Summer 2023 - Vol. 18, No. 2
SCIENTIFIC REPORT
Emerging Tickborne Diseases in Pennsylvania
A Case Discussion and Summary of a
Department of Health Advisory
Pratiti Roy, MD
Family Physician, Family Medicine Residency Program
Penn Medicine Lancaster General Health
In August, a 55-year-old woman presents to your Lancaster County clinic complaining of fever, diffuse joint pain, and chills. She started having these symptoms yesterday. She denies shortness of breath, chest pain, or rash. She is an avid hiker who claims she scrupulously checks herself for ticks after every outdoor excursion and has not noted any bug bites recently. She is otherwise healthy and up to date on all her preventive care. At home she has had temperatures up to 103°F. In your office, her vitals are normal. Her exam is otherwise unremarkable. You order a complete blood count, comprehensive metabolic panel, and Lyme panel. Her results come back showing a mild leukopenia and slightly elevated transaminases. Her Lyme testing is negative.
EMERGING TICKBORNE ILLNESSES
Borrelia miyamotoi infection is also known as hard tick relapsing fever.1 The bacteria implicated here is closely related to Borrelia burgdorferi, the pathogen that causes Lyme disease, and is spread by the same vector, Ixodes scapularis — commonly known as the blacklegged tick or deer tick. The Pennsylvania Department of Health recently issued an advisory warning about an increase in B. miyamotoi infections2 in the state after researchers reported that 1% of adult deer ticks in the state are carriers of B. miyamotoi.
Like B. burgdorferi infections, B. miyamotoi infections are spread through a tick bite. However, while B. burgdorferi transmission requires a tick be attached for between 36-48 hours to transmit the infection, B. miyamotoi can be transmitted within 24 hours of attachment.3 In addition, while B. burgdorferi is transmitted to a tick while feeding from an infected host, B. miyamotoi can spread via vertical transmission from mother to egg, which means a larva that has not yet fed can potentially spread the disease.3 Thus, while B. burgdorferi tends to spread throughout the spring and summer, B. miyamotoi infections peak in July/August, when larvae are most prevalent1 (see Fig. 1). These tick larvae are incredibly small — the size of a poppy seed (see Fig. 2) — which makes them difficult to detect.
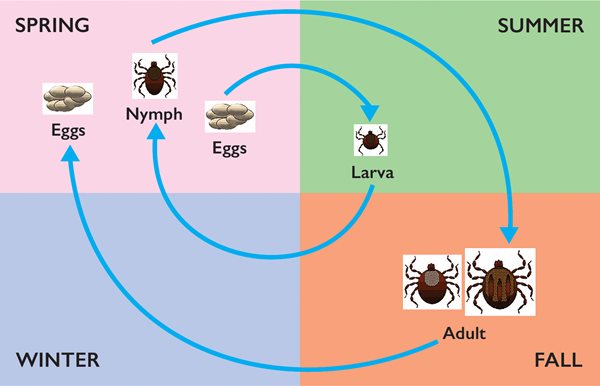
Fig. 1. The lifecycle of a tick, showing larvae most prevalent in summer. Adapted from CDC sources.
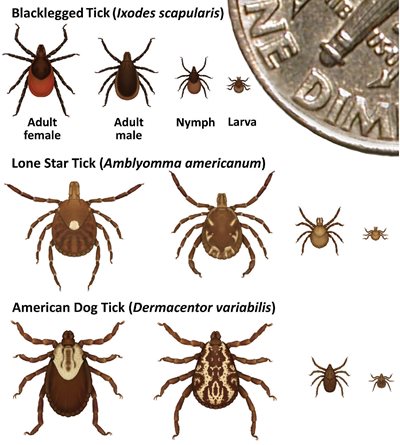
Fig. 2. Though the actual size of tick larvae is incredibly small, this figure is enlarged to show markings and stages of common tick species. Figure from cdc.gov/ticks/life_cycle_and_hosts.html.
Patients infected with B. miyamotoi also present in a way that is unique from patients who are infected with B. burgdorferi. Usually, patients with B. miyamotoi will complain of fever accompanied by arthralgias, headache, chills, and fatigue. Gastrointestinal symptoms, rash, and dyspnea are much less common than in patients with B. burgdorferi infection. Common lab findings in a patient with B. miyamotoi infection include leukopenia, thrombocytopenia, and elevated transaminases.2 Notably, in an immunocompetent patient, symptoms tend to be milder and more self-limited; there also does not tend to be relapse of the fever or any other chronic symptoms. In an immunocompromised patient, there is the potential for central nervous system involvement, although this is not commonly seen.3
Commercial testing is available, but it is separate from standard tickborne illness panels. At Penn Medicine Lancaster General Health, the test is available as a send-out polymerase chain reaction (PCR) test that can take days to weeks to come back. The recommended treatment in patients with B. miyamotoi is two to four weeks of doxycycline.2 In pediatric and pregnant patients, amoxicillin is an appropriate alternative.3 Improvement should be noted within 72 hours; the Jarisch-Herxheimer reaction is a possibility. While post-exposure prophylaxis is available to prevent B. burgdorferi infection, this has not been shown to be useful against B. miyamotoi.
The literature does not provide guidelines on whether clinicians should treat empirically or wait for test results. On the one hand, the test results can take so long to return that waiting for a result could potentially delay treatment by weeks. In addition, Ixodes can carry multiple pathogens, thus co-infection is a concern in treating any tickborne illness.4 The benefit of doxycycline is that it treats not only Borrelia infections, but it also treats anaplasmosis, a common co-infection in Ixodes ticks.4 However, it is also worth noting that in many immunocompetent patients, this appears to be a self-limited illness without known long-term repercussions. An analysis of serum samples of people living in New England found that 5% to 10% of participants had a prior infection with B. miyamotoi with minimal to no symptoms and thus had never sought or received treatment with no long-term consequences.5 In the absence of clear recommendations, treating empirically seems like the safer option; shared decision-making should be employed.
The Pennsylvania Department of Health advisory also includes updates on two other tickborne diseases: Heartland virus and Spotted fever rickettsiosis. These two diseases were previously unheard of in Pennsylvania, as their vectors — the lone star tick and the gulf coast tick, respectively — could not be found here. However, due to climate change, there has been northward expansion of these ticks’ range,6 and it is valuable to be aware of the diseases these ticks carry.
A patient infected with the Heartland virus, spread by the lone star tick, can present with fever, fatigue, anorexia, nausea/vomiting, diarrhea, and/or headache. Treatment consists of supportive care. Lab results will show leukopenia, thrombocytopenia, and elevated transaminases. Testing for Heartland virus is available by coordination with the Centers for Disease Control and Prevention (CDC). In Pennsylvania, clinicians should contact the Pennsylvania Department of Health for help. A lone star tick in southeastern Pennsylvania has been found to have Heartland virus, but thus far there have been no cases of human infection in the Commonwealth.2
Spotted fever rickettsiosis is caused by the bacteria Rickettsia parkeri, a bacteria related to Rickettsia rickettsia, which causes Rocky Mountain Spotted Fever (RMSF). R. parkeri is spread by the gulf coast tick, which was first found in Pennsylvania in 2022. The illness course of Spotted fever rickettsiosis tends to be less severe than RMSF, but the presenting symptoms are similar: maculopapular rash (see Fig. 3), fever, headaches, and myalgias.

Fig. 3. Rocky Mountain Spotted Fever rash. Photo from cdc.gov/dotw/rmsf/index.html.
One distinguishing factor is the presence of an inoculation eschar (see Fig. 4) — a necrotic lesion that forms around the site of the tick bite. This eschar is generally not present in RMSF.

Fig. 4. Spotted fever rickettsiosis eschar. Photo from cdc.gov/otherspottedfever/healthcare-providers/index.html.
Like RMSF, if there is suspicion for Spotted fever rickettsiosis, it is best to start treatment with doxycycline empirically (100 mg twice daily for five to seven days in adults). While commercially available PCR testing for RMSF exists, testing for R. parkeri can only be done through coordination with the CDC, with assistance from the Pennsylvania Department of Health.2
CASE DISCUSSION
To return to our initial case of presumed tickborne infection, testing this patient reveals she is positive for B. miyamotoi. Treatment with doxycycline is initiated, and she completes two weeks without missing any doses. Your patient’s symptoms resolve, and at her follow-up she is fully recovered and states she will be more liberal with bug spray when she goes hiking.
As a clinician, it can be challenging to stay up to date on tickborne diseases. Climate change is creating warmer and more humid conditions that allow both for northward creep of ticks that used to have a more southern range and for increased activity in those areas where ticks are endemic.7 We are living in a world where the incidence of diseases like Lyme disease and RMSF are increasing alongside emerging tickborne infections that we are just starting to understand. Both the CDC and the Pennsylvania Department of Health have helpful guidelines on diagnosis and management of tickborne diseases; they are updated frequently.3,8
REFERENCES
1. Hard Tick Relapsing Fever. Centers for Disease Control and Prevention. August 5, 2022. Accessed April 12, 2023. https://www.cdc.gov/ticks/tickbornediseases/hard-tick-relapsing-fever.html
2. Emerging Tickborne Diseases in Pennsylvania. Pennsylvania Department of Health. August 26, 2022. Accessed April 10, 2023. https://www.health.pa.gov/topics/Documents/HAN/2022-658-8-26-ADV-Tickborne.pdf
3. Department of Health and Human Services, Centers for Disease Control and Prevention. Tickborne Diseases of the United States: A Reference Manual for Health Care Providers. 2022. Accessed April 27, 2023. https://www.cdc.gov/ticks/tickbornediseases/TickborneDiseases-P.pdf
4. Swanson SJ, Neitzel D, Reed KD, et al. Coinfections acquired from ixodes ticks. Clin Microbiol Rev. 2006;19(4):708-727.
5. Krause PJ, Narasimhan S, Wormser GP, et al. Borrelia miyamotoi sensu lato seroreactivity and seroprevalence in the northeastern United States. Emerg Infect Dis. 2014;20(7):1183-1190.
6. Stafford KC, Molaei G, Little EAH, et al. Distribution and establishment of the lone star tick in Connecticut and implications for range expansion and public health. J Med Entomology. 2018;55(6):1561-1568.
7. U.S. Global Change Research Program. Chapter 5: Vector-borne diseases. In: Crimmins A, Balbus J, Gamble JL, et al., eds. The Impacts of Climate Change on Human Health in the United States: A Scientific Assessment. 2016. Accessed April 14, 2023. https://health2016.globalchange.gov
8. Lyme Disease and Other Tickborne Diseases in Pennsylvania. Pennsylvania Department of Health. April 13, 2023. Accessed April 27, 2023. https://www.health.pa.gov/topics/Documents/HAN/2023-690-4-13-Lyme.pdf