
Spring 2015 - Vol. 10, No. 1
Breastfeeding and Maternal Risk of Cardio Metabolic Disease
Gurpinder K. Chatha, M.D.
The Heart Group of Lancaster General Health
Introduction
Cardiovascular disease is the leading cause of death in women1 but awareness levels in US remain low.2 As we transition from individual-level towards population-based care, control of risk factors and prevention of disease become paramount. Among women, adherence to lifestyle guidelines on diet, exercise, and abstinence from smoking is associated with a very low risk of coronary heart disease.3 To further reduce the burden of CV disease in women, it is important to identify and modify additional risk factors and behaviors. While it is acknowledged that breastfeeding benefits infant health, the maternal benefits of lactation appear to be less widely appreciated despite growing evidence that breastfeeding may have lasting effects on the development of cardiovascular disease years later.
Metabolic changes in pregnancy
During pregnancy, dramatic changes occur in a woman’s metabolism to support the developing fetus and prepare for lactation. A mother’s body accumulates fat, especially visceral fat, to meet the feto-placental and maternal demands of gestation and lactation. Visceral (or intra-abdominal) fat is more metabolically active than fat depots in other body areas and is linked to a more adverse cardio-metabolic profile.4 There is increased insulin resistance which is associated with glucose intolerance and a more atherogenic lipid profile.5 Childbearing is also associated with long-term weight gain, obesity, and obesity-related illnesses.6,7 It is hypothesized that lactation plays a central role in “resetting” maternal metabolism, thereby reducing maternal risk for future cardio metabolic disease.5 There is evidence of reduced risk of cardiovascular risk factors including obesity, metabolic syndrome, diabetes, hypertension and hyperlipidemia in women who breastfeed.
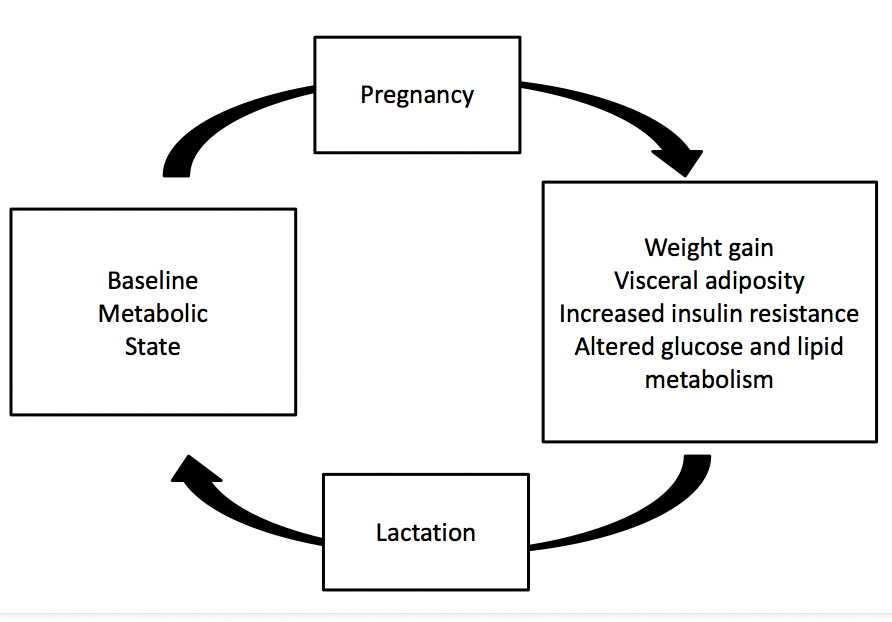
Fig.1. Adapted from Stuebe AM1, Rich-Edwards JW. The reset hypothesis: lactation and maternal metabolism. Am J Perinatol. 2009 Jan;26(1):81-8
Weight changes during breastfeeding
Lactation increases a mother’s metabolic expenditure by an estimated 480 Kcal/day and mothers who breastfeed lose more weight in the postpartum period than mothers who do not.8 In a large prospective study, Baker et al. showed that greater intensity and duration of breastfeeding was associated with greater weight loss at 6 and 18 months postpartum in women of all BMI categories.9 Studies of millions of women reported a relationship between lactation and mother’s obesity in later life, even years afterward. Sixteen to twenty years after their last pregnancy, women who had breastfed for longer than 6 months had significantly lower total body fat mass and fat mass percentage, particularly in the android region, than mothers who had breastfed for less than 6 months. These differences were independent of pre-pregnancy weight and BMI, menopausal status, smoking status, level of education, participation in past and present leisure-time physical activity, and current dietary energy intake.10
Breast-feeding also appears to affect body fat distribution in a positive way. Study of Women’s Health Across the Nation (SWAN)-Heart Study used computed tomography to assess abdominal adiposity. Among premenopausal/early-peri-menopausal mothers, those who never breastfed had 28% greater visceral adiposity, a 4.7% greater waist-hip ratio, and a 6.49 cm greater waist circumference than mothers who breastfed all of their children for ≥3 months.11 Similar findings were seen in the Women and Infant Study of Healthy Hearts (WISH). Visceral adiposity was greater among mothers who never breastfed than among mothers who breastfed for ≥3 months after every birth, even after adjustment for various confounding factors.12
Breastfeeding and risk of Metabolic syndrome
Metabolic syndrome has been defined as the concomitant clustering of central obesity, dysglycemia, hypertension, hypertriglyceridemia, and low high-density lipoprotein (HDL) cholesterol. Several studies have confirmed the increased risk of CVD in individuals with Metabolic syndrome.13
By reducing fat, especially visceral fat, and improving insulin resistance, breastfeeding may reduce the risk of Metabolic syndrome. In the SWAN study, duration of lactation was associated with lower prevalence of Metabolic syndrome in a dose-response manner in midlife, parous women. This was seen after adjusting for age, smoking history, parity, ethnicity, socioeconomic status, study site, physical activity, caloric intake, and high school body mass index.14
Breastfeeding and risk of Diabetes
Several authors have found a higher risk of diabetes in women who have never breastfed compared with those who breastfed for a prolonged period.
In the Nurses Health Study, among parous women, increasing duration of lactation was associated with a reduced risk of type 2 diabetes.For each additional year of lactation, women had a decrease in the risk of diabetes of 15%, controlling for current body mass index and other relevant risk factors for type 2 diabetes.15 Schwarz et al examined data from 139,681 postmenopausal women enrolled in the Women’s Health Initiative observational study or controlled trials. Women who reported a lifetime history of more than 12 months of lactation were less likely to have diabetes than women who never breastfed.16
Similar trends were seen in studies from other countries. The Shanghai Women’s Health Study was a prospective study of 62,095 middle-aged parous women in Shanghai, China, who had no prior history of type 2 diabetes mellitus, cancer or cardiovascular disease at study recruitment. After 4.6 years of follow-up, women who had breastfed their children tended to have a lower risk of diabetes mellitus than those who had never breastfed. Increasing duration of breastfeeding was associated with a reduced risk of type 2 diabetes mellitus.17 Odds ratio for developing obesity and diabetes appears to be especially high in younger (<50 years old) parous women who have never lactated.18
Gestational diabetes mellitus (GDM) during pregnancy puts a mother at high risk not only for developing diabetes but also cardiovascular disease years later. Women with gestational diabetes who breastfeed have a significantly reduced risk of developing diabetes. Women with GDM participating in the prospective German GDM study were followed from delivery for up to 19 years postpartum for diabetes development. Among islet autoantibody-negative women, breastfeeding was associated with a median time to diabetes of 12.3 years compared with 2.3 years in women who did not breastfeed.19
Breastfeeding and risk of Hypertension
There is growing evidence that mothers who do not breastfeed are more likely in later life to develop hypertension, a major cardiovascular risk factor.
In the SWAN study, duration of lactation inversely correlated with both systolic blood pressure and diastolic blood pressure.20 Schwarz et al examined data from 139,681 postmenopausal women in the Women’s Health Initiative observational study or controlled trials. Women who reported a lifetime history of more than 12 months of lactation were less likely to have hypertension (odds ratio [OR] 0.88, P<.001 than women who never breast-fed.21 Similarly, in the US Nurses’ Health Study II, there was an increased risk of maternal hypertension associated with absent or curtailed lactation compared with the recommended ≥6 months of exclusive or ≥12 months of total lactation per child.22
The reduced risk of hypertension has been observed in mothers that breastfed for as little as one to 3 months although longer duration appears to be more beneficial. The beneficial effect of breastfeeding on the risk of Hypertension appears to last long after weaning as seen in the million hearts study.23
Breastfeeding and Risk of Hyperlipidemia
Lipid levels can change dramatically during pregnancy, and serum cholesterol and triglyceride concentrations increase to maximum values during the third trimester. Lactation is associated with a less atherogenic lipid profile both in the short and long term; women who bottle-feed their infants show elevated serum triglyceride level for up to three times longer than those who breastfeed their infants.24 Lactation for at least 3 months is associated with a much smaller reduction in HDL-C levels. In the SWAN study, duration of lactation inversely correlated with triglycerides, total cholesterol, and low-density lipoprotein (LDL) cholesterol, and there was a positive correlation with fasting HDL levels.25 In the Women’s Health Initiative observational study or controlled trials, women who reported a lifetime history of more than 12 months of lactation were less likely to have hyperlipidemia than women who never breastfed.26
As for Hypertension, changes in lipid profile may also persist for years after weaning. At 16-20 years after their last pregnancy, women in the million hearts study who had breastfed for less than 6 months had higher total body fat mass and fat mass percentage which was associated with higher LDL cholesterol and total cholesterol concentrations.27
Effect of lactation on subclinical and clinical CV disease
Mothers who do not breastfeed their infants appear to be at higher risk of vascular characteristics associated with increased risk. Schwarz et al conducted a cross-sectional analysis of women enrolled in the Study of Women Across the Nation-SWAN Heart Study. After adjustment for socioeconomic status, lifestyle, family history variables, body mass index and traditional risk factors for cardiovascular disease, mothers who had not breastfed were more likely to have aortic calcification than mothers who had consistently breastfed. Similarly, the Women and Infants Study of Healthy Hearts showed that compared with mothers who breastfed for 3 or more months after every birth, mothers who never breastfed exhibited unfavorable vascular characteristics like larger lumen diameter and larger adventitial diameter in models adjusting for multiple variables.
Several large prospective cohort studies have found reduced risk of coronary artery disease in women who breastfeed. In the Nurses’ Health Study, Stuebe et al found an inverse association between long duration of lactation and myocardial infarction independent of known risk factors for cardiovascular disease.28 Compared to women who had never breastfed, women who had lactated for 2 or more years had a 23% lower risk of coronary heart disease after adjusting for age, parity , lifestyle factors, family history, early adult adiposity and history of stillbirth. Over an average of 7.9 years of postmenopausal participation in the Women’s Health Initiative, women with a single live birth who breastfed for 7-12 months were significantly less likely to develop cardiovascular disease (hazard ratio 0.72) than women who never breastfed.29 In the Nord-Trøndelag Health Survey (HUNT2), parous women younger than 65 years who had never lactated had a higher cardiovascular mortality than the reference group of women who had lactated 24 months or more (HR 2.77).30
Conclusion
There is growing evidence that breastfeeding reduces the risk of multiple cardiovascular risk factors including metabolic syndrome, visceral adiposity, hypertension, hyperlipidemia and diabetes. There is also emerging evidence that it reduces subclinical as well as clinical cardiovascular disease including cardiovascular mortality.
Despite improvements, breastfeeding rates in the US remain lower than recommended. Of infants born in 2011, 49% were breastfeeding at 6 months and 27% at 12 months but rates for exclusive breastfeeding were much lower.31 In addition to increased maternal and infant morbidity and mortality, suboptimal breastfeeding is also associated with billions of dollars in health care costs.32 The Baby-friendly Hospital Initiative (BFHI) was launched by WHO and UNICEF in 1991 to implement practices that protect, promote and support breastfeeding. In 2012 less than 7% of the US births occurred in baby friendly facilities. In Pennsylvania this number was even lower at 0.08%.33 As previously discussed in a detailed article in this Journal that provided an in-depth review of breast feeding practices at LGH and the measures taken to maximize its use, LGH’s Women and Babies Hospital is one of the only three facilities in Pennsylvania that are designated Baby-friendly.34
A vast majority of the mothers in the Unites States are not receiving the quality of care that will give them the best possible start by providing information, confidence, and skills to successfully initiate and continue breastfeeding their babies. As we move toward value based care and population health, breast-feeding should be considered a key modifiable risk factor for cardiovascular disease and promoted as a part of a healthy lifestyle.
REFERENCES
1. www.cdc.gov/nchs/data_access/Vitalstatsonline.htm
2. Mosca L et al. Fifteen-year trends in awareness of heart disease in women: results of a 2012 American Heart Association national survey. Circulation. 2013 Mar 19;127(11):1254-63, e1-29.
3. Stampfer MJ, Hu FB, Manson JE, Rimm EB, Willett WC. Primary prevention of coronary heart disease in women through diet and lifestyle. N Engl J Med. 2000 Jul 6;343(1):16-22.
4. Pascot A, Lemieux S, Lemieux I, et al. Age-related increase in visceral adipose tissue and body fat and the metabolic risk profile of premenopausal women. Diabetes Care. 1999 Sep; 22(9):1471-8.
5. Stuebe AM , Rich-Edwards JW. The reset hypothesis: lactation and maternal metabolism. Am J Perinatol. 2009 Jan;26(1):81-8.
6. Wolfe WS1, Sobal J, Olson CM, et al. Parity-associated weight gain and its modification by sociodemographic and behavioral factors: a prospective analysis in US women. J Nutr. 2001 Jan;131(1):53-8.
7. Rooney BL, Schauberger CW, Mathiason MA. Impact of perinatal weight change on long-term obesity and obesity-related illnesses. Obstet Gynecol. 2005 Dec; 106(6):1349-56.
8. Butte NF1, Wong WW, Hopkinson JM. Energy requirements of lactating women derived from doubly labeled water and milk energy output. J Nutr. 2001 Jan; 131(1):53-8.
9. Baker JL, Gamborg M, Heitmann BL, Lissner L, Sørensen TI, Rasmussen KM. Breastfeeding reduces postpartum weight retention. Am J Clin Nutr. 2008 Dec; 88(6):1543-51.
10. Wiklund P, Xu L, Lyytikäinen A, Saltevo J, et al. Prolonged breast-feeedng protects mothers from later-life obesity and related cardio-metabolic disorders. Public Health Nutr. 2012 Jan;15(1):67-74.
11. McClure CK1, Schwarz EB, Conroy MB, et al. Breastfeeding and subsequent maternal visceral adiposity. Matern Child Health J. 2012 Feb;16(2):316-21.
12. McClure CK1, Catov J, Ness R, Schwarz EB. Maternal visceral adiposity by consistency of lactation. Matern Child Health J. 2012 Feb;16(2):316-21.
13. Mottillo S, Filion KB, Genest J, et al. The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J Am Coll Cardiol. 2010 Sep 28; 56(14):1113-32.
14. Ram KT1, Bobby P, Hailpern SM, et al. Duration of lactation is associated with lower prevalence of the metabolic syndrome in midlife--SWAN, the study of women’s health across the nation. Am J Obstet Gynecol. 2008 Mar;198(3):268.e1-6.
15. Stuebe AM1, Rich-Edwards JW, Willett WC, et al. Duration of lactation and incidence of type 2 diabetes. JAMA. 2005 Nov 23;294(20):2601-10.
16. Schwarz EB1, Ray RM, Stuebe AM, et al. Duration of lactation and risk factors for maternal cardiovascular disease. Am J Obstet Gynecol. 2008 Mar;198(3):268.e1-6.
17. Villegas R1, Gao YT, Yang G, et al. Duration of breast-feeding and the incidence of type 2 diabetes mellitus in the Shanghai Women’s Health Study. Diabetologia. 2008 Feb;51(2):258-66.
18. Natland ST1, Nilsen TI, Midthjell K, et al. Lactation and cardiovascular risk factors in mothers in a population-based study: the HUNT-study. Int Breastfeed J. 2012 Jun 19;7(1):8.
19. Ziegler AG, Wallner M, Kaiser I, et al. Long-Term Protective Effect of Lactation on the Development of Type 2 Diabetes in Women With Recent Gestational Diabetes Mellitus. Diabetes. 2012 Dec;61(12):3167-71.
20. Ram KT1, Bobby P, Hailpern SM, et al. Duration of lactation is associated with lower prevalence of the metabolic syndrome in midlife--SWAN, the study of women’s health across the nation.
21. Schwarz EB1, Ray RM, Stuebe AM, et al. Duration of lactation and risk factors for maternal cardiovascular disease. Am J Obstet Gynecol. 2008 Mar;198(3):268.e1-6.
2. Stuebe AM1, Schwarz EB, Grewen K, et al. Duration of lactation and incidence of maternal hypertension: a longitudinal cohort study. Am J Epidemiol. 2011 Nov 15;174(10):1147-58.
23. Wiklund P, Xu L, Lyytikäinen A, Saltevo J, et al. Prolonged breast-feeding protects mothers from later-life obesity and related cardio-metabolic disorders.Public Health Nutr. 2012 Jan;15(1):67-74.
24. Darmady JM, Postle AD. Lipid metabolism in pregnancy. Br J Obstet Gynaecol. 1982 Mar;89(3):211-5.
25. Ram KT1, Bobby P, Hailpern SM, et al. Duration of lactation is associated with lower prevalence of the metabolic syndrome in midlife--SWAN, the study of women’s health across the nation. Am J Obstet Gynecol. 2008 Mar;198(3):268.e1-6.
26. Schwarz EB1, Ray RM, Stuebe AM, et al. Duration of lactation and risk factors for maternal cardiovascular disease. Obstet Gynecol. 2009 May;113(5):974-82.
27. Wiklund P1, Xu L, Lyytikäinen A, Saltevo J, et al. Prolonged breast-feeding protects mothers from later-life obesity and related cardio-metabolic disorders. Public Health Nutr. 2012 Jan;15(1):67-74.
28. Stuebe AM1, Michels KB, Willett WC, et al. Duration of lactation and incidence of myocardial infarction in middle to late adulthood. Am J Obstet Gynecol. 2009 Feb;200(2):138.e1-8.
29. Schwarz EB1, Ray RM, Stuebe AM, Allison MA, Ness RB, Freiberg MS, Cauley JA. Duration of lactation and risk factors for maternal cardiovascular disease. Obstet Gynecol. 2009 May;113(5):974-82.
30. Natland Fagerhaug T, Forsmo S, Jacobsen GW, et al. A prospective population-based cohort study of lactation and cardiovascular disease mortality: the HUNT study. BMC Public Health. 2013 Nov 13;13:1070.
31. www.cdc.gov/breastfeeding/data/nis_data/index.htm
32. Bartick MC1, Stuebe AM, Schwarz EB, Luongo C, Reinhold AG, Foster EM. Cost analysis of maternal disease associated with suboptimal breastfeeding. Obstet Gynecol. 2013 Jul;122(1):111-9.
33. www.cdc.gov/breastfeeding/pdf/2012breastfeedingreportcard.pdf
34. Frye, GM. Breast Feeding Initiatives At Women And Babies Hospital. J Lanc Gen Hosp. 2013; 8: 21-27