 Click to Print Adobe PDF
Click to Print Adobe PDF
Spring 2010 - Vol.5, No.1
THE LANCASTER GENERAL RESPONSE TO THE EPIDEMIC OF OBESITY
Alice M. Yoder, MSM, RN
Director of Community Health
|
 |
Advances in science have led to a steady increase in life expectancy over the past thousand years, yet this trend is projected to come to a halt due to one factor – obesity. In this as in so many other health issues, Lancaster General Health must go beyond the walls of the hospital and into the community in order to effectively execute our mission: “to improve the health and well being of the communities we serve
To identify the greatest needs and to measure our impact, we compile and analyze multiple data sources in partnership with various community organizations. These data consist of:
- morbidity
- mortality
- survey of youth risk factors
- Center for Disease Control Adult Behavioral Risk Factor Survey
- health system data,
- minority focus group reports.
Outliers are identified from county and state comparison data and trends. The data are analyzed and a comprehensive criteria tool leads to the selection of priority areas for community health improvement. Criteria guidelines include identifying the scope and seriousness of the problem, and its effect on the community. Through this process it has become clear that prevention of obesity needs to be the primary focus. Seven of the top ten leading causes of death in Lancaster County are related to obesity.
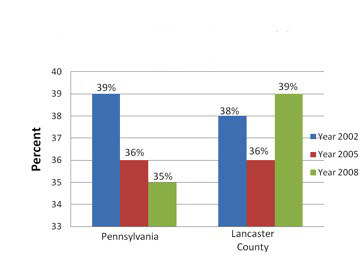
61% of adults in Lancaster County are overweight or obese and 16% of youth have a BMI >18. (Figures 1 & 2 – children’s figure not included) Though diabetes is also very common, a focus on diabetes would only be applying a Band-Aid and would not address the root cause. As a society, we have dramatically altered the way we live, work, eat, and play, and we have created an environment that fuels the obesity epidemic.
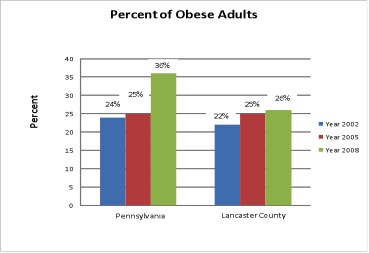
Figure 1 and 2. Lancaster Behavioral Risk Factor Survey 2008; PA Department of Health EpiQMS System (Data provided by the Bureau of Health Statistics and Research, Pennsylvania Department of Health. The Department specifically disclaims responsibility for any analyses, interpretations or conclusions.)
Lancaster General utilizes the socio-ecological model as a framework to develop healthy weight management initiatives. Research shows that consistent policies and education throughout each of the shared environments heightens public awareness, influences policy, challenges beliefs, and ultimately leads to increased knowledge and behavioral changes.
A comprehensive approach has been developed which consists of interventions at the provider, school, individual, interpersonal, and policy level. But there is only so much that one organization can do by itself.It will take many sectors of the community to impact obesity. The Lighten up Lancaster County Coalition serves as the forum for collaboration to address this issue in our community. The coalition has set goals and developed a strategic plan that they hope will stabilize obesity rates and begin to decrease them by 2015. The Logic Model is the framework used to organize the Coalition’s work and progress. A logic model displays the sequence of actions that describe what the program is and will do – how investments link to results. It is used in planning, implementation, evaluation and communication. The core components of a logic model are:
1. INPUTS: resources, contributions, investments that go into the program
2. OUTPUTS: activities, services, events and products that reach people who participate or who are targeted.
3,4,5. OUTCOMES (Short, Intermediate, and Long-term): results or changes for individuals, groups, communities, organizations, communities, or systems.
Lancaster General Current Initiatives
Lancaster General Health’s strategic approach to Healthy Weight Management is planned using national, state and local data and engages community stakeholders to provide evidenced-based programs. The Healthy Weight Management model provides a systematic and visual framework to view the relationships between our resources, our program activities and the measurable impact they have on our community. The socio-ecological model for health depicted on this page integrates those program activities throughout the shared environment.
A comprehensive program of strategies would include:
Healthy Eating:
- Create incentive programs to attract supermarkets and grocery stores to underserved neighborhoods;
- Require menu labeling in chain restaurants to provide consumers with calorie information on in-store menus and menu boards;
- Mandate and implement strong nutrition standards for foods and beverages available in government-run or regulated after-school programs, recreation centers, parks, and child-care facilities, including limiting access to unhealthy foods and beverages;
- Adopt building codes to require access to and maintenance of, fresh drinking water fountains (e.g. public restrooms).
- Implement a tax strategy to discourage consumption of foods and beverages that have minimal nutritional value, such as sugar sweetened beverages.
- Develop media campaigns, utilizing multiple channels (print, radio, internet, television, social networking and other promotional materials) to promote healthy eating (and active living) using consistent messages.
Physical Activity Strategies:
- Plan, build and maintain a network of sidewalks and street crossings that connects to schools, parks and other destinations and create a safe and comfortable walking environment;
- Adopt community policing strategies that improve safety and security of streets and park use, especially in higher-crime neighborhoods;
- Collaborate with schools to implement a Safe Routes to Schools program’
- Build and maintain parks and playgrounds that are safe and attractive for playing, and in close proximity to residential areas;
- Collaborate with school districts and other organizations to establish agreements that would allow playing fields, playgrounds, and recreation centers to be used by community residents when schools are closed (joint-use agreements); and
- Institute regulatory policies mandating minimum play space, physical equipment and duration of play in preschool, afterschool and child-care programs.
THE ROLE OF THE PHYSICIAN
Active involvement by the medical practitioner is crucial to success. Doctors need to continue to be active in their communities promoting prevention as a policy focus in different areas of public health. Physicians are the ones who have been able to encourage concerted actions, to influence policy makers, and often to become policy makers. Physician involvement is necessary for medical assessment and coordination of multidisciplinary obesity treatment. Obese patients who receive counseling and weight management from physicians are more likely to succeed in intervention programs.
CONCLUSIONS
As a health system we could continue to build more cardiac catherization labs to treat heart disease or build more operating rooms to replace joints that deteriorate prematurely because they have experienced too much weight, but these interventions are all expensive band-aids and are not financially sustainable in the future models of health care. We must focus upstream and identify root causes to address the obesity epidemic and begin to reverse this epidemic by implementing multi-faceted strategies at the individual, family, community, and provider levels.