

Fall 2006 - Vol.1, No.2
“Breast Cancer: An Illustrated Case Study”
Daleela G. Dodge, M.D.
Chief of General Surgery, Lancaster General Hospital,
Lancaster Surgical Group
and
Jennifer L. Kegel, M.D.
Section Chief, Mammography,
Lancaster General Hospital, Lancaster Radiology Associates.
Judy Connolly (not her real name) had her first screening mammogram at the age of 46, and a spiculated
density was discovered in her medial left breast (Fig. 1). Ms. Connolly then acknowledged she was able to appreciate a palpable prominence in her medial breast and a “lump” in her left axilla. An ultrasound (Fig. 2)
disclosed a highly suspicious mass that measured 15 ¡Ñ 14 ¡Ñ 15 mm in the breast, and a left axillary mass that measured 35 ¡Ñ 29 ¡Ñ 14 mm.
Her primary care physician referred Ms. Connolly to a surgeon who specialized in breast surgery. In the office, the surgeon performed ultrasound-guided core biopsies of the tumor and the axillary mass. Pathologic examination of both lesions revealed a Grade III infiltrating ductal carcinoma, which was estrogen and progesterone receptor negative, and HER-2/neu positive. Ms. Connolly had a normal chest
x-ray and bone scan, but a PET scan revealed tumor isolated to the breast and axilla. An MRI confirmed
the presence of the malignancy in the left breast and the enlarged lymph node in the axilla; it also showed
no satellite lesions and a normal right breast (Figs. 3-5).
Based on Ms. Connolly’s aggressive and advanced breast cancer, the surgeon felt she should be considered for neoadjuvant chemotherapy. Ideally, the patient would receive immediate systemic therapy, followed by an assessment of response to this therapy. If the patient then chose breast conservation, this plan would improve her chances and the ultimate cosmetic result.
Ms. Connolly was referred to a medical oncologist and a radiotherapist, and her case was discussed at the
bi-monthly Breast Cancer Tumor Board. A course to include neo-adjuvant chemotherapy followed by surgery and postoperative radiation therapy was chosen. The oncologist treated Ms. Connolly with Adriamycin and Cytoxan followed by Taxol and Herceptin. She had a dramatic clinical response with resolution of all palpable disease. She was counseled by the surgeon and given the options of breast conserving lumpectomy or mastectomy. She chose mastectomy and, six months after her original
presentation, underwent a mastectomy with sentinel lymph node biopsy. The pathology examination found
no residual carcinoma in either the breast or lymph nodes. The patient plans to undergo breast reconstruction after completing her radiation therapy. She has tolerated her treatments with minimal side effects and no complications.
Figure 1: Screening film mammography in the mediolateral oblique
(MLO) and craniocaudad (CC) projection reveals the palpable mass
in the lower inner quadrant of the left breast. The enlarged lymph
node in the left axilla is partially imaged on the MLO view.
Figure 2: Ultrasound of the left breast reveals a solid mass at the
9 o’clock position of the left breast and an enlarged lymph node in the
left axilla.
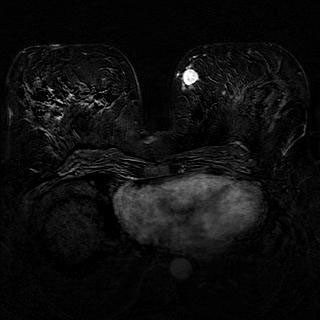
Figure 3: MRI in the axial plane shows the malignancy as an
enhancing lesion in the medial aspect of the left breast. (This is a 3D
Gradient Echo Subtracted MRI. The final image was obtained
by post-processing of contrast enhanced sequences, which results in
better delineation of abnormally enhanced lesions.)
Figure 4: MRI in the sagittal plane shows the enhanced malignancy
and a clip (black spot at tip of arrow) that was placed during the
previous ultrasound-guided core biopsy. (This is a Water Excitation
MRI, which uses a contrast enhanced sequence that shows optimal
detail of the internal architecture of the breast, and reveals how a
lesion affects the surrounding tissues.)
Figure 5: MRI in the axial plane reveals the enlarged lymph node in
the left axilla. (This is an Inversion Recovery MRI, which uses a
particular sequencing technique to detect adenopathy.)