for Enhanced Recovery (ASER) in 2014 to critically evaluate the role of ERAS within the colorectal patient population. Data from U.S. medical centers included experience at Duke University, where anesthesiologist Dr. Timothy Miller and colorectal surgeon Dr. Julie Thacker showed positive outcomes after implementing an enhanced recovery protocol.6 Their prospective trial showed a decrease of length of stay of two days, as well as a reduction in the number of complications and readmissions.
Earlier this year the University of Virginia (UVA) Health system published outcomes that were similar to those at Duke University when they implemented their own enhanced recovery protocol at UVA. Dr. Thiele and colleagues also implemented a seven-month prospective study to compare outcomes before and after the standardization of care for patients undergoing colorectal surgery. This particular study was unique in that they not only focused on outcomes, but also evaluated direct costs and patient satisfaction using Press Ganey scores. As expected, the enhanced recovery patients showed a substantial reduction in length of stay, faster bowel function recovery, and a reduction in overall complications. In addition, there was a reduction in direct cost per patient of $7,129, resulting in a total savings of $777,061 during the trial. Considerable improvement in patient satisfaction was also seen in the enhanced recovery group as shown by higher Press Ganey scores.7 These findings were so significant that they led to a Wall Street Journal article in May 2015.8 Dr. Traci Hedrick, one of the authors of the UVA study, commented “this will be the standard way that we are managing patients, because the results are so dramatic. It provides higher quality at lower cost, which is the ultimate goal.”9
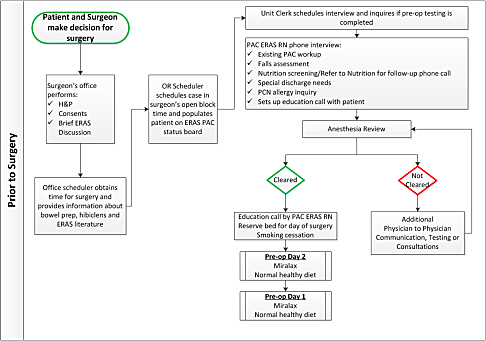
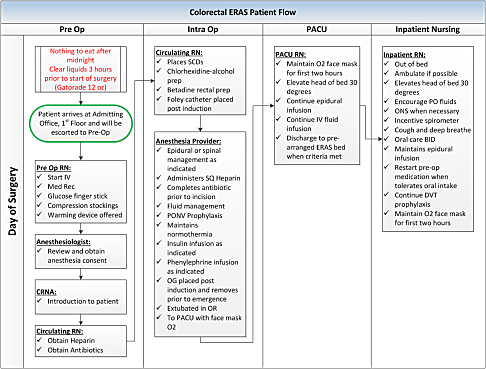
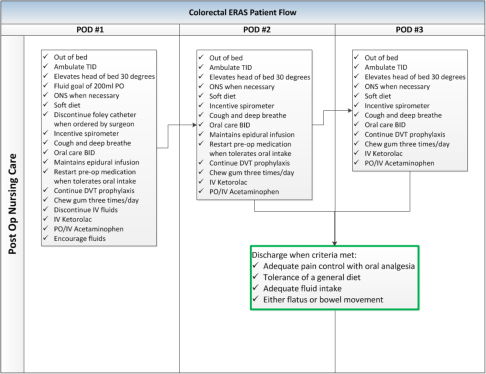
IMPLEMENTATION OF ERAS AT LGH
ERAS is a set of principles that focuses on optimizing nutrition, minimizing electrolyte disturbances and fluid shifts, using non-opioid analgesia, implementing minimally invasive approaches, and promoting early ambulation and feeding. It is changing the landscape of surgical management around the world, with a significant impact on patient care and cost. It has also been evaluated in other surgical disciplines and the results are promising. LGH is on the forefront of these changes; over the past year, a team consisting of anesthesiologists, surgeons, nursing staff, pharmacists, nutritionists, administration, and information technology staff have designed a set of enhanced recovery protocols for LGH patients undergoing elective colorectal procedures. These protocols are now in use (see accompanying graphics). In a few months, we hope to have our own data that show improvements in patient care and satisfaction, while lowering the costs, complications, and hospital stays of our colorectal patients.
REFERENCES
1.Gustafsson UO, Scott MJ, Schwenk W et al. Guidelines for Perioperative Care in Elective Colonic Surgery: Enhanced Recovery After Surgery. World J Surg. 2013 Feb;37(2):259-84. doi: 10.1007/s00268-012-1772-0.
2. Brady M, Kinn S, Stuart P (2003) Preoperative fasting for adults to prevent perioperative complications. Cochrane Database Syst Rev 4:CD004423
3. Guenaga KF, Matos D, Castro AA, Atallah AN, Wille-Jorgen- sen P (2003) Mechanical bowel preparation for elective colo- rectal surgery. Cochrane Database Syst Rev 2:CD001544
4. Han-Geurts IJ, Hop WC, Kok NF, Lim A, Brouwer KJ, Jeekel J (2007) Randomized clinical trial of the impact of early enteral feeding on postoperative ileus and recovery. Br J Surg 94(5):555–561
5. Varandhan KK, Neal KR, Dejong CH et al. The enhanced recovery after surgery (ERAS) pathway for patients undergoing major elective open colorectal surgery: a meta-analysis of randomized trials. Clin Nutr. 2010 Aug;29(4):434-40. doi: 10.1016/j.clnu.2010.01.004. Epub 2010 Jan 29.
6. Miller TE, Thacker JK, White WD et al. Reduced Length of Hospital Stay in Colorectal Surgery after Implementation of an Enhanced Recovery Protocol Anesth Analg. 2014;118(5):1052-61. doi: 10.1213/ANE.0000000000000206
7. Thiele RH, MD, Rea KM, Turrentine FE et al. Standardization of Care: Impact of an Enhanced Recovery Protocol on Length of Stay, Complications, and Direct Costs after Colorectal Surgery. J Am Coll Surg. 2015;220(4):430-43. doi: 10.1016/j.jamcollsurg.2014.12.042.
8. http://www.wsj.com/articles/patients-bounce-back-faster-from-surgery-with-hospitals-new-protocol-1427739292
9. https://www.facs.org/media/press%20releases /jacs/colorectal0205