 Click to Print Adobe PDF
Click to Print Adobe PDF
Fall 2007 - Vol.2, No.3
Leigh S. Shuman, M.D.
Staff Radiologist, Lancaster General Hospital
Lancaster Radiology Associates, Ltd.
|
 |
Clinical Setting: For patients with pancreatic cancer and other abdominal malignancies, debilitating pain can significantly reduce their quality of life, particularly since their lifespan is typically measured in months. Although medical management of pain is successful in the majority of patients, some patients experience side effects from pain medications that reduce their ability to function and remain alert. 10-20% of patients may not achieve adequate pain control from medical therapy alone, which provides a role for interventional techniques that can effectively control visceral pain while reducing the need for medication. With our colleagues in anesthesia, we have treated a number of these patients with image-guided celiac plexus block.
Anatomy and Physiology: Pain from the pancreas and adjacent structures travels to the central nervous system by way of the celiac plexus, a group of 1-4 ganglia that lie just below the aortic origin of the celiac artery and just anterior to the aorta. Blockade of this plexus has been described for decades in the anesthesia literature, either blindly using dead reckoning, or with fluoroscopy to identify landmarks based on the spine and the expected location of the aorta and celiac artery relative to bony structures. Long-acting local anesthetics have been tried, but their effect is not durable enough; prolonged relief of pain requires neurolysis, typically with either alcohol or phenol. Both of these agents are potent destroyers of any tissue they contact, which makes accurate delivery critical to achieving success and avoiding complications.
Technique: The original technique uses fluoroscopic guidance and a posterior paraspinous approach. This technique is still used on selected patients by several of our pain specialists. With the advent of cross-sectional imaging, more precise ways to deliver a neurolytic agent to the celiac plexus have been developed. Techniques have been described that use computed tomography (CT), ultrasound, or MRI for guidance, along with endoscopic ultrasound.
We have used computed tomography in 5 patients. As noted, a variety of imaging modalities have been described, and both anterior (Fig 1) and posterior (Fig 2) approaches have been utilized. While ultrasound is rapid, real-time, and relatively inexpensive, accurate needle position can be difficult to confirm depending on bowel gas and body habitus. CT, however, allows precise localization of the needle, and confirms that the agent is going to the intended location. We prefer the anterior approach for image-guided therapy, since it allows the patient to lie supine, which is typically more comfortable and permits easier monitoring and airway management.
The procedure is generally done on an outpatient basis. Since the injection of alcohol can be quite painful, our anesthesia colleagues administer deep conscious sedation with Propofol. The anterior abdominal wall is cleansed and anesthetized, and the interventional radiologist inserts a 22-guage Chiba needle to a location just anterior to the abdominal aorta, and just above the celiac axis. This is generally very easy to identify with CT, even without IV contrast. Although the ganglia lie just below the origin of the celiac artery, placement of the needle just above the artery avoids the numerous visceral branches, and the origin of the Superior Mesenteric Artery which is just below. Sufficient agent is injected to spread to the celiac plexus. (The needle is small enough to traverse the stomach, colon, and liver with a very high degree of safety.)
When the needle is in place, 5-10 cc of local anesthetic and dilute contrast are injected first to confirm the spread of fluid along the anterior wall of the aorta (Fig 2). The local anesthetic minimizes the pain of the alcohol injection, but does not serve as a “test” since there is a poor correlation between rapid response to local anesthesia and a sustained response to neurolysis. If the needle is in proper position, 30-40cc of absolute ethanol is injected, the needle is flushed with saline, and removed. Patients are then transferred to the Post-Anesthesia Care Unit for monitoring and pain management. Up to 30% of patients experience transient hypotension related to sympathetic blockade, which responds to volume expansion. Some experience substantial pain from the alcohol, which generally resolves in a few hours. Once discharged, the patients return to their oncologist for adjustment of oral pain medications.
Results: Four of the five patients we have treated have experienced substantial pain relief and have required less oral analgesia. The response lasted until the patients died, typically several months later. The one non-responder had extensive post-operative and post-radiation scarring in the pre-aortic space, as well as extensive tumor invasion. This situation has been well described as a cause of failure, because the alcohol cannot spread effectively.
Aside from one failure to relieve pain, we have had no other major complications. With fluoroscopic guidance alone, neurological injury, including paraplegia, has been reported. These complications should be very rare with the anterior image-guided approach, since the spinal artery and cord are well away from the injection site.
Conclusions: We have found that working together with our anesthesia colleagues in pain management, we can offer substantial improvement in the end-of-life experience for some of the most challenging cancer patients.
REFERENCES
- Titton RL, Lucey BC, Gervais DA, et al. Celiac Plexus Block. AJR 2002;179:633-636
- Akhan O, Ozmen MN, Basgun N, et al. Long-Term Results of Celiac Ganglia Block. AJR 2004;182:891-896
Leigh S. Shuman, M.D.
Staff Radiologist, Lancaster General Hospital
Lancaster Radiology Associates, Ltd.
P.O. Box 3555
Lancaster, PA 17604
717-544-4900
LSShuman@LGHealth.org
Figure 1. Posterior approach to celiac ganglion block. Contrast can be seen spreading in front of the abdominal aorta.
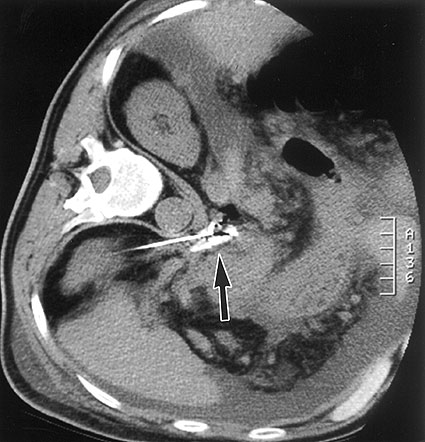
|
(Reprinted with permission from the American Journal of Roentgenology. Titton RL et al., AJR 2002;179:633-636)
|
Figure 2. Anterior approach to the celiac plexus, our preferred method. Contrast injection confirms spread of fluid in front of the aorta and celiac artery.
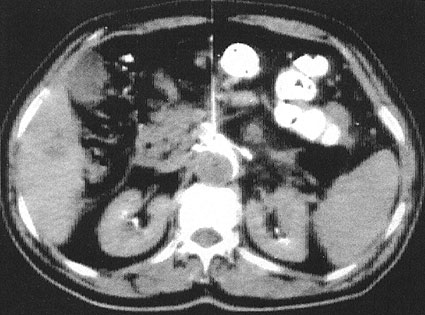
(Reprinted with permission from the American Journal of Roentgenology. Akhan O et al., AJR 2004;182:891-896)