ABSTRACT
Gamma knife radiosurgery is a minimally invasive form of radiation therapy in which a high dose of stereotactically guided radiation is delivered to a specific target in the brain at a single setting.
We have performed 1,188 gamma knife procedures in 1,044 patients at the Lancaster General Hospital Gamma Knife Center over a 7-year period. Overall, patient outcomes have been excellent.
INTRODUCTION
Gamma knife radiosurgery is a minimally invasive, stereotactic radiation therapy used to treat multiple types of brain lesions (Figure 1). Treatable lesions include benign tumors such as meningiomas, pituitary adenomas, and acoustic neuromas; malignant tumors such as brain metastases, and high-grade gliomas; and conditions such as trigeminal neuralgia, and arteriovenous malformations of the brain.
The gamma knife uses an array of 201 sources of cobalt radiation which focus a high dose of radiation on a specific target area. Since adjacent normal brain tissue receives minimal amounts of radiation, the gamma knife offers several advantages over traditional open neurosurgery. Because it is minimally invasive, there is no risk of hemorrhage, spinal fluid leakage, or infection, and there is no risk of scarring or disfigurement. In most cases, the procedure is performed entirely on an outpatient basis (no hospital stay is required), and recovery time is minimal. Only local anesthesia and mild sedation are needed, which eliminates the risk of general anesthesia. Patients may resume their usual activities within one day of treatment.
Radiosurgery has other significant advantages over conventional fractionated radiation therapy. The most important appears to be more effective radiobiological action on the irradiated tissue by this high-dose, single-fraction radiation, which translates to better outcomes for lesions that respond poorly to conventional radiation therapy. The other obvious advantage is that the whole treatment takes place in one setting on a single day, thus avoiding 4 to 6 weeks of daily radiation treatments.
Worldwide, nearly 400,000 patients with vascular disorders, benign or malignant tumors, and functional and ocular disorders have been treated with the gamma knife. We report our experience with the gamma knife in 1,188 treatments in 1,044 patients over a 7-year period at the Lancaster General Hospital (LGH) Gamma Knife Center.
METHODS
The Procedure
Gamma knife radiosurgery is a multiple step procedure that requires a detailed treatment plan, which is developed and finalized immediately before the intervention. First, with the patient awake and under local anesthesia and mild sedation, the stereotactic frame is affixed to the patient’s head with 4-point fixation. Magnetic resonance imaging (MRI) is then performed to visualize and stereotactically localize the lesion. Using computer modeling, the lesion is identified and outlined, and a radiation dose is calculated. A plan is then developed to deliver radiation to the lesion while minimizing exposure of normal tissue. After completion of the treatment plan, the patient is moved to the gamma knife unit. The patient’s head is fixed to the gamma knife table, and the treatment plan is carried out. Once the radiation has been delivered, the head frame is removed, and the patient is discharged.
Patient Population
Between July 1999 and July 2006, 1,044 patients with a variety of brain lesions underwent a total of 1,188 gamma knife radiosurgery treatments at the LGH Gamma Knife Center. Patients were predominantly from Lancaster and surrounding counties. Individual patient data were recorded in an ongoing database.
LANCASTER GENERAL HOSPITAL EXPERIENCE
Benign Brain Tumors
We have treated 137 acoustic neuromas, benign tumors that grow from the acoustic-vestibular nerve. As the tumor expands, hearing loss, dizziness, tinnitus, and problems with balance may ensue. In 136 patients, gamma knife radiosurgery either halted tumor growth or induced regression. One patient experienced postinterventional tumor enlargement, and subsequently required microneurosurgical removal.
218 patients with a meningioma have undergone gamma knife radiosurgery, and tumor growth was arrested in 95%. Postprocedural tumor growth that caused significant brain swelling occurred in 3 patients, and surgical intervention was required.
We have also treated recurrent and residual benign pituitary tumors with the gamma knife. Though the treatment of choice is transsphenoidal removal, the gamma knife is indicated in patients with recurrent and residual tumors, and in patients whose tumor extends laterally into the cavernous sinus area, because surgical excision in this latter group is not feasible. Of the 47 patients with pituitary tumors treated at LGH, tumor growth was halted in 46.
Malignant Brain Tumors
Metastatic tumors are the most common malignant brain tumors treated with gamma knife radiosurgery (Figure 2). The primary sources of most cancers that metastasize to the brain are lung, breast, kidney, and melanoma, although any type of malignancy may spread to the brain. Single and multiple brain metastases are treatable with the gamma knife, but we generally limit treatment to patients with fewer than 5 metastatic tumors. Many patients with brain metastases require repeat gamma knife treatment as they develop new tumors.
To date, 350 patients with a variety of metastatic tumors have undergone gamma knife radiosurgery at LGH. Outcomes in this population are measured by our ability to control progression of the brain metastases. Excellent results—tumor progression slowed or halted—were observed in 70% to 80% of patients (Figure 3). Unfortunately, most patients with metastatic cancer eventually succumb to the primary cancer, but gamma knife radiosurgery may prolong survival and significantly improve the quality of life.
We treated 78 patients with primary brain tumors, mainly high-grade gliomas, with the gamma knife. In these ominous lesions, the gamma knife is used to boost external beam radiation, and the benefits in this group of patients are limited.
Trigeminal Neuralgia
Trigeminal neuralgia is a disorder of the trigeminal nerve—the fifth and largest cranial nerve - that causes periodic episodes of intense, acute facial pain most often near the nose, lips or eyes. Medical intervention with agents such as carbamazepine, gabapentin, and baclofen are the primary treatments of choice, but if these treatments fail, patients are eligible for gamma knife radiosurgery. The gamma knife can deliver a high dose of radiation directly to the nerve, which often alleviates pain.
We have treated 193 patients with trigeminal neuralgia; facial pain resolved in approximately 55% of our patients, and 25% improved within 3 weeks to 3 months of treatment. Although transient or permanent facial numbness occurred in about 10% of patients, Trigeminal neuralgia is so painful that most patients willingly accept this risk. Patients with recurrent pain may undergo repeat gamma knife Radiosurgery, and approximately 60% of patients in this population ultimately achieved resolution of their pain.
Arteriovenous Malformations of the Brain
Two types of arteriovenous malformations of the brain can be treated with gamma knife radiosurgery: true arteriovenous malformations and cavernous angiomas. The former is characterized by a high-flow arteriovenous fistula with a large conglomeration of abnormal blood vessels that connect directly from the arterial to the venous side of the circulation. These patients are at risk for intracranial hemorrhage. Patients with cavernous angiomas have a lower bleeding risk, but if they have a documented history of cerebral hemorrhage, treatment is warranted.
Gamma knife radiosurgery tends to obliterate true arteriovenous malformations within 2 to 3 years of treatment. We treated 22 patients with true arteriovenous malformations, and 14 patients with cavernous angiomas. The results have been excellent, and no patient has suffered a recurrent hemorrhage (Figures 4 and 5).
SAFETY & COMPLICATIONS
Side effects of radiosurgery may be acute (within the first few days post treatment), delayed (months later), or chronic (longer than a year after treatment). Acute effects include seizures, headaches, vomiting, and dizziness, which are short lasting and usually resolve completely. Delayed complications are due to cerebral edema which may or may not lead to neurological deficits. Chronic side effects include radionecrosis or death of adjacent brain tissue. The risk of developing a radiation induced neoplasm in the brain following radiosurgery has been estimated to be less than 1/10,000.
Our own experience has been very favorable with less than 2% of patients suffering significant complications. The few patients with radiation edema/necrosis have responded well to steroid therapy. We have observed no cases of radiation induced tumors, and hair loss is uncommon. Loss of cognitive function, which sometimes occurs with whole brain radiation, is not typically seen with gamma knife radiosurgery.
DISCUSSION
Overall, our experience at LGH compares favorably with the experiences reported in the literature by other major centers. Moreover, gamma knife radiosurgery compares favorably with other treatment options, particularly neurosurgical intervention. For example, a 2006 study compared gamma knife surgery with surgical resection in 82 patients with vestibular schwannomas (acoustic neuromas).1 Although there was no difference in tumor control between treatments, preservation of serviceable hearing and facial nerve function was significantly more common with radiosurgery than surgical resection after 3 months (P<0.001), 1-year (P<0.001), and 42-months (P<0.01). Surgical resection was associated with a significant loss of physical function, as well as persistent pain at 3-month and 1-year follow-up. Conversely, patients who underwent radiosurgery experienced no decline in physical function, and also had lower dizziness handicap scores (P=0.02). The investigators concluded that radiosurgery is the preferred treatment for acoustic neuromas.
Such conclusions are supported by long-term follow-up data.2 Hasegawa and colleagues recently reported outcomes at a median of 7.8 years in 301 patients who underwent radiosurgery. Tumor growth was stopped in 93% of patients. The treatment failed in 7%. Hearing was preserved in 68% of patients. Transient facial palsy and facial numbness occurred in 1% and 2% of patients, respectively. Other investigators have reported similar long-term outcomes, as well.3 Such findings are consistent with those observed at LGH.
Like the treatment of acoustic neuromas, gamma knife radiosurgery appears safe and effective for the management of trigeminal neuralgia. Regis and co-workers4 recently reported that 83 of 100 treated patients were pain free 12 months after therapy. All quality of life parameters were significantly improved in these patients (P<0.001), and 58 stopped taking medication during the follow-up period. Mild facial paresthesia and hypesthesia were reported by 6 and 4 patients, respectively.
Similar long-term outcomes (median 49 months) were observed by McNatt and colleagues.5 In their study of 49 patients, 61% with trigeminal neuralgia experienced excellent pain relief by the last follow-up visit. Recurrent pain after a period of relief (mean 9.6 months) was reported by 23%. Mild to moderate facial numbness and dysesthesia were reported by 29% and 18% of patients, respectively. Gamma knife surgery produced symptomatic improvement in the majority, and complete cure in a notable proportion.
Data on the treatment of cerebral metastases and primary gliomas are mixed. Some investigators have reported arresting disease progression and prolonging survival in cases of brain metastases with radiosurgery alone.6-8 Others have noted equivocal outcomes as well as higher recurrence rates with radiosurgery alone, and they propose combining gamma knife therapy with whole-brain radiation therapy.9-11 Some data suggest that radiosurgery provides a needed boost to other forms of radiation therapy. In our experience, gamma knife radiosurgery was associated with significant benefit in patients with metastatic tumors, and limited benefit in patients with high-grade gliomas.
CONCLUSIONS
Gamma knife radiosurgery is a noninvasive technology useful in the management of multiple types of cerebral lesions. It is safe, and, in many conditions, highly efficacious. At LGH, we have treated more than 1,000 patients with a variety of brain lesions, and results have been excellent in the majority. Use of the gamma knife is expanding, and, in addition to the conditions treated at LGH, the technology may have a future role in the management of epilepsy and Parkinson’s disease.
REFERENCES
- Pollock, BE, Discoll, CL, Foote, RL, et al. Patient outcomes after vestibular schwannoma management: a prospective comparison of microsurgical resection and stereotactic radiosurgery. Neurosurgery 2006;59:77-85.
- Hasegawa, T, Fujitani, S, Katsumata, S, Kida, Y, Yoshimoto, M, Koike, J. Stereotactic radiosurgery for vestibular schwannomas: analysis of 317 patients followed more than 5 years. Neurosurgery 2005;57:257-65.
- Chan, AW, Black, P, Ojeman, EG, et al. Stereotactic radiotherapy for vestibular schwannomas: favorable outcome with minimal toxicity. Neurosurgery 2005;57:60-70.
- Regis, J, Metellus, P, Hayaski, M, Roussel, P, Donnet, A, Bille-Turc, F. Prospective controlled trial of gamma knife surgery for essential trigeminal neuralgia. J Neurosurg 2006;104:913-24.
- McNatt, SA, Yu, C, Giannotta, SL, et al. Gamma knife radiosurgery for trigeminal neuralgia. Neurosurgery 2005;56:1295-301.
- Jawahar, A, Willis, BK, Smith, DR, Ampil, F, Datta, R, Nanda, A. Stereotact Funct Neurosurg 2002;79:262-71.
- Koc, M, McGregor, J, Grecula, J, Bauer, CJ, Gupta, N, Gahbauer, RA. Gamma knife radiosurgery for intracranial metastatic melanoma: an analysis of survival and prognostic factors. J Neurooncol 2005;71:307-313.
- Maucevic, A, Kreth, FW, Tonn, JC, Wowra, B. Stereotactic radiosurgery for multiple brain metastases from breast carcinoma. Cancer 2004;100:1705-11.
- Aoyama, H. Shirato, H, Tago, et al. Stereotactic radiosurgery plus whole-brain radiation therapy vs. stereotactic radiosurgery alone for treatment of brain metastases: a randomized controlled trial. JAMA 2006; 295:2483-91.
- Manon, R, O’Neill, A, Knisely, J, et al. Phase II trial of radiosurgery for one to three newly diagnosed brain metastases from renal cell carcinoma, melanoma, and sarcoma: an Eastern Cooperative Oncology Group study (E 6397). J Clin Oncol 2005;23:8870-6.
- Cho, KH, Hall, WA, Lo, SS, Dusenbury, KE. Stereotactic radiosurgery versus fractionated stereotactic radiotherapy boost for patients with glioblastoma multiforme. Techol Cancer Res Treat 2004;3:41-9.
Eddy Garrido, M.D., Lancaster Neuroscience & Spine Associates
1617 Crooked Oak Drive, Lancaster, PA 17601
717-569-1240
Egarrido@redrose.net
Kenneth Berkenstock, M.D., Lancaster Radiology Associates, Ltd.
2100 Harrisburg Pike, Lancaster, PA 17604
717-544-3113
kgberken@LGHealth.org
Charles Fuller, Ph.D., D.A.B.R. Medical Physicist, Lancaster General Cancer Center
2102 Harrisburg Pike, Lancaster, PA 17604
717-544-3113 Ext. 88853
cifuller@LGHealth.org
Christine Burfete, R.N., B.S.N., Gamma Knife Nurse, Lancaster General Hospital
2102 Harrisburg Pike, Lancaster, PA 17604
717-544-3065
ceburfet@LGHealth.org
FIGURE LEGENDS
Figure 1. The gamma knife machine with a treatment-ready patient.

Figure 2. Left frontal lobe metastasis renal cell carcinoma prior to gamma knife radiosurgery.

Figure 3. Following gamma knife radiosurgery, the left frontal lobe metastasis resolved.

Figure 4. Left parietal lobe arteriovenous malformation prior to gamma knife radiosurgery.
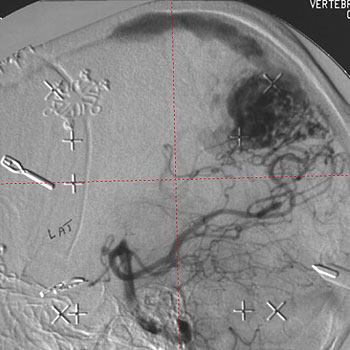
Figure 5. Four years following gamma knife radiosurgery, the arteriovenous malformation had completely resolved.
