 Click to Print Adobe PDF
Click to Print Adobe PDF
Fall 2015 - Vol. 10, No. 3
|
Assuring the Blood Supply
at Lancaster General Hospital
Jessica Carlino Yoder, B.S.H.S.
Ulstrasound Technologist, LGHP Surgical Group
Tomomi Horning, M.H.A.
Faculty, Pennsylvania College of Health Sciences
|
  |
“Although an estimated 38% of the U.S. population is eligible to donate, less than 10% actually do each year.”1
ABSTRACT
The Lancaster General Hospital Blood Donor Center has experienced a steady decline in the number of units donated over the last four years. We studied the perspectives of 15 regular donors to uncover their reasons for donating, anticipating that this would assist The Blood Donor Center’s efforts at recruitment and retention.
The three most common motives for initially donating were: a) a desire to help others; b) the influence of role models; and c) incidental factors. The top four reasons for continuing to donate regularly were: a) a desire to help others; b) a smooth donation process; c) an awareness of ongoing need; and d) regular reminders (tied with ongoing need).
We also found that donors appreciate small tangible rewards, and that convenience is critical. These findings suggest several supply-side strategies including: a) pursuing a “captive audience strategy” for institutionally-affiliated non-employees, including medical/dental staff, students, and visitors; b) mobile blood collection at LGH Duke Street; and c) partnering with primary care physicians who would encourage their patients to donate. A review of the academic literature that focused on the demand for blood offered several other considerations including: a) educating physicians; b) assessing physicians’ knowledge of transfusion medicine; c) performing retrospective audits; d) instituting an improved approval processes; and e) implementing PBM (Patient Blood Management) systems.
INTRODUCTION
According to the American Red Cross, roughly 5 million patients in the United States need blood every year. To address those needs, more than 41,000 blood donations are required daily.1 Supply management is complicated by blood’s shelf life of 35-42 days, and the fact that “older” blood can increase morbidity and mortality.
BLOOD DONATION AT LANCASTER GENERAL HOSPITAL
LGH is fortunate in that much of its blood supply is obtained locally from community donors. Nevertheless, as shown in Table 1, the number of donors drawn by the Blood Donor Center (BDC) declined progressively from 2012 to 2015.
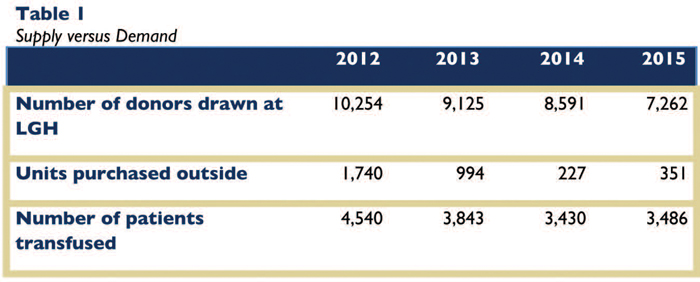
The number of units purchased outside of LGH has changed as the need for blood has fluctuated. Some of the changing requirements may be due to an increased need for platelets in open-heart procedures and at the cancer center. In sum, while there is no crisis, the trends indicate the decline in donors drawn continues to exceed the decline in number of patients transfused.
METHODS
The purpose of this study was to answer the question, “What motivates people to become repeat blood donors?” By exploring the perspectives of regular donors we hoped to uncover information that would improve efforts to recruit and retain more donors. Our hope is that the results of this research will enhance the operations of the LGH BDC and help address the blood needs of the community.
At the request of the LGH BDC supervisor, we sampled 15 participants, all of whom were self-reported members of the LGH BDC Hero Club, who have committed to giving blood at least four times a year. We utilized a convenience sampling technique, developed a semi-structured interview guide based on nine questions, and collected data between January and March 2015. Participants were fully anonymized, and the findings refer to the participants by number, corresponding to the order that the interviews occurred. (Details of the interview protocol are contained in an Appendix that is published on the Journal’s website with the online version of this article.)
RESULTS
Initial motiviation to donate.
Participants attributed their initial decision to donate blood to various underlying influences. As shown in Figure 1, the three most frequently recorded factors were: a) a desire to help others; b) the influence of role models; and c) incidental factors, whereby the participant did not anticipate donating, but responded to opportunities that presented themselves. Other factors included positive peer pressure, employer incentives, and advertisements, which we categorized as other external factors. Two participants cited family needs as their initial motivation.
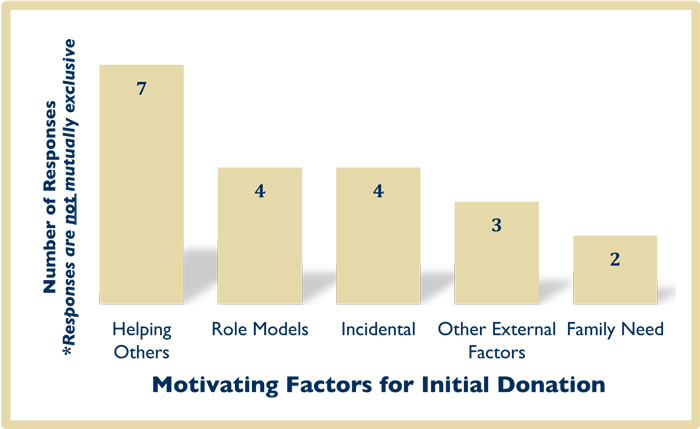
Helping others included descriptive responses that went beyond unembellished statements of that motive. For example, Participant 3 acknowledged that helping others was a learned trait, rooted in childhood. Participant 4 had a similar response, but credited the desire to help others to experiences working in health care. Participant 6 credited their* own good health status as providing sufficient reason to donate, especially when giving blood would help others in the community. Participant 9 incorporated an economic aspect into their response, stating that giving blood to help others did not cost anything.
The second most frequently cited factor was having positive role models, with participants making references to important and influential persons in the their lives. Of the four responses in this category, three participants specifically identified their fathers as an influential role model. Participant 5 identified the Pope as their role model. This participant recalled a time when the Pope held a world blood donor day, published in the Vatican newsletter, which compelled them to donate.
Third, several participants identified that they had no pre-meditation to donate blood, but happened across a blood donor event in which they participated. We categorized these as incidental factors leading to blood donation. All four participants identified the event as having taken place at a college or high school campus.
MOTIVATION FOR ROUTINE DONATION
We also explored why participants donated repeatedly. As shown in Figure 2, the top four factors were: a) a desire to help others, b) a favorable donation process; c) awareness of ongoing need; and d) the receipt of reminders (tied with ongoing need). Other reasons included: a) donors’ personal good health (3 participants), and donors’ current or past work experience (2 participants). One donor stated that they developed donating into a personal habit.
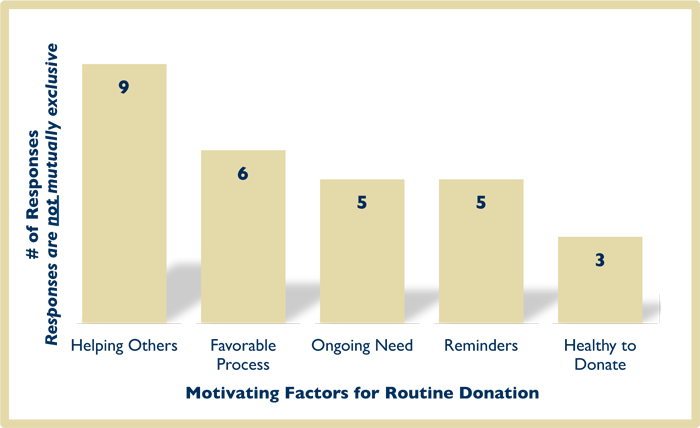
As shown in Figure 2, the most frequently mentioned motive was an unambiguous desire to help others. One participant identified the potential to save a life through their donation efforts. Five participants attributed their regular blood donation to a sense of social justice by helping others (e.g. “important to do,” “right thing to do”), and they expressed a “why not?” perspective. Many participants felt that they were fortunate to be able to give blood, while others could not. They believed they were fulfilling their social responsibility by helping others through blood donation, whereas responses coded to the fifth category, healthy to donate (see Figure 2), did not extend the rationale beyond the participants’ personal health status.
The next two motives were mentioned with equal frequency: a favorable donation process and an ongoing need for blood. Responses coded into favorable donation process included descriptions of the experience as “safe,” “quick,” “easy,” “convenient,” “painless,” “a positive experience,” etc. Donors who cited ongoing need often went beyond this simple statement and mentioned matters such as seeing ill people, and having a frequently needed blood type.
Some participants attributed their routine donations to external factors. Five participants pointed to reminder calls or being prompted by BDC representatives who informed them of their eligibility to donate again. One participant appreciated emails when there was high demand, as well as reminders regarding upcoming blood drives.
INCENTIVES AND CONVENIENCE
We posed two specific questions based on themes that are prevalent in the academic literature: the use of incentives, and the convenience of the blood donor center.
The responses regarding incentives varied. The majority of participants reported that while incentives were not the main reason they donated, they appreciated the gratitude conveyed by incentives. One participant stipulated that incentives should only be used if they do not adversely affect the finances of the BDC. Many participants preferred opportunities to be recognized or personally thanked in lieu of tangible incentives. Participants’ responses varied regarding the desire for recognition to be public or private. One suggested that local public officials could formally recognize routine blood donors, while another preferred a personal thank you.
The participants unanimously affirmed the importance of convenience, which they defined from two perspectives: geographic, and ease of access, which they related principally to operating hours. 46% of participants used emphatic language such as critical and very important when describing convenience. Two participants indicated that they would not donate as frequently if not for convenience of location, or if they had to travel far out of their way to donate.
DISCUSSION
Supply side
Several implications regarding the supply of blood can be drawn from these findings. First, we affirmed the LGH BDC’s current practice of holding multiple mobile blood drives throughout the community in addition to its existing donor center at the Suburban Outpatient Pavilion. Representatives of LGH BDC also communicate frequently with donors. These personal calls are not only functionally effective (e.g. in minimizing missed appointments, optimizing donors’ eight-week rotation, etc.), but they provide opportunities for BDC representatives to thank donors, a recognition that is clearly important to donors. The continued use of small monetary incentives (e.g. gift cards) and non-monetary tangible ones (e.g. movie tickets) is encouraged, but only as a secondary measure of recognition. The findings suggest that donors’ primary motivation stems from their altruistic nature, and therefore any campaigns should affirm donors’ desire to help others. Extensions of current practices include: a) recording video testimonials from blood recipients to use in marketing and/or recruiting; b) recording video testimonials of donors (especially high-school/college-age donors) to use in marketing and/or recruiting their peers; c) inviting blood recipients to speak at donor appreciation events; and d) partnering with public leaders to develop recognition awards for community members who regularly donate.
An analysis of our findings in conjunction with the extant literature also reveals several strategies for LGH BDC to consider. One is a renewed focus on recruiting institutionally affiliated individuals, including non-employees such as medical/dental staff, students, and visitors. This recommendation is based on the criticality of convenience cited by participants as encouraging initial donation as well as making it logistically feasible for them to give routinely, as well as incidental factors, leading to the initial decision to donate. This is seen as a captive audience strategy.1
For example, a study at The University of Virginia Health System highlighted the opportunity for increased blood donation among physicians.2 The researchers found that only 3.1% of donors were physicians, whereas 24.9% were visitors and 23.1% were students. They concluded that physicians are a largely untapped potential donor pool, and hypothesized that convenience may be a constraining factor for physicians. Also, the physician’s role is to help people, which aligns with our finding that helping others was one of the main drivers of routine blood donation.
Given that there is a large captive audience at the LGH Duke Street facility, one suggestion may be to establish a mobile BDC operation there. This expands upon what is already being done, with donation stations being set up by the employee parking garage or in other areas. Another recommendation is to equip a BDC representative to float throughout the building (e.g. family waiting areas, Skylight Café, other public areas, etc.). The focus of this strategy would not necessarily be volume driven, but rather a public relations/marketing effort, providing potential donors incidental opportunities to donate, making the most of the convenience factor, and harnessing donors’ desire to help others-—aligning with the findings from this study. In order to implement such a suggestion and maintain budget neutrality, LGH BDC could determine the times that SOP BDC experiences the lowest volume of donors, and shift those staff hours to Duke Street for mobile blood collection.
While this strategy is perhaps the most easily applied to visitors (who are not constrained by the demands of patient care), inviting medical/dental staff, students, and employees to donate throughout the day may be worth considering. For example, it may be possible to provide donation opportunities during breaks and/or times when a potential donor is performing administrative duties and can sit still for the duration of the blood collection (e.g. staff meetings, making phone calls in the medical staff lounge, etc.).
Finally, physicians in the primary care setting can influence the supply of blood by encouraging their patients to donate. Primary care providers are best positioned to assess their patients’ suitability as donors and to connect information from patients’ medical records (e.g. family, surgical histories, blood type information) with an invitation to donate. This also aligns with our findings that family need drove some participants to initially donate. Additionally, patients generally respect their physicians’ opinions and seek their approval. Patients who are asked by their physicians to donate may be more inclined to do, which may be an application of the positive role model findings from the study.
Demand side
While our study focused on uncovering information that may help improve the blood supply, there is an extensive literature on effective management of blood demand. The literature affirms that consistent and satisfactory application of evidence-based criteria for transfusions is still inadequate, resulting in continued inappropriate use of blood products.3,4,5
At the University of Texas Medical Branch (UTMB), a regional acute care Level 1 trauma center with 699 beds, 70.6% of calls to the blood bank physician were related to requests for blood components that did not meet their previously defined transfusion guidelines, and 14.7% were explicitly attributed to other physician education issues.5 Of the 158 calls related to requests that did not meet transfusion guidelines, only 60% were approved.
The prevalent “physician education issues” reflected poor understanding of: a) the indications for using fresh frozen plasma versus cryoprecipitate; b) calculation of the corrected PLT count increment after a PLT transfusion; c) transfusion reactions; d) transfusion of RBCs to patients with unexpected antibodies, etc.
Marques and co-workers at the University of Alabama/Birmingham Hospital used standardized audits of blood utilization to improve physicians’ knowledge of transfusion medicine.6 Physicians who ordered transfusions without meeting transfusion guidelines received emails asking them to justify their decisions.
Inappropriate transfusions can have serious adverse effects.7 To address quality of care concerns, medical and administrative leaders at New York Methodist Hospital (NYMH), a 612-bed nonprofit, community-based teaching hospital, implemented a two-tier system of assessing the necessity of transfusions.3 The first tier comprised of technologists in the blood bank who evaluated requests against established guidelines. If requests did not meet guidelines, ordering physicians were required to seek approvals from departmental reviewers (Chairs or Division Chiefs in tier two), whose decisions were final. Over the two-year study period, NYMH decreased its blood usage between 24.3% and 56.1%, depending on the blood product, despite a 4.0% increase in hospital admissions. The decreased usage of blood products was accompanied by a 28.6% reduction in complications, and a reduction of more than $2.2 million in total cost of blood products.
A final theme in the literature concerns the efficacy of a comprehensive patient blood management (PBM) system, which has been previously discussed in this Journal.8 In one study, the number of appropriate RBC orders increased, transfusions per patient day decreased by 67%, and blood expenses were reduced by 3%.9 Another institution experienced a decrease in RBC transfusions of 38% despite a 22% increase in admissions.10 Similarly, Stanford Hospital implemented a real-time support system for clinical decisions about blood transfusions that integrated best practice alerts into physician order entry.11 This program resulted in a 24% decrease in RBC transfusions, despite an increase in case mix index from 1.952 to 2.026, with an estimated cost saving of greater than $1.6 million.
In recent years LGH has created a transfusion safety specialist role as well as making continuous improvements in the blood management program which has been reflected in steady improvement in appropriate use of RBC transfusions. In 2012, 70.9% of transfused patients had HGB > 7.0, but that figure has dropped to 29.5%! These results align with the literature, which calls for increased education for physicians to improve knowledge of transfusion medicine. It also highlights the benefits of developing appropriate processes and policies to manage blood demand.
CONCLUSIONS
Our findings affirmed many of the practices of the LGH BDC. Donors are initially and subsequently motivated by a sense of altruism, followed by having positive role models and unplanned opportunities that allowed them to donate immediately. The top four factors which motivated repeated donations included: a) helping others, b) a favorable donation process; c) ongoing need; and d) receiving reminders. The findings also demonstrated that donors appreciate small tangible rewards, and that convenience is critical for effective recruitment and retention.
Several supply-side strategies were also suggested, including: a) pursuing a captive audience strategy for institutionally-affiliated non-employees including medical/dental staff, students, and visitors; b) considering mobile blood collection at LGH Duke Street; and c) partnering with primary care physicians for them to encourage their patients to donate. A review of the academic literature revealed several suggestions including: a) providing physician education; b) specific assessment of physicians’ knowledge of transfusion medicine; c) performing retrospective audits; d) instituting approval processes; and e) implementing PBM systems.
APPENDIX A
One researcher conducted all interviews for consistency. The principal investigator volunteered at the BDC between January and March 2015 and, utilizing a convenience sampling technique, asked donors if they were members of the Hero Club and if so whether they would participate in the study. All participants were self-reported members of the LGH BDC Hero Club, who commit to giving blood at least four times a year. Each participant was given an information sheet that outlined study risks, benefits, and intended uses of the data collected during the study. The acceptance of the invitation to participate served in lieu of an informed consent. At the request of the LGH BDC supervisor the researchers included 15 participants in this study.
As noted in the article, we developed a structured interview protocol comprised of nine questions. Participants were fully anonymized, and the findings refer to the participants by number, corresponding to the order in which the interviews occurred. Most interviews occurred immediately following the donors’ visits to the BDC, though some were conducted via telephone.
Interview Questions
1. What motivated you to initially donate blood?
2. What motivates you to donate blood routinely?
3. What are your attitudes regarding incentives for blood donation?
4. In your opinion, what type of incentive would be the best to receive in exchange for blood donation?
5. How important is convenience of donation center?
6. Have you or a loved one ever received a blood transfusion?
7. Do you feel a sense of social responsibility to continue donating?
8. Do you ever experience fear or anxiety prior to or during donation?
9. Do you feel as though you are aware and educated on the entire blood donation process, such as where your blood goes after it is taken from your body?
REFERENCES
1. Blood Facts and Statistics. American Red Cross, 2015. (Accessed July 13, 2015, from http://www.redcrossblood.org/learn-about-blood/blood-facts-and-statistics)
2. Kanner WA, Jeffus S, & Wehrli, G. An academic-based hospital donor site: Do physicians donate blood? Annals of Clinical & Laboratory Science 2009;39(4): 339-344.
3. Politsmakher A, Doddapaneni V, Seeratan R, & Dosik, H. Effective reduction of blood product use in a community teaching hospital: When less is more. The American Journal of Medicine 2013;126:894-902.
4. Bennett-Guerrero E, Zhao Y, O’Brien SM, et al. Variation in use of blood transfusion in coronary artery bypass graft surgery. JAMA 2010;304(14):1568-75.
5. Bryant BJ, Alperin JB, & Indrikovs AJ. Blood bank on-call physician’s experience at a large university medical center. Transfusion 2005;45:35-40.
6. Marques MB, Polhill SR, Waldrum MR, et al. How we closed the gap between red blood cell utilization and whole blood collections in our institution. Transfusion 2012;52:1857-67.
7. Sharma S, Sharma P, & Tyler LN. Transfusion of blood and blood products: Indications and complications. American Family Physician 2011;83(6):719-24.
8. Bator, S and Bassalin, M. What is a blood management program? J Lanc Gen Hosp. 2013; 8:53-56.
9. Cohn CS, Welbig J, Bowman R, Kammann S, Frey K, & Zantek N. A data-driven-approach to patient blood management. Transfusion 2014;54:316-22.
10. Leahy MF, Roberts H, Mukhtar SA, et al. A pragmatic approach to embedding patient blood management in a tertiary hospital. Transfusion 2014;54:1133-45.
11. Goodnough LT, Shieh L, Hadhazy E, Cheng N, Khari P, Maggio P. Improved blood utilization using real-time clinical decision support. Transfusion 2014;54:1358-65.
* We use gender-neutral pronouns throughout this article, as we did not collect any specific patient identity data, including gender.