Spring 2006 - Vol.1, No.1


COLORECTAL CANCER SCREENING:
HOW DOES CT COLONOGRAPHY FIT IN
BRUCE H. POKORNEY, M.D.
Chief Medical Officer, Sr. VP, Medical Affairs,
Lancaster General Hospital
Gastroenterologist
EDGAR C. FEARNOW, III, M.D.
Chief, Division of Computerized Tomography,
Lancaster General Hospital
Lancaster Radiology Associates, Ltd.
ABSTRACT
Colorectal cancer continues to be one of the leading causes of death in the United States. Despite the potential of screening methods to decrease mortality, screening rates among eligible individuals are abysmal. Conventional colonoscopy remains the gold standard for colorectal cancer screening, but poor patient compliance and negative attitudes toward this procedure may contribute to the low screening rates. CT colonography is more patient-friendly and may increase screening rates for colorectal cancer. Based on initial studies, it holds promise as a screening method, and may ultimately decrease mortality rates from colon cancer. However, CT colonography technique and technology must improve before the procedure can be widely adopted for screening. LGH physicians find that CT colonography is a helpful tool when optical colonoscopy is not feasible or successful, but should not be used for widespread screening of average risk individuals until further validation studies are completed.
DISCUSSION
Colorectal cancer remains the second most common cause of cancer death in the US, afflicting more than 145,000 people and killing more than 56,000 people each year. These bleak statistics persist despite reductions in the mortality rate during the last decade. Fortunately, screening methods can profoundly affect morbidity and mortality rates from colorectal cancer because it is a highly preventable and curable disease. The natural history of the disease, in which pre-malignant adenomatous polyps can take up to 10 years to develop into malignant ones, presents an ideal scenario for preventive screening to be effective by allowing identification and removal of pre-malignant polyps before cancer occurs.
For individuals with no other risk factors, who have an average cumulative risk of developing colorectal cancer of 6 percent, as well as for individuals with increased risk, conventional optical colonoscopy is still widely accepted as the best screening method. Despite the potential effectiveness of screening in reducing mortality, less than one-fourth of the eligible population in the US undergoes colorectal screening by any method. The low screening rate is the result of poor patient compliance, negative patient and physician attitudes toward screening, and, in particular, toward colonoscopy, and lack of trained colonoscopists to meet demand in some regions of the US. Optical colonoscopy, still considered the gold standard for screening because of its high sensitivity and specificity, has the distinct advantage of being the only screening method that can be used as both a diagnostic and a therapeutic tool. Nonetheless, optical colonoscopy is far from being the perfect screening method—it is expensive, invasive, resource-intensive, and has a small, but significant risk of complications. Many patients find that the bowel preparation required for the test is very uncomfortable. In addition, optical colonoscopy has limitations in that abnormalities, including small polyps or early cancers, may be missed at the hepatic and splenic flexures or in the cecum, where up to 20 percent and 15 percent of colorectal cancer occur, respectively.
Despite its limitations and disadvantages, initial colonoscopy for colorectal cancer screening has a higher benefit-cost ratio than any other screening test currently recommended for any disease. The technology used continues to advance, and developments, such as chromoendoscopy and fully digital high-resolution imaging, will eventually further improve its sensitivity and specificity.
CT colonography, or virtual colonoscopy, which has been in development for more than a decade, continues to show promise as a screening test for the future. The three-dimensional endoluminal view provides the radiologist with the ability not only to closely simulate the view obtained with conventional colonoscopy, but also to view the colon in countless other ways, including reverse and rotated views. One landmark study by Pickhardt et. al. reported that CT colonography has a sensitivity rate for detecting polyps 6 mm or larger nearly equal to, if not better than, optical colonoscopy. Further, CT colonography allows physicians to identify highly important extracolonic findings. Because it is not invasive, does not have a risk of complications, and does not require sedation or analgesia, and, therefore, has no patient recovery time, CT colonography has been touted as an attractive alternative to optical colonoscopy and a possible way to increase patient compliance.
Preparation for the procedure is basically the same as for conventional colonoscopy. At Lancaster General we use Fleet® Phospho-soda® Oral Saline Laxative, Bisacodyl tablets, and an enema. After a catheter is placed in the rectum, the colon is insufflated with 2 L of air, if it is tolerated. To determine if the colon is sufficiently distended, the radiologist turns the patient to the supine position and obtains a scout CT image. More air is added, if necessary. The radiologist then obtains 0.75 mm overlapping CT images of the patient, from the level of the diaphragm to the level of the perineum, in the supine and prone positions during a breathhold. The examinations are reviewed in two-dimensional multiplanar and three-dimensional endoluminal (fly-through) mode.
Figure 1: Virtual endoluminal view
is reconstructed by computer
processing to simulate a conventional
endoluminal view of the colon.
Why hasn’t CT colonography been adopted for widespread use in screening? First and most important, some studies comparing optical colonoscopy and CT colonography have reported a wide range in sensitivity and specificity of virtual colonoscopy. Differences in interpreter proficiency, imaging technique, and bowel preparation all contributed to the variation in results.
Only radiologists with a tremendous amount of experience - not only in general CT, but with the three-dimensional endoluminal view of the colon in particular, should be performing and reading CT colonography. Fortunately, radiologists at LGH have considerable experience with CT colonography. For optimum readability and patient comfort, thinner multi-slice CT scanners and three-dimensional software analysis packages are essential. At LGH, radiologists primarily perform examinations using a 16-slice scanner, and review examinations in both two-dimensional multiplanar and three-dimensional endoluminal modes.
Other disadvantages to CT colonography include the low to moderate exposure to radiation, which is not insignificant. Bowel preparation, considered the most unpleasant feature, is the same as for optical colonoscopy. Further, insufflation of the colon with air can often be uncomfortable for the patient. In some cases, distension of the colon can be suboptimal, making visualization of the colon in non-distended segments very difficult. The test is not reimbursed by insurance, unless the patient needs the procedure because of a failed conventional colonoscopy or is unable to undergo conventional colonoscopy. Although the potential cost may be low in the future, the out-of-pocket cost to the patient currently may be prohibitive.
Overall, although CT colonography is not yet a technique that is suitable for widespread screening of average risk individuals, it is helpful and, at times, essential in the management of patients in prevention, screening, and surveillance of colorectal cancer. Since CT colonography was first implemented at LGH in May 2005, it has been used only in the following circumstances: conventional colonoscopy has failed, which is very rare; colonoscopy is unable to view the colon proximal to an obstructing lesion or stricture; the patient cannot tolerate conventional colonoscopy or sedation, such as with elderly or frail patients; the patient should not have anticoagulant therapy discontinued; the patient refuses conventional colonoscopy for other reasons; or there are conditions present under which conventional colonoscopy is anticipated to be difficult or dangerous.
|
CURRENT LGH INDICATIONS FOR CT COLONOGRAPHY
-
Conventional colonoscopy has failed
-
Conventional colonoscopy is unable to view the colon proximal to obstructing lesion or stricture
-
Patient cannot tolerate conventional colonoscopy or sedation (e.g., elderly or frail patients)
-
Patient should not have anticoagulant therapy discontinued for conventional colonoscopy
-
Patient refuses conventional colonoscopy
-
Conditions are present that would make conventional colonoscopy difficult or dangerous
|
How would the widespread use of CT colonography affect the guidelines for patient care based on the size of polyps found on examination? Currently, the size and number of polyps found at initial screening is a significant factor in determining the next steps. Polyp size is often divided into three categories: 1 cm or larger, 6 to 9 mm, and 5 mm or smaller. For optical colonoscopy, all identified polyps, regardless of size, are immediately removed during the procedure. For CT colonography, patients would require immediate therapeutic colonoscopy for polyps 1 cm or larger. Many practitioners agree that polyps 5 mm or smaller are insignificant, and, if found by CT colonography, may be followed over time. The problem arises with polyps between 6 and 9 mm, a range in which the sensitivity and specificity of CT colonography can be more unpredictable and reader dependent.
Most physicians, including those radiologists and gastroenterologists who have developed the joint CT colonography guidelines at LGH, concur that 6 to 9 mm polyps found at CT colonography warrant colonoscopic removal. The situation becomes further complicated by the fact that differentiating between a 6 mm and 5 mm polyp using either optical colonoscopy or CT colonography is often difficult. Measurements within 1 mm are clearly subject to considerable operator or reader variability.
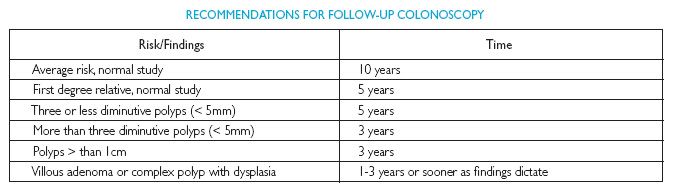
The size of polyps found on examination also affects patient followup. Patients with no polyps and no family history of polyps or colorectal cancer should return for followup screening in 10 years. Patients with no polyps, but who have a family history of cancer or complex polyps should return for another screening test in 5 years. Followup screening tests are recommended every 3 years for patients with adenomatous polyps 1 cm or larger, with a complex polyp, such as those showing dysplasia or a predominant villous pattern, or with three or more polyps that are 5 mm or smaller.

Many physicians cite an additional major obstacle in adopting CT colonography at their facilities—the potential “turf wars” between radiologists and gastroenterologists in implementing CT colonography. No doubt, the welfare of patients is enhanced if CT colonography is carried out with a high level of interaction and cooperation between radiologists and optical colonoscopists, particularly if polyps are found on CT colonography.
The close collaboration of gastroenterologists and radiologists at LGH provides an important model for interspecialty cooperation. The Department of Radiology and the Division of Gastroenterology worked collaboratively to define the current best uses for CT colonography from the patient’s perspective. Currently, a gastroenterologist must order the CT colonography, and the Department of Radiology can usually carry out the study on the same day a conventional colonoscopy has been attempted. Since the patient has already undergone colon preparation, a same day study is a great convenience for the patient. In the future, as the use of CT colonography increases, we hope that the reciprocal arrangement will also be feasible: if the findings of CT colonography require a followup colonoscopy for polyp removal, the Division of Gastroenterology will be able to accommodate patients on the same day they undergo primary CT colonography screening.
As the technology evolves even further, close collaboration between radiologists and gastroenterologists such as we have developed at LGH is essential to integrate CT colonography into the care plan for patients. Ultimately, the collaboration between both specialties has flourished because of the effort to place what is best for the patient as the highest priority, not what is best for the providers’ work processes or specialty.
The future of CT colonography in colorectal cancer screening remains dynamic. Software analysis packages continue to improve, shortening the procedure time for patients. Researchers have studied CT colonography using ultra-low dose radiation and found that a high sensitivity was maintained while the exposure to radiation was greatly reduced. Fecal tagging using iodinated contrast material may eventually eliminate the need for bowel preparation and greatly increase patient compliance.
Also, carbon dioxide can be used for colonic insufflation, making the procedure more tolerable for patients because it is more readily absorbed and more easily eliminated than air. As more data regarding the test’s sensitivity and specificity are published , and the method becomes more accepted by patients and physicians, CT colonography may become a more reasonable option for colorectal cancer screening in average risk patients. However, this prospect may only be realistic in facilities with a high degree of collaboration between CT colonographers and optical colonoscopists. We hope LGH will become a benchmark for such facilities.
REFERENCES
-
[1] Cappell MS. The pathophysiology, clinical presentation, and diagnosis of colon cancer and adenomatous polyps. Med Clin N Am 2005;89:1-42.
-
[2] Cotton PB, Durkalski VL, Pineau BC et al. Computed tomographic colonography (virtual colonoscopy): A multicenter comparison with standard colonoscopy for detection of colorectal neoplasia. JAMA 2004;291(14):1713-1719.
-
[3] Jemal A, Murray T, Ward E, et al. Cancer Statistics, 2005. CA Cancer J Clin 2005;55:10-30.
-
[4] Iannaccone R, Laghi A, Catalano C, et al. Detection of colorectal lesions: Lower-dose multi-detector row helical CT colonography compared with conventional colonoscopy. Radiology 2003;229:775-781.
-
[5] Lefkovtiz A, Shapiro R, Koch S, et al. The emerging role of virtual colonoscopy. Med Clin N Am 2005;89:111-138.
-
[6] Pickhardt PJ, Choi R, Hwang I, et al. Computed tomographic virtual colonoscopy to screen for colorectal neoplasia in asymptomatic adults. NEJM 2003;349(23):2191-2200.
-
[7] Schafer JM. Is virtual colonoscopy ready for your prime time? HONI 2005;Jan;3-6.
Bruce H. Pokorney, M.D.
Chief Medical Officer
Sr. VP, Medical Affairs, Lancaster General Hospital
Gastroenterologist
555 N. Duke Street
Lancaster, PA 17604
717-544-5145
Edgar C. Fearnow, III, M.D.
Chief, Division of Computerized Tomography,
Lancaster General Hospital
Lancaster Radiology Associates, Ltd.
P.O. Box 3555
Lancaster, PA 17604
717-544-4900